Abstract
Purpose
The traditional prone positioning of percutaneous nephrolithotomy (PCNL) is associated with various anesthetic and logistic difficulties. We aimed to compare the surgical outcomes of PCNLs performed using our modified supine position with those performed in the standard prone position.
Materials and Methods
A prospective group of 236 renal units (224 patients) undergoing PCNL were included in this 2 site study: 160 were performed in the modified supine position were compared with 76 undergoing PCNL in the prone position. The outcomes of radiation dose, radiation time, stone free rate, body mass index (BMI), stone size, operative time, length of stay (LOS), in hospital and complications were compared. Chi-square and t-tests were used.
Results
There were no significant differences in mean radiation time, radiation dose or stone size between the modified supine and prone groups. The supine group had a higher mean BMI (31 kg/m2 vs. 28 kg/m2, p=0.03), shorter mean surgical time (93 minutes vs. 123 minutes, p<0.001), shorter mean LOS (2 days vs. 3 days, p=0.005) and higher stone free rate (70% vs. 50%, p=0.005). There were no differences in septic or bleeding complications but the prone group had a higher rate of overall complications.
Percutaneous nephrolithotomy (PCNL) is the treatment of choice for renal stones ≥2 centimetres [1]. The traditional prone position for PCNL is favoured by a majority of urologists [2] due to familiarity with the procedure, larger surface area for choice of puncture site and a potentially more direct approach to the kidney [3].
However, the prone position is associated with several anaesthetic, surgical and logistical disadvantages. As a result, several alternative positions are increasingly being utilised including complete supine, modified supine, or flank positioning [456789] as they offer advantages including reduced ventilation and circulation difficulties, less radiation exposure to the surgeon, more direct renal puncture and avoidance of repositioning the patient during the procedure [45678910]. The modified supine position that combines a tilted supine position with lithotomy provides the additional benefit of allowing simultaneous retrograde access to the upper tracts. This enables a dual approach to large staghorn calculi and ureteric stones potentially reducing the operative time, trauma to the patient and increasing the stone free rate [11].
While there is substantial data comparing the supine PCNLs with the prone position, there is a paucity of data comparing the modified supine to the prone position and the current literature has no clear consensus on which position is superior. Thus the aim of this study is to determine the surgical outcomes of patients undergoing PCNL in the 2 positions.
A prospective study was conducted on 236 renal units undergoing PCNL where 148 patients (160 renal units) prospectively undergoing PCNL in the modified supine position as described previously [11] were compared to 76 patients in the standard prone position from November 2009 to February 2014 at our institution. Institutional Review Board approval obtained from the Monash Health Human Research Ethics Committee (approval number: 12336Q).
The modified supine position PCNL is performed a using a C-shaped vacuum beanbag on the operating table. Under general anaesthesia the legs are placed in the lithotomy position, with the ipsilateral hip flexed with a flexed knee, and the contralateral leg is abducted and supported in an extended position [11]. The beanbag is rolled under the hips and shoulders to tilt and support the torso at approximately 20 to 30 degrees. The ipsilateral arm is supported with a flexed elbow over the chest with the contralateral arm tucked next to the torso with an extended elbow. Suction is applied to the beanbag, thus supporting the patient in the tilted position (Fig. 1). A detailed description of procedure is included in our previous publication [11]. The number of punctures and pole of puncture was determined on the size and location of the calculus. All PCNLs (modified supine and prone) had ureteric catheters placed and ureteropelvic junction occlusion balloons were not used in any of the procedures. Nephrostomies were inserted if clinically indicated.
All patients booked for PCNL went into a pool of patients and then were allocated to an individual surgeon's list by the nurse-led surgical bookings team. All surgeons who perform PCNLs were included in this study. The adopted method was due to allocated surgeon's standard preference (Two surgeons performed PCNLs in the prone while 4 surgeons performed PCNLS in modified supine position) and all surgeons were well experienced the position of choice.
Patient demographics were collected from scanned medical records. Maximum stone diameter was used to assess stone burden. All those who had secondary procedures during the same admission or later for stone clearance were counted as having residual stones. All patients had postoperative X-Ray or computed tomography scans at 3 months to determine stone-free rates.
Measured data included radiation dose, radiation time, stone free rate, patient body mass index (BMI), stone size, operative time, length of stay in hospital and postoperative complications.
The data was analysed by SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) using chi-square and t-tests. A p-value less than 0.05 was considered statistically significant.
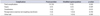
Similar characteristics were seen in both groups, but the patients who underwent modified supine PCNLs has a higher mean BMI (31 kg/m2 vs. 28 kg/m2, p=0.03) but had similar stone sizes (Table 1). While the stone locations and stone compositions between the 2 groups were similar, the majority of the prone procedures (90.8%) had the less complex lower pole punctures compared to modified supine group (67.5%) (Table 2).
The modified supine cohort was on average 30 minutes shorter than the mean operation time of the prone cohort (p<0.001) (Table 3). The stone free rate was significantly higher for the modified supine cohort than for the prone cohort (70% vs. 50%, p=0.005) with a significantly shorter mean length of stay in hospital (p=0.005). There were no significant differences in mean radiation time or radiation dose between the two groups (Table 3).
Of the modified supine cohort, 56 procedures (14%) included combined procedures (i.e., dual access with ureteroscopy or flexible pyeloscopy) and 16 of these patients (10%) also had ureteric calculi which were cleared during the same procedure.
All prone PCNLs had intraoperative nephrostomies placed, while in the modified supine group, all of the first 68 patients had intraoperative nephrostomies placed but of the subsequent cases, 58 (36%) had no nephrostomies and 36 (22.5%) were totally tubeless.
There was a significantly higher rate of overall complications seen in the prone group compared with the modified supine group (Table 4). However, for both groups the rate of complications was relatively low, with 14 total complications (18%) for the prone group and 13 total (8%) for the supine group. One major complication (haemothorax) occurred in the prone group which required drainage. Sepsis occurred in 4 patients (5%) in the prone group and 6 patients (3%) in the supine group, and there was a urine leak (urinoma requiring stenting or percutaneous drainage) for 1 patient in both the groups. Blood transfusions were required for 3 patients (4%) in the prone group and 3 patients (2%) in the modified supine group, with postoperative anaemia not requiring transfusion occurring in both groups, with 3 patients (4%) and 1 patient (0.6%) respectively. Other complications which occurred included need for post operative hyperkalaemia, and low post operative saturations.
To our knowledge this is the largest prospective single centre study comparing standard prone PCNL with a recently described modified supine position [11]. We found a shorter operative time in the modified supine group compared with the prone group. This 30-minute difference can be accounted for by not repositioning the patient (and consequently repeat prepping and draping, as well as staff rescrubbing and gowning), as well as the modified supine position facilitating dual access to the area, assisting with stone clearance and saving time [11]. Our findings are consistent with those of a recent meta-analysis of PCNL positioning by Liu et al. [12], where the supine position was found to have a mean reduction of 25 minutes when compared with the prone position. However, the evidence for shorter operating time is not entirely in favour of the modified supine position, with a prospective randomized study by Wang et al. [13] reporting lower operation times in their prone group, as compared to modified supine. While familiarity with the procedure performed in the supine position may affect the success and efficiency of the operation, Wang et al. [13]'s study also had patients with a much lower mean BMI compared to our series.
We found that the PCNLs performed in the modified supine position had a significantly higher stone-free rate. De Sio et al. [14], in keeping with our results, found the supine position to have higher stone-free rates. However, a comparison of positioning by Valdivia et al. [2], which comprised the 5,803 patients from the Clinical Research Office of the Endourological Society's (CROES) prospective PCNL database f ound that stone-f ree rates were significantly higher (77% vs 70.2%) for the prone group as compared with supine, though the vast majority of these cases would have been in the complete supine position. In addition to the CROES study, there are other studies favouring the prone position [12]. While these studies have compared prone PCNLs with complete supine PCNLs, factors that may explain our higher stone-free rate in the our modified supine position may include the possibility of simultaneous anterograde and retrograde stone removal in the supine position, and the effect of gravity-induced stone clearance [11]. Simultaneous antegrade and retrograde access which is an advantage of the modified supine position also gives dual access to large stag horn calculi as well as ureteric calculi provides better stone clearance in a single procedure. Furthermore, as the nephroscope enters from below the posterior axillary line as described in our previous article [11], this angle uses gravity to drain the fluid and the residual stone fragments.
The modified supine cohort stayed on average a day shorter in hospital than the prone group with most other studies showing no significant differences between the 2 groups [212]. One of the main reasons for shorter hospital stay due to nephrostomies. A large proportion of the supine PCNLs were done with no nephrostomies or completely tubeless, while the traditional prone PCNLs all had nephrostomies, which delayed discharge from hospital.
Increased BMI is one of the risk factors for renal calculi and associated with reduced stone-free rates [15]. The CROES prospective database of 5,803 patients found that obesity was associated with longer operative time, decreased stone-free rate (and subsequent higher re-treatment rate) [16]. The modified supine position offers several advantages in this regard. Firstly, as the patient is lying supine for the duration of the procedure, there is less pressure placed on their lungs compared to when they are lying prone. This reduces difficulties associated with maintaining stable ventilation of patients while they are prone, particularly obese patients where the abdominal compression can cause decreased venous output [10]. Supine position also allows easier and faster access to the airway should the need for reintubation arise. Secondly, performing PCNL in the traditional prone position required the patient to be moved from a supine to a prone position partway through the operation needing repositioning and redraping together with staff rescrubbing and regowning partway through the procedure, which has added difficulties in obese patents which is minimised in the modified supine position [11]. Furthermore the prone position is associated with increased risk of postoperative visual loss [17], direct pressure injuries and peripheral nerve damage, particularly to obese patients [10]. A study by Mazzucchi et al. [18] found that the complete supine position offers significantly shorter operative times and postoperative length of stay in hospital, when performed in obese patients. These factors strongly favour performing PCNL in the modified supine position especially in the obese patients, particularly with patients presenting with cardiopulmonary comorbidities. In addition to obese patients [16], patients with a solitary kidney [19] and patients with spinal deformities [20], some of whom are unable to lie in the prone position entirely [21] variations of the supine position has shown superior results.
Our study found significantly higher overall complication rates in the prone position compared with the modified supine position but transfusion and sepsis rates were similar between the two positions. The meta-analysis by Liu et al, [12] which also found no significant difference in complication rates between their modified supine and prone cohorts. While our rates of complications were within an acceptable range (11% of cohort), being slightly lower than other similar studies such as Scoffone et al. [9] (38.6%) or De Sio et al. [14] (17%). The same can be said of the rate of transfusions (2.5%) and sepsis (4.2%), which are also similar to previous studies [12]. It should be noted that our study was conducted at a tertiary referral centre where PCNLs were performed on more complex stones and higher risk patients.
One of the main limitations in this study was that the cases were not randomised, and therefore could introduce selection bias. However, allocation to a particular surgeon from a pool of patients for PCNLs by the nurse led booking team may have minimised some of this selection bias. A further limitations of this study was the learning curve associated with the modified supine position, as most surgeons were already familiar with the prone position for PCNL, but may not have had the same practice in the modified supine position and thus the surgeon's experience or skills and intersurgeon variability could exist and could have an effect on the results. In addition we did not adjust for stone characteristics such as hardness (stone composition), locations (renal pelvis, upper calyx, and lower calyx) and multiplicity (single or multiple stones) may have also had an influence on the operation time. We did not routinely measure the postoperative haemoglobin and only checked if clinically indicated, which could have affected transfusion rates.
This prospective study comparing the modified supine position with the standard prone position demonstrates reduced operative time and length of hospital stay, and increased stone-free rates with fewer complications. Given the benefits of the modified supine position for the surgical and anaesthetic teams, particularly with obese patient groups, and should be considered by all surgeons performing PCNLs.
Figures and Tables
 | Fig. 1This figure demonstrates the typical position used for our variation of the modified supine percutaneous nephrolithotomy prior to prepping and draping. This also shows the positioning of the bean bag which is utilized to position the patient for access. |
Table 1
Patient characteristics

Table 2
Stone characteristics and puncture sites

Table 3
Surgical outcomes

References
1. Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on urolithiasis [Internet]. Arnhem (NL): European Aossciation of Urology;c2015. cited 2015 May 23. Available from: http://uroweb.org/wp-content/uploads/22-Urolithiasis_LR_full.pdf.
2. Valdivia JG, Scarpa RM, Duvdevani M, Gross AJ, Nadler RB, Nutahara K, et al. Supine versus prone position during percutaneous nephrolithotomy: a report from the clinical research office of the endourological society percutaneous nephrolithotomy global study. J Endourol. 2011; 25:1619–1625.
3. Miano R, Scoffone C, De Nunzio C, Germani S, Cracco C, Usai P, et al. Position: prone or supine is the issue of percutaneous nephrolithotomy. J Endourol. 2010; 24:931–938.
4. Grasso M, Nord R, Bagley DH. Prone split leg and flank roll positioning: simultaneous antegrade and retrograde access to the upper urinary tract. J Endourol. 1993; 7:307–310.
5. Gofrit ON, Shapiro A, Donchin Y, Bloom AI, Shenfeld OZ, Landau EH, et al. Lateral decubitus position for percutaneous nephrolithotripsy in the morbidly obese or kyphotic patient. J Endourol. 2002; 16:383–386.
6. Valdivia Uría JG, Valle Gerhold J, Lopez Lopez JA, Villarroya Rodriguez S, Ambroj Navarro C, Ramirez Fabian M, et al. Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol. 1998; 160(6 Pt 1):1975–1978.
7. Steele D, Marshall V. Percutaneous nephrolithotomy in the supine position: a neglected approach? J Endourol. 2007; 21:1433–1437.
8. Ibarluzea G, Scoffone CM, Cracco CM, Poggio M, Porpiglia F, Terrone C, et al. Supine Valdivia and modified lithotomy position for simultaneous anterograde and retrograde endourological access. BJU Int. 2007; 100:233–236.
9. Scoffone CM, Cracco CM, Cossu M, Grande S, Poggio M, Scarpa RM. Endoscopic combined intrarenal surgery in Galdakao-modified supine Valdivia position: a new standard for percutaneous nephrolithotomy? Eur Urol. 2008; 54:1393–1403.
10. Atkinson CJ, Turney BW, Noble JG, Reynard JM, Stoneham MD. Supine vs prone percutaneous nephrolithotomy: an anaesthetist's view. BJU Int. 2011; 108:306–308.
11. McCahy P, Rzetelski-West K, Gleeson J. Complete stone clearance using a modified supine position: initial experience and comparison with prone percutaneous nephrolithotomy. J Endourol. 2013; 27:705–709.
12. Liu L, Zheng S, Xu Y, Wei Q. Systematic review and meta-analysis of percutaneous nephrolithotomy for patients in the supine versus prone position. J Endourol. 2010; 24:1941–1946.
13. Wang Y, Wang Y, Yao Y, Xu N, Zhang H, Chen Q, et al. Prone versus modified supine position in percutaneous nephrolithotomy: a prospective randomized study. Int J Med Sci. 2013; 10:1518–1523.
14. De Sio M, Autorino R, Quarto G, Calabrò F, Damiano R, Giugliano F, et al. Modified supine versus prone position in percutaneous nephrolithotomy for renal stones treatable with a single percutaneous access: a prospective randomized trial. Eur Urol. 2008; 54:196–202.
15. Andreoni C, Afane J, Olweny E, Clayman RV. Flexible ureteroscopic lithotripsy: first-line therapy for proximal ureteral and renal calculi in the morbidly obese and superobese patient. J Endourol. 2001; 15:493–498.
16. Fuller A, Razvi H, Denstedt JD, Nott L, Pearle M, Cauda F, et al. The CROES percutaneous nephrolithotomy global study: the influence of body mass index on outcome. J Urol. 2012; 188:138–144.
17. Agah M, Ghasemi M, Roodneshin F, Radpay B, Moradian S. Prone position in percutaneous nephrolithotomy and postoperative visual loss. Urol J. 2011; 8:191–196.
18. Mazzucchi E, Vicentini FC, Marchini GS, Danilovic A, Brito AH, Srougi M. Percutaneous nephrolithotomy in obese patients: comparison between the prone and total supine position. J Endourol. 2012; 26:1437–1442.
19. Wang Y, Hou Y, Jiang F, Wang Y, Wang C. Percutaneous nephrolithotomy for staghorn stones in patients with solitary kidney in prone position or in completely supine position: a single-center experience. Int Braz J Urol. 2012; 38:788–794.
20. Goumas-Kartalas I, Montanari E. Percutaneous nephrolithotomy in patients with spinal deformities. J Endourol. 2010; 24:1081–1089.
21. Rana AM, Bhojwani JP, Junejo NN, Das Bhagia S. Tubeless PCNL with patient in supine position: procedure for all seasons?--with comprehensive technique. Urology. 2008; 71:581–585.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download