Abstract
Urethral stricture after radiation therapy for localized prostate cancer is a delicate problem as the decreased availability of tissue healing and the close relation to the sphincter complicates any surgical approach. We here review the pathophysiology, dosimetry, and the disease specific aspects of urethral strictures after radiotherapy. Moreover we discuss different treatment option such as direct vision internal urethrotomy as well as techniques for open reconstruction with and without tissue transfer.
Prostate cancer (PCa) is the second most commonly diagnosed cancer [1]. The majority of patients are diagnosed in potentially cureable early stages [2]. Standard local treatment options include active surveillance, radical prostatectomy (RP) and radiotherapy (RT), that can be delivered via external beam (EBRT) and/or brachytherapy (BT) [3]. According to the Surveillance, Epidemiology and End Results database the distribution of these treatment options in men with newly diagnosed PCa is the following: RP, 36%; EBRT, 20%; BT, 10%; EBRT+BT, 4% [4]. For localized disease, 5-year survival rates for these therapies alone or in combination reach almost a 100%; however, side effects associated with each treatment vary significantly [56]. Due to the high survival rates, the number of prostate cancer survivors in the United States annually increased by 200,000 men up to almost 2.8 millions in 2012, leaving a large cohort of men at risk for short and/or long-term side effects of their cancer treatment [6]. Despite significant advances in techniques for RT delivery (e.g., intensity modulated radiation therapy, IMRT), some patients treated with RT may suffer from long-term genitourinary side effects [7] and significant quality of life impact [48]. Particular the development of urethral stricture is a delicate problem. It occurs in about 2% of patients undergoing EBRT, 4% for BT and 11% of EBRT-BT combination therapy [4]. In addition, due to its specific pathophysiology, the treatment of radiation-induced urethral strictures is complex and demands some operative skills.
Radiation causes ionization events and production of free radicals resulting in different types of DNA damage. DNA double-strand brakes (DSB) are generally thought to represent the principal lethal events and the most critical lesions to RT. DSBs initiate a complex set of cellular responses including DNA damage recognition and transduction of the signal, resulting in many downstream effects including cell cycle checkpoint activation, induction and coordination of stress response genes, DNA repair, and/or activation of the apoptotic cascade [9]. The consequential cell death is generally caused by improperly repaired DNA damage and/or the induction of apoptosis. Moreover radiation activates pro-inflammatory and pro-fibrotic cytokines leading to vascular injury (endarteritis) and stem cell damage. The tissue responds with features of failed wound healing like vascular atrophy leading to poorly oxygenated tissue and/or collagen deposition with eventual tissue scarring [10]. Epithelial leakage allows extravastation of urine causing a fibrotic reaction. The induced inflammation processes lead to the proliferation of myofibroblasts, loss of smooth muscle cells and microvessels and collagen synthesis [11]. Consequential late effects may occur where severe early reactions have led to impaired tissue recovery. In order to facilitate cross-comparisons between investigators and institutions several systems for documenting normal tissue responses to RT have been developed. These include the Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer classification, the Common Terminology Criteria for Adverse Events (CTCAE v4) scale and the (LENT/SOMA) Late Effects Normal Tissue Task Force Subjective, Objective, Management, and Analytic system, specifically designed to score late reactions [12].
Several randomized clinical trials have shown that dose-escalated RT to the prostate gland resulted in improved biochemical and local controls. However, this improvement in outcomes is often associated with increased rates of urinary toxicity [131415]. Merrick et al. [15] revealed in a series with low-dose rate (LDR) BT patients that urethral stricture correlates highly with the radiation dose to the membranous urethra. In addition he described the dose applied 20 mm distal to the apex as independent risk factor for the development of urethral strictures. In a high-dose rate (HDR) series comparing 3 different fractionation schedules, the importance of the fractionation schedule and a higher urethral D10 (defined as the minimum dose received by the "hottest" 10% of the urethral volume) was demonstrated. Higher stricture rates were observed after 19 Gy in 2 fractions as compared to 18 Gy in 3 and 20 Gy in 4 fractions [16]. Another cohort of HDR patients treated as monotherapy with 4 fractions of 9.5 Gy within 48 hours showed very high rates of late genitourinary toxicity. The actuarial proportion of patients with late grade 3 toxicity at 5 years was 17.7%. Six out of 36 patients had a bulbar urethral stricture requiring urethral dilatation. Late grade 3 toxicity was associated with urethral V120 (urethral volume receiving ≥120% of the prescribed dose) [17]. Several factors influence the incidence of urethral strictures in RT patients, but it appears that rates are higher in EBRT-HDR compared with LDR-BT [18]. Nevertheless it is very important to properly select the patients for each specific modality, to strictly respect the urethral doses below the recommended dose constraints as well as to keep a rigorous quality assurance on the processes of RT planning and delivery.
The overall reported incidence of urethral stricture after RT for PCa varies between 0%–18 % [419]. The majority of series report rates after BT between 3%–10% [820], 1%–12% after EBRT [42122] and higher rates after the combination of both. However, more recent data using modern LDR-BT and IMRT techniques describe lower rates down to 3% [2324]. In a series by Mohammed et al. [18] stricture rates after high dose BT were higher (11%) compared to LDR-BT (4%) and EBRT (2%). Reported stricture rates also increase with longer follow-up periods. Results from the CaPSURE database published by Elliott et al. [19] revealed a correlation of stricture incidence and time showing that the stricture rate increased from 1% directly after treatment to 16% after 4 years (Table 1).
Urethral stricture after RT is a late complication usually observed 1–3 years after radiation. Several risk factors for the development of a urethral stricture have been identified. Previous transurethral resection of the prostate (TURP) increases the stricture rates up to 15% compared to 6% without prior resection [2526]. Interestingly the history of arterial hypertension in combination with diabetes mellitus is also a predictive factor, as this may lead to reduced blood supply due to changes in microcirculation. This explanation might also be conclusive for TURP as it results in hypovascularized fibrotic tissue with reduced capacity of wound healing after additional radiation [2627]. The combination of BT and EBRT also significantly increases the rates of strictures compared to BT or EBRT alone [28].
Typically urethral stricture after primary RT of the prostate appear in the bulbomembranous urethra (BM, >90%), mostly at or below the apex, even though theoretically receiving lower radiation dose compared to intraprostatic urethra where strictures are rarely seen [426]. The radiation sensitivity of the BM urethra is not well understood yet. Mohammed et al. [18] described a hot spot distally the bulbar urethra due to the cylindric volume in patients treated with HDR-BT. After a change of software in 2004 decreasing the dosage at the apex of the prostate he observed lower stricture rates (9% vs. 0%, p=0.04). Another explanation is caudal needle sipping during HDR-BT, however Hindson et al. [16] did not observe a decrease of stricture rates after replanning in cases of a caudal movement seen in computed tomography scan. However, as far as a proper coverage of target is achieved, the sparing of the prostatic apical urethra appears to be important to decrease the risk of stricture formation.
Postprostatectomy strictures are more often anastomotic strictures than urethral strictures, often imprecisely mixed with bladder neck obstruction (BNC). The published incidence rates of BNC after RP vary from 0%–10% but are decreasing with the use of modern technologies like robotic surgery (5.1% for open RP, 1.1% for laparoscopic RP, and 1.4% for robot-assisted laparoscopic radical prostatectomy [RLRP]) [29]. Risk factors are well described as multiple previous interventions, urinary leakage, adjuvant RT (up to >40%), ischemia and surgeon experience [30313233]. All these risk factors seem to have a compromised wound healing in common. As a result fibrotic tissue narrows the bladder neck. In contrast to post RT strictures anastomotic stricture due to RP develop within 2–8 months after surgery.
Usually patients present with typical lower urinary tract symptoms (LUTS). As mentioned the time to presentation is earlier after RP (2–8 months) compared to RT (1–3 years). Work-up is similar to "normal" LUTS including history taking (to rule out radiation cystitis), examination, urine analyses, uroflow, sonographie and antegrade and retrograde urethrographie (RUG). Specific care should be taken to prostate-specific antigen level to allow diagnosis of local recurrence. Antegrade and RUG allow determining stricture length and a cystoscopy the evaluation of the appearance of the urethral mucosa and stricture characteristics, especially if planning a urethroplasty.
A major challenge in treatment of radiation induced strictures is the urethral tissue damage with reduced healing capacity, not only of the strictures area itself but also proximal and distal of the scar. Moreover the close relation to the sphincter can complicate surgery. Management can be performed as endoscopic surgery and open urethroplasty.
Data from nonirradiated urethral strictures treated with dilatation and/or direct vision internal urethrotomy (DVIU) show a close correlation between the length of stricture and treatment response, as strictures <1 cm have higher success rates (50%–85%) compared to >1 cm (6%–40%). However, success rates decline progressively with longer follow-up [343536].
Brandes [37] reviewed their experience in men treated with dilatation or DVIU with radiation induced strictures (BT, EBRT, combination of both modalities) and report about a mean stricture length of 2.5 cm. Interestingly, the authors described completely different success rates according to the different radiation techniques. After BT they found a mean time to recurrence of 3.7 months, while this was increased to 26 months after EBRT. For nonradiation related 2- to 4-cm strictures recurrence rates of 50% at 12 months and 75% after 48 months are described. They concluded that the high failure rates are more probably due to high dose fraction of radiation rather than stricture length itself, as results after EBRT appeared to be comparable to nonirradiated strictures. However, the success rates after 4 years are poor (BT, 0%; EBRT, 20%). Even worse data is reported after the combination of both techniques with longer median stricture length (3.5 cm), shorter time to diagnosis (10.9 months) and higher failure rate after dilatation and/or DVIU. In conclusion, Brandes [37] stated: "As successive urethrotomy or dilation is short-lived and palliative, 80% of the patients require repeat treatment and most more than three".
Moreover, repeated conservative treatments complicate stricture characteristics and delay time to definitive urethroplasty.
The options for open reconstruction include stricture excision and primary anastomosis (EPA), buccal mucosa graft urethroplasty and flap reconstruction. The accurate diagnostics and careful patient selection are necessary for the selection of the best surgical technique and therefore successful treatment. Again, all techniques have to be performed in radiation damaged hypovascularized and hypoxic tissue with a decreased availability of tissue healing. When considering these principles, high success rates can be achieved, especially after EPA for short strictures.
Recently, Rourke et al. [38] published their results for 35 patients who underwent urethroplasty for radiation induced (20 patients after EBRT, 15 after BT) bulbomembranous stenosis with a mean length of 3.5 cm. For the majority (65.7%) EPA was performed, while the rest required buccal mucosa graft or penile flap. After a follow-up of 4 years cystoscopic patency was almost 86% with no difference between techniques. In contrast to most series they also documented complications: 31.4% experienced 90-day complication, all of them relatively mild Clavien-Dindo grades I–II. From these patients 25.7% complained about a new or impairment of a pre-existing incontinence. The rate decreased to 13.3 if patients having a prior TURP were excluded. While incontinence in patients without TURP was managed mostly with anticholinergics, incontinence in patients with prior TURP required intervention due to its sphincteric etiology (Table 2).
In the largest study examining the outcome of men treated for RT induced strictures Hofer et al. [39] examined 72 patients. Of these 42% received BT, 42% received EBRT and 14% a combination of both modalities and presented with a mean stricture length of 2.3 cm. The majority of the patients (n=66) were treated with EPA. Intervention was successful in 70% of the patients. The median time to recurrence was around 10 months and 18.5% complained about incontinence. Worsened continence might be explained by the close relationship to the external sphincter in combination with an impaired bladder (e.g., radiation cystitis, low compliance bladder) function.
In contrast to Rourkes, but in consensus to other author's data, the rate of erectile dysfunction remained stable (preoperative, 45.6%; postoperative, 50.9%) (Table 2) [39].
Technically surgery is performed as in nonradiation strictures, however the intervention is demanding because of the radiation damages fibrotic tissue, the close relationship to the sphincter and reduced healing capacity. Fibrotic and necrotic tissue should be removed before a tension free anastomosis of "healthy" mucosa and surrounding tissue is performed.
The selection of surgical intervention is an individual decision. However, after comparing the better long-term outcome data after EPA to those after tissue transfer (see below) EPA should be the first option for short strictures with few surrounding scar tissue distant from the sphincter.
Tissue transfer techniques include buccal and penile skin graft. The indication is usually based on stricture length. However, published data are controversial as some groups perform EPA up to 3 cm [39], while others perform tissue transfer for strictures longer the 1 or 2 cm. Generally speaking tissue transfer surgery has to deal with the same limitation due to the previous radiation exposure as EPA.
Ahyai et al. [40] recently published a series of 38 men receiving buccal mucosa graft urethroplasty for strictures after RT (64.9% EBRT, 21.6% BT, 13.5% a combination of both modalities) in Hamburg/Germany. Strictures were located in the BM urethra with a median length of 3 cm (range, 1–8 cm). After a median follow up of 2 years they described an overall success rate of 71% (Table 2). While the overall success rates are comparable to published EPA results, the recurrence rates increased over time. They observed success rates of 90%, 76%, and 39% after 1, 3, and 4 years after buccal mucosa graft urethroplasty, respectively [40]. This unsatisfying medium term results reported from a center of excellence in urethroplasty clearly indicate the difficulties in treating radiation therapy induced urethral strictures.
Many patients are treated with RT for localized prostate cancer. After treatment radiation induced stricture of the urethra is a severe long-term side effect, as radiation damage may result in vasculare atrophy, poorly oxygenated tissue and/or collagen deposition with eventual tissue scarring. The decreased availability of tissue healing and the close relation to the sphincter complicates any surgical approach. According to dilatation and/or DVIU results are poor. If open surgery is planned, the careful evaluation of the actual stricture, patient counseling and patient selection are basic requirements for a successful treatment. The surgeon should be experienced with all the techniques of open stricture surgery. Even in experienced hands, success rates decrease with the extent of tissue damage and stricture length. For short strictures EPA should be the first choice, as onlay techniques are required for longer strictures. Patients undergoing surgery should be informed about the chances of stricture recurrence. Moreover they need to know about a new or impairment of a pre-existing incontinence, especially for membranous strictures or after previous TURP or RP. Nonsuitable patients should be informed about alternative (palliative) methods such as intermittent self-catheterization. A continent vesicostomy or urinary diversion might be an alternative for patients with devastated bladder outlet (combination of stricture and incontinence).
Figures and Tables
Table 1
Stricture free rates after prostate cancer therapy
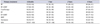
Values are presented as % stricture treatment free (95% confidence interval).
RP, radical prostatectomy; EBRT, external beam radiotherapy; BT, brachytherapy; WW, watchful waiting.
Adapted from Elliott et al. J Urol 2007;178:529–34, with permission of Elsevier [19].
Table 2
Characteristics after intervention for irradiation induced strictures

| Source | No. of patients | Location | Mean length (cm) | Intervention | F/U (yr) | Success definition | Success rate (%) | Time to recurrence (mo) |
|---|---|---|---|---|---|---|---|---|
| Rourke et al. [38] | 35 | BM | 2.1 | EPA (65%) | 4 | Patency | 91 | 29.8 |
| 6.1 | Graft/flap (35%) | 75 | ||||||
| Hofer et al. [39] | 72 | B & BM | 2.4 | EPA (92%) | 3.5 | ≤16 Fr on cystoscopy | 69.7 | 10.1 |
| 4.25 | Graft/flap (8%) | 5.5 | 85 | 7 | ||||
| Ahyai et al. [40] | 38 | B & BM | 2.9 | BMGU | 2.2 | Remanipulation or intervention | 71.1 | 17 |
References
1. SEER Stat fact sheets: prostate cancer [Internet]. Bethesda(MD): National Cancer Institute;2012. cited 2016 Mar 12. Available from: http://seer.cancer.gov/statfacts/html/prost.html.
2. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014; 65:124–137.
3. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014; 65:467–479.
4. Herschorn S, Elliott S, Coburn M, Wessells H, Zinman L. SIU/ICUD Consultation on Urethral Strictures: Posterior urethral stenosis after treatment of prostate cancer. Urology. 2014; 83:3 Suppl. S59–S70.
5. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008; 58:71–96.
6. Hudson SV, O'Malley DM, Miller SM. Achieving optimal delivery of follow-up care for prostate cancer survivors: improving patient outcomes. Patient Relat Outcome Meas. 2015; 6:75–90.
7. Viswanathan AN, Yorke ED, Marks LB, Eifel PJ, Shipley WU. Radiation dose-volume effects of the urinary bladder. Int J Radiat Oncol Biol Phys. 2010; 76:3 Suppl. S116–S122.
8. Aström L, Pedersen D, Mercke C, Holmang S, Johansson KA. Long-term outcome of high dose rate brachytherapy in radiotherapy of localised prostate cancer. Radiother Oncol. 2005; 74:157–161.
9. Liauw SL, Connell PP, Weichselbaum RR. New paradigms and future challenges in radiation oncology: an update of biological targets and technology. Sci Transl Med. 2013; 5:173sr2.
10. Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003; 4:529–536.
11. Singh M, Blandy JP. The pathology of urethral stricture. J Urol. 1976; 115:673–676.
12. Hoeller U, Tribius S, Kuhlmey A, Grader K, Fehlauer F, Alberti W. Increasing the rate of late toxicity by changing the score? A comparison of RTOG/EORTC and LENT/SOMA scores. Int J Radiat Oncol Biol Phys. 2003; 55:1013–1018.
13. Díez P, Mullassery V, Dankulchai P, Ostler P, Hughes R, Alonzi R, et al. Dosimetric analysis of urethral strictures following HDR (192)Ir brachytherapy as monotherapy for intermediate- and high-risk prostate cancer. Radiother Oncol. 2014; 113:410–413.
14. Martinez AA, Gonzalez J, Ye H, Ghilezan M, Shetty S, Kernen K, et al. Dose escalation improves cancer-related events at 10 years for intermediate- and high-risk prostate cancer patients treated with hypofractionated high-dose-rate boost and external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 79:363–370.
15. Merrick GS, Butler WM, Wallner KE, Galbreath RW, Anderson RL, Allen ZA, et al. Risk factors for the development of prostate brachytherapy related urethral strictures. J Urol. 2006; 175:1376–1380.
16. Hindson BR, Millar JL, Matheson B. Urethral strictures following high-dose-rate brachytherapy for prostate cancer: analysis of risk factors. Brachytherapy. 2013; 12:50–55.
17. Ghadjar P, Oesch SL, Rentsch CA, Isaak B, Cihoric N, Manser P, et al. Late toxicity and five year outcomes after high-dose-rate brachytherapy as a monotherapy for localized prostate cancer. Radiat Oncol. 2014; 9:122.
18. Mohammed N, Kestin L, Ghilezan M, Krauss D, Vicini F, Brabbins D, et al. Comparison of acute and late toxicities for three modern high-dose radiation treatment techniques for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012; 82:204–212.
19. Elliott SP, Meng MV, Elkin EP, McAninch JW, Duchane J, Carroll PR, et al. Incidence of urethral stricture after primary treatment for prostate cancer: data from CaPSURE. J Urol. 2007; 178:529–534.
20. Zelefsky MJ, Yamada Y, Cohen GN, Sharma N, Shippy AM, Fridman D, et al. Intraoperative real-time planned conformal prostate brachytherapy: post-implantation dosimetric outcome and clinical implications. Radiother Oncol. 2007; 84:185–189.
21. Lawton CA, Bae K, Pilepich M, Hanks G, Shipley W. Long-term treatment sequelae after external beam irradiation with or without hormonal manipulation for adenocarcinoma of the prostate: analysis of radiation therapy oncology group studies 85-31, 86-10, and 92-02. Int J Radiat Oncol Biol Phys. 2008; 70:437–441.
22. Gardner BG, Zietman AL, Shipley WU, Skowronski UE, Mc-Manus P. Late normal tissue sequelae in the second decade after high dose radiation therapy with combined photons and conformal protons for locally advanced prostate cancer. J Urol. 2002; 167:123–126.
23. Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2008; 70:1124–1129.
24. Sandhu AS, Zelefsky MJ, Lee HJ, Lombardi D, Fuks Z, Leibel SA. Long-term urinary toxicity after 3-dimensional conformal radiotherapy for prostate cancer in patients with prior history of transurethral resection. Int J Radiat Oncol Biol Phys. 2000; 48:643–647.
25. Seymore CH, el-Mahdi AM, Schellhammer PF. The effect of prior transurethral resection of the prostate on post radiation urethral strictures and bladder neck contractures. Int J Radiat Oncol Biol Phys. 1986; 12:1597–1600.
26. Sullivan L, Williams SG, Tai KH, Foroudi F, Cleeve L, Duchesne GM. Urethral stricture following high dose rate brachytherapy for prostate cancer. Radiother Oncol. 2009; 91:232–236.
27. Chon BH, Loeffler JS. The effect of nonmalignant systemic disease on tolerance to radiation therapy. Oncologist. 2002; 7:136–143.
28. Jarosek SL, Virnig BA, Chu H, Elliott SP. Propensity-weighted long-term risk of urinary adverse events after prostate cancer surgery, radiation, or both. Eur Urol. 2015; 67:273–280.
29. Msezane LP, Reynolds WS, Gofrit ON, Shalhav AL, Zagaja GP, Zorn KC. Bladder neck contracture after robot-assisted laparoscopic radical prostatectomy: evaluation of incidence and risk factors and impact on urinary function. J Endourol. 2008; 22:97–104.
30. Huang G, Lepor H. Factors predisposing to the development of anastomotic strictures in a single-surgeon series of radical retropubic prostatectomies. BJU Int. 2006; 97:255–258.
31. Erickson BA, Meeks JJ, Roehl KA, Gonzalez CM, Catalona WJ. Bladder neck contracture after retropubic radical prostatectomy: incidence and risk factors from a large single-surgeon experience. BJU Int. 2009; 104:1615–1619.
32. Gillitzer R, Thomas C, Wiesner C, Jones J, Schmidt F, Hampel C, et al. Single center comparison of anastomotic strictures after radical perineal and radical retropubic prostatectomy. Urology. 2010; 76:417–422.
33. Hu JC, Gu X, Lipsitz SR, Barry MJ, D'Amico AV, Weinberg AC, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009; 302:1557–1564.
34. Hafez AT, El-Assmy A, Dawaba MS, Sarhan O, Bazeed M. Long-term outcome of visual internal urethrotomy for the management of pediatric urethral strictures. J Urol. 2005; 173:595–597.
35. Holm-Nielsen A, Schultz A, Moller-Pedersen V. Direct vision internal urethrotomy. A critical review of 365 operations. Br J Urol. 1984; 56:308–312.
36. Boccon Gibod L, Le Portz B. Endoscopic urethrotomy: does it live up to its promises? J Urol. 1982; 127:433–435.
37. Brandes SB. Radiotherapy-Induced urethral strictures. In : Brandes SB, Morey AF, editors. Advanced male urethral and genital reconstructive surgery. New York: Humana Press;2014. p. 337–350.
38. Rourke K, Kinnaird A, Zorn J. Observations and outcomes of urethroplasty for bulbomembranous stenosis after radiation therapy for prostate cancer. World J Urol. 2016; 34:377–382.
39. Hofer MD, Zhao LC, Morey AF, Scott JF, Chang AJ, Brandes SB, et al. Outcomes after urethroplasty for radiotherapy induced bulbomembranous urethral stricture disease. J Urol. 2014; 191:1307–1312.
40. Ahyai SA, Schmid M, Kuhl M, Kluth LA, Soave A, Riechardt S, et al. Outcomes of ventral onlay buccal mucosa graft urethroplasty in patients after radiotherapy. J Urol. 2015; 194:441–446.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download