Abstract
Purpose
This study aimed to compare the safety and efficacy of tamsulosin and tadalafil as medical expulsive therapy for distal ureteral stones.
Materials and Methods
This prospective randomized study was conducted at the Department of Urology of Bir Hospital over a period of 12 months in patients with distal ureteral stones sized 5 to 10 mm. Patients were randomly divided into 2 groups: group A received tamsulosin 0.4 mg and group B received tadalafil 10 mg at bedtime for 2 weeks. Stone expulsion rate, number of ureteric colic episodes and pain score, analgesic requirements, and adverse drug effects were noted in both groups. Statistical analyses were performed by using Student t-test and chi-square test.
Results
Altogether 85 patients, 41 in group A and 44 in group B, were enrolled in the study. The patients' average age was 31.72±12.63 years, and the male-to-female ratio was 1.5:1. Demographic profiles, stone size, and baseline investigations were comparable between the 2 groups. The stone expulsion rate was significantly higher in the tadalafil group than in the tamsulosin group (84.1% vs. 61.0%, p=0.017). Although the occurrence of side effects was higher with tadalafil, this difference was not significant (p=0.099). There were no serious adverse effects.
Urolithiasis is one of the most common diseases of the urinary tract. The lifetime prevalence of urinary stones is around 1% to 15%, and the peak age of incidence is at 30 years. Men are affected 2 to 3 times more often than women [1]. Ureteral stones account for 20% of the calculi in urolithiasis and about 70% of ureteral stones are present in the distal third of the ureter at the time of presentation [2].
Ureteral stones induce ureteral spasms that interfere with stone expulsion. Thus, reducing these spasms while maintaining normal peristaltic activity can facilitate stone expulsion. Almost 50% of ureteral stones will pass spontaneously over time and stone size is the key factor for success. Usually, stones smaller than 5 mm are expected to pass spontaneously, whereas only 20% of stones larger than 8 mm will pass [3]. Improvements in minimally invasive procedures in the last few decades have considerably changed the treatment of ureteral stones, but such procedures are not free of risks and are costly as well. A conservative approach through medical expulsive therapy (MET) has now become an established treatment modality that employs various drugs acting on the ureter by different mechanisms.
The alpha-1 adrenergic blockers are the most commonly used agents for MET. Tamsulosin has been proved to increase the stone expulsion rate and decrease the expulsion time and thus has been extensively used [45]. Recently, phosphodiesterase-5 (PDE5) inhibitors have shown some benefit in stone expulsion. Phosphodiesterases are key enzymes regulating intracellular cyclic nucleotide metabolism (cyclic guanosine monophosphate [cGMP], cyclic adenosine monophosphate [cAMP]) and thus the contraction and relaxation of the muscle. In vitro studies have found that PDE5 inhibitors relax the ureteric muscle [6].
Tadalafil, a PDE5 inhibitor, acts by a nitric oxide/cGMP signaling pathway of smooth muscles, resulting in high levels of cGMP and thus causing relaxation of ureteral muscle [7]. Tadalafil has the longest duration of action (~36 hours) among the current PDE5 inhibitors. Although tadalafil has been used in the treatment of erectile dysfunction (ED) and lower urinary tract symptoms due to benign prostatic hyperplasia (BPH), its use in MET for ureteral stones is very limited in the Nepalese population. On the other hand, tamsulosin has been widely used for ureteral stones in our practice and has been found to be efficacious. This study aimed to analyze the safety and efficacy of tadalafil in distal ureteral stones and also to compare the efficacy of tadalafil with that of tamsulosin.
This prospective randomized study was performed in a tertiary care hospital in Kathmandu, Nepal, from June 2015 to May 2016. Approval for the study was obtained from the Institutional Review Board of the National Academy of Medical Sciences. Patients aged 18 years or older who presented to the Urology Outpatient Department (OPD) with ureteral stones 5–10 mm in size and located in the distal ureter (below the sacroiliac joint) were included. Diagnosis was made by noncontrast computed tomography (NCCT). Patients with urinary tract infection, severe refractory pain, severe hydronephrosis, acute or chronic renal failure, multiple ureteral stones, bilateral ureteral calculus or a single functioning kidney, any history of ureteral surgery or procedure, or urinary tract anomalies were excluded. Similarly, patients receiving concomitant treatment with alpha-blockers, calcium channel blockers, nitrates, steroids, or PDE5 inhibitors; patients having ischemic heart disease, congestive cardiac failure, or complicated hypertension; pregnant or lactating mothers; and patients who demanded urgent stone removal were also not included.
A total of 99 patients who fulfilled the criteria were enrolled in the study. After providing written informed consent, these patients were randomly divided into 2 groups by use of a computer-generated random number table. The patients in group A and those in group B received tamsulosin 0.4 mg or tadalafil 10 mg orally at bedtime, respectively. In both groups, drugs were continued until stone expulsion or for a period of 2 weeks. The drugs were used for 2 weeks because there is no strong evidence that a longer duration will increase the expulsion rate or that the deleterious effect of obstruction on kidney function will be minimized. Patients were asked to drink plenty of fluids and filter their urine with a thin cloth or net to look for stone expulsion. For pain control during colicky episodes, aceclofenac 100-mg tablets were given on an as-needed basis. The patients were followed up every week in the Urology OPD. The stone expulsion time, analgesic use, number of hospital visits for pain, and adverse effects of drugs were noted. The pain intensity was calculated by use of the World Health Organization numerical pain score of 0–10. Similarly, occurrences of any drug side effects like headache, postural hypotension, gastritis, and backache were recorded. Expulsion of the stone was confirmed by X-ray of the kidneys, ureters, and bladder; ultrasonography; or NCCT. The primary outcome was the stone expulsion rate. The secondary endpoints were stone expulsion time, number of colicky attacks, analgesics required, and drug side effects. Patients who failed to pass the stone after 2 weeks were subjected to semirigid ureteroscopy for stone removal.
Data were collected by filling in pro forma data sheets, which included the patients' demographic profiles, investigation reports, and the results of primary and secondary outcomes. Data were analyzed by using the SPSS, ver. 17.0 (SPSS Inc., Chicago, IL, USA). Discrete variables were evaluated by chi-square test and continuous variables by unpaired Student t-test. All statistical tests were based on two-tailed probability, and a p-value <0.05 was considered statistically significant.
Of 99 patients, 13 were lost to follow-up and 1 patient developed allergy to the drug (tamsulosin). Thus, 85 patients completed the study, 41 in group A (tamsulosin) and 44 in group B (tadalafil), and were analyzed (Fig. 1). The patients' mean age was 31.72±12.63 years (range, 18–68 years) and the male-to-female ratio was 1.5. Variables such as age, sex, symptom duration, presenting symptoms, blood chemistries like creatinine and blood sugar, and stone parameters like stone size and stone laterality were comparable between the 2 groups. The mean stone size was 7.09±1.2 and 7.13±1.5 mm in groups A and B, respectively. Almost two-thirds of the patients had stones on the right side (Table 1).
The overall stone expulsion rate in the study was 72.9% (62 of 85). The stone expulsion rate was significantly higher in group B than in group A (84.1% vs. 61.0%, p=0.017). The mean stone expulsion time was lower in group B (8.08±3.3 days) than in group A (9.64±3.8 days), but this difference was not significant (p=0.094). Forty-eight of 85 patients (56.47%) had no episodes of colicky pain and 52 of 85 patients (61.17%) did not require any analgesics for pain during the study period. The number of episodes of colicky pain, the pain score, and the analgesic requirement were less in group B, but these differences were not significant (Table 1).
The overall incidence of side effects was higher in group B than in group A (14.6% vs. 29.5%, p=0.099), but this difference was not significant. The individual side effects were also comparable between the 2 treatment groups (Table 2). Among the 24 male patients from group B, 18 patients (75%) felt a mild degree of penile tumescence (after intake of tadalafil) lasting for 20–30 minutes, but no patients developed priapism. However, all of these side effects were mild and well tolerated, and no patients had to drop out of the study.
Urolithiasis is a chronic disease with huge economic consequences and great public health importance, because it affects young people and has a high recurrence rate of approximately 50% within 5 years and 75% at 10 years [8]. Although ureteric stones make up only 20% of urolithiasis, they are the most symptomatic of the calculi. Studies have found that the probability of spontaneous passage of distal ureteral stones is 71% to 98% for stones sized less than 5 mm and 25% to 51% for stones sized 5 to 10 mm [910]. Many factors influence the spontaneous expulsion of stones, such as stone location, stone size, stone number, stone structure, ureteral spasm, mucosal edema or inflammation, and ureteral anatomy. Therefore, the use of medical therapy is justifiable to reduce edema, reduce spasm, and relax the smooth muscles for stone expulsion [11]. MET has recently emerged as an alternative strategy for the initial management of selected patients with distal ureteral stones [912].
A better understanding of ureteric function and pathophysiology has helped in employing MET as a conservative treatment approach. Many randomized controlled trials have supported the role of MET, especially with alpha-1 blockers [811131415]. The most common adrenoceptors found in the ureter are alpha-1D and alpha-1A [16]. These are more abundant on the distal ureter. Tamsulosin is an alpha-1A-selective alpha-blocker. Gratzke et al [7], in their in vitro study, showed the ureteral muscle relaxing effect of PDE5 inhibitors. Tadalafil is a PDE5 inhibitor that relaxes the ureteral muscle by increasing the cGMP level. Despite having a well-established role in ED and BPH, the use of tadalafil for MET is in the preliminary stage.
The stone expulsion rate in the present study was significantly higher in the tadalafil group than in the tamsulosin group (61% vs. 84.1%, p=0.017). Furthermore, we found that the expulsion rate of both drugs was better than the expulsion rates in historical controls used in earlier studies [13171819]. Although we could not find studies directly comparing tamsulosin with tadalafil, the expulsion rate of tadalafil was found to be higher in different studies (Table 3) [2021222324]. Kumar et al. [20] and Jayant et al. [21] in their studies compared the stone expulsion rate of tamsulosin with the tamsulosin and tadalafil combination. The expulsion rate was 74.2% versus 83.9% (p=0.349) and 65.5% versus 83.6% (p=0.031), respectively. In another study, Hasan et al. [22] found that tadalafil had an expulsion rate of 93% compared with 67% for a placebo group. In a randomized study with 285 patients, Kumar et al. [23] compared the efficacy of 3 drugs, tamsulosin, silodosin, and tadalafil, as MET for lower ureteral stones. The expulsion rate was 64.4%, 83.3%, and 66.7%, respectively, but there was no significant difference between the tamsulosin and tadalafil groups (p=0.875).
Subgroup analysis was performed between the patients who passed the stone (MET success) and those who failed to pass the stone (MET failure). Patient age (p=0.559) and the male-to-female ratio (p=0.921) were comparable between the success and failure groups. However, mean stone size was smaller in the MET success group (6.87±1.45 mm) than in the MET failure group (7.77±1.05 mm), which was statistically significant (p=0.008). Similarly, subgroup analysis was also performed among the patients who successfully passed the stones in both the tamsulosin and tadalafil groups. There were no significant differences in age (p=0.972), male-to-female ratio (p=0.272), or stone size (p=0.444) between these 2 groups.
MET not only facilitates stone passage, but also decreases the stone expulsion time, colicky pain episodes, and analgesic requirement. Jayant et al. [21], who had compared tamsulosin with the combination of tamsulosin and tadalafil, demonstrated a significantly decreased expulsion time (16.7±4.8 vs. 14.9±4.4 days, p=0.003), significantly fewer colicky pain episodes (1.60±1.0 vs. 0.45±0.68, p=0.000), and significantly less analgesic use (2.90±0.90 vs. 1.87±0.8, p=0.000). Colicky pain in ureteral stones occurs owing to an increase in intraureteral pressure above the site of ureteral obstruction. Kinnman et al. [25] demonstrated that α-blockade relieves ureteric colic by blocking the C-fibers responsible for mediating pain. Both drugs are thought to decrease the frequency and amplitude of phasic peristaltic contractions that accompany ureteric obstruction and to decrease the need for analgesia. In the present study, these parameters were lower in group B, but these differences did not reach the level of significance. Hasan et al. [22] reported a significantly lower pain score of 3.9 versus 7.9 (p<0.0001) and a significantly lower analgesic requirement in the tadalafil group than in the placebo group. Although the pain score was low in group B in our study, the difference was not statistically significant (2.09±2.5 vs. 2.29±2.5, p=0.744).
The incidence of side effects was higher in the tadalafil group, but the difference was not statistically significant. Similar results were demonstrated in studies by Kumar et al. [2023] and Jayant et al. [21]. No serious adverse effects were encountered in either group in our study and all reported side effects were mild and well tolerated. This is probably because the study population was young and lacked significant comorbidities.
Recently, a few studies have questioned the efficacy of MET for ureteral stones. Bensalah et al. [12] in 2008 performed a randomized study in which 129 patients were divided into tamsulosin and placebo groups and treated for 42 days. The expulsion rate was 77.0% and 70.5% for tamsulosin and placebo, respectively. However, mean stone diameter was only 3.1 mm, a stone size that naturally has a high spontaneous expulsion rate. A more recent well designed, randomized, multicenter, placebo-controlled study was reported from 24 hospitals in the United Kingdom in which 1,136 ureteral stone patients were given tamsulosin, nifedipine, and placebo for 4 weeks and followed up until 12 weeks [26]. Their primary outcome, absence of intervention by 4 weeks (which was regarded as equivalent to stone passage), was 81%, 80%, and 80% in the tamsulosin, nifedipine, and placebo groups, respectively, and was not significant (active treatment vs. placebo [p=0.78] and tamsulosin vs. nifedipine [p=0.77]). However, that study had limitations; first, no imaging was used to document the stone passage, and second, almost 75% of the stones were <5 mm in size. Currently, MET remains an established treatment option for lower ureteral stones.
Our study was not without limitations. The sample size was small, the treatment duration was short, and there was no placebo group. However, this is one of the few studies that used PDE5 inhibitors as a treatment for distal ureteral stones and thus is still valuable as a pilot study. Further larger, multi-institutional prospective studies will help to establish the role of PDE5 inhibitors as MET for distal ureteral stones.
Tadalafil has a significantly higher stone expulsion rate than tamsulosin as a MET for distal ureteral stones of 5–10 mm in size. Tadalafil also provides early stone expulsion, a greater decrease in colicky pain episodes, and a greater decrease in analgesic requirement, although not statistically significant. Both drugs are safe, effective, and well tolerated with minor side effects.
Figures and Tables
Table 1
Patients' characteristics and the results of the study

Table 2
Side effects in each group

Table 3
Stone expulsion rate of tamsulosin and tadalafil for distal ureteral stones in different studies
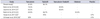
| Study | Tamsulosin | Tadalafil | Tamsulosin+Tadalafil | Silodosin | Placebo |
|---|---|---|---|---|---|
| Present studya | 61.0% | 84.1% | - | - | - |
| Kumar et al, 2014 [20] | 74.2% | - | 83.9% | - | - |
| Jayant et al, 2014 [21]a | 65.5% | - | 83.6% | - | - |
| Kumar et al, 2015 [23] | 64.4% | 66.7% | - | 83.3% | - |
| Hasan et al, 2011 [22]a | - | 93% | - | - | 67% |
| Al-Ansari et al, 2010 [24]a | 82% | - | - | - | 61% |
References
1. Pearle MS, Lotan Y. Urinary lithiasis: etiology, epidemiology, and pathogenesis. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders Elsevier;2012. p. 1257–1286.
2. Ahmed AF, Al-Sayed AY. Tamsulosin versus alfuzosin in the treatment of patients with distal ureteral stones: prospective, randomized, comparative study. Korean J Urol. 2010; 51:193–197.
3. Ueno A, Kawamura T, Ogawa A, Takayasu H. Relation of spontaneous passage of ureteral calculi to size. Urology. 1977; 10:544–546.
4. Singh SK, Agarwal MM, Sharma S. Medical therapy for calculus disease. BJU Int. 2011; 107:356–368.
5. Wang CJ, Huang SW, Chang CH. Efficacy of an alpha1 blocker in expulsive therapy of lower ureteral stones. J Endourol. 2008; 22:41–46.
6. Gratzke C, Uckert S, Kedia G, Reich O, Schlenker B, Seitz M, et al. In vitro effects of PDE5 inhibitors sildenafil, vardenafil and tadalafil on isolated human ureteral smooth muscle: a basic research approach. Urol Res. 2007; 35:49–54.
7. Gratzke C, Uckert S, Reich O, Schlenker B, Tilki D, Seitz M, et al. PDE5 inhibitors. A new option in the treatment of ureteral colic? Urologe A. 2007; 46:1219–1223.
8. Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006; 368:1171–1179.
9. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. The American Urological Association. J Urol. 1997; 158:1915–1921.
10. Shrestha A. Factors predicting spontaneous passage of ureteric stones [master's thesis]. Kathmandu: National Academy of Medical Sciences;2013.
11. Seitz C, Liatsikos E, Porpiglia F, Tiselius HG, Zwergel U. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009; 56:455–471.
12. Bensalah K, Pearle M, Lotan Y. Cost-effectiveness of medical expulsive therapy using alpha-blockers for the treatment of distal ureteral stones. Eur Urol. 2008; 53:411–418.
13. Parsons JK, Hergan LA, Sakamoto K, Lakin C. Efficacy of alpha-blockers for the treatment of ureteral stones. J Urol. 2007; 177:983–987.
14. Campschroer T, Zhu Y, Duijvesz D, Grobbee DE, Lock MT. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014; (4):CD008509.
15. Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007; 50:552–563.
16. Sigala S, Dellabella M, Milanese G, Fornari S, Faccoli S, Palazzolo F, et al. Evidence for the presence of alpha1 adrenoceptor subtypes in the human ureter. Neurourol Urodyn. 2005; 24:142–148.
17. Kumar S, Kurdia KC, Ganesamoni R, Singh SK, Nanjappa B. Randomized controlled trial to compare the safety and efficacy of naftopidil and tamsulosin as medical expulsive therapy in combination with prednisolone for distal ureteral stones. Korean J Urol. 2013; 54:311–315.
18. Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM. Nifedipine versus tamsulosin for the management of lower ureteral stones. J Urol. 2004; 172:568–571.
19. Dellabella M, Milanese G, Muzzonigro G. Randomized trial of the efficacy of tamsulosin, nifedipine and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J Urol. 2005; 174:167–172.
20. Kumar S, Jayant K, Agrawal S, Singh SK. Comparative efficacy of tamsulosin versus tamsulosin with tadalafil in combination with prednisolone for the medical expulsive therapy of lower ureteric stones: a randomized trial. Korean J Urol. 2014; 55:196–200.
21. Jayant K, Agrawal R, Agrawal S. Tamsulosin versus tamsulosin plus tadalafil as medical expulsive therapy for lower ureteric stones: a randomized controlled trial. Int J Urol. 2014; 21:1012–1015.
22. Hasan HF, Jaffal WN, Al-Hossona HA. The role of tadalafil in lower ureteric stone expulsion. Iraqi Postgrad Med J. 2011; 10:24–32.
23. Kumar S, Jayant K, Agrawal MM, Singh SK, Agrawal S, Parmar KM. Role of tamsulosin, tadalafil, and silodosin as the medical expulsive therapy in lower ureteric stone: a randomized trial (a pilot study). Urology. 2015; 85:59–63.
24. Al-Ansari A, Al-Naimi A, Alobaidy A, Assadiq K, Azmi MD, Shokeir AA. Efficacy of tamsulosin in the management of lower ureteral stones: a randomized double-blind placebo-controlled study of 100 patients. Urology. 2010; 75:4–7.
25. Kinnman E, Nygards EB, Hansson P. Peripheral alpha-adrenoreceptors are involved in the development of capsaicin induced ongoing and stimulus evoked pain in humans. Pain. 1997; 69:79–85.
26. Pickard R, Starr K, MacLennan G, Lam T, Thomas R, Burr J, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015; 386:341–349.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download