Abstract
Parastomal hernia, defined as an "incisional hernia related to an abdominal wall stoma", is a frequent complication after conduit urinary diversion that can negatively impact quality of life and present a clinically significant problem for many patients. Parastomal hernia (PH) rates may be as high as 65% and while many patients are asymptomatic, in some series up to 30% of patients require surgical intervention due to pain, leakage, ostomy appliance problems, urinary obstruction, and rarely bowel obstruction or strangulation. Local tissue repair, stoma relocation, and mesh repairs have been performed to correct PH, however, long-term results have been disappointing with recurrence rates of 30%–76% reported after these techniques. Due to high recurrence rates and the potential morbidity of PH repair, efforts have been made to prevent PH development at the time of the initial surgery. Randomized trials of circumstomal prophylactic mesh placement at the time of colostomy and ileostomy stoma formation have shown significant reductions in PH rates with acceptably low complication profiles. We have placed prophylactic mesh at the time of ileal conduit creation in patients at high risk for PH development and found it to be safe and effective in reducing the PH rates over the short-term. In this review, we describe the clinical and radiographic definitions of PH, the clinical impact and risk factors associated with its development, and the use of prophylactic mesh placement for patients undergoing ileal conduit urinary diversion with the intent of reducing PH rates.
Parastomal hernias are one of the most common complications seen after conduit urinary diversion with up to half of patients exhibiting radiographic or clinical signs by two years after cystectomy. Up to a third of patients require surgical intervention, most commonly due to discomfort, poor fit of the ostomy appliance, or rarely due to obstruction, bowel perforation, or strangulation. The high prevalence of parastomal hernias, the morbidity of surgical repair, and high recurrence rates have prompted surgeons to attempt to prevent their formation from the time of the initial surgery. Randomized trials of prophylactic mesh placement at the time of conduit formation have demonstrated success in reducing parastomal hernia rates, all with acceptable morbidity. In this manuscript, we review the definitions of parastomal hernias, risk factors for developing a parastomal hernia, surgical maneuvers to correct it, and the background and early data on prophylactic mesh placement at the time of radical cystectomy.
Stomal complications remain one of the major challenges with conduit urinary diversion and have been shown to negatively impact on quality of life after radical cystectomy (RC) [1]. Although PH remains one of the most frequent complications after stoma formation, accurate rates have been difficult to estimate. Quoted rates for PH vary widely between 5%–65% [2345678] depending on the length of follow-up and whether the diagnosis is made clinically or radiographically. Many historical reports fail to state the definition used for PH in their studies and standardized clinical criteria to define PH have been lacking. Because of inconsistent definitions and variable lengths of follow-up, it is difficult to compare PH rates between different series. Rates of PH also vary with the type of stoma created, ranging between 4%–48% for end-colostomy and 1.8%–23% for end-ileostomy [9]. Loop ileostomy has the lowest reported rates of PH (0%–6.2%), possibly because these are often constructed on an elective basis with the intention of reversal at a later date and follow-up may not be long enough to identify significant PH rates [9]. Most studies have reported PH rates based upon clinical exam, which can vary based upon if the data is collected prospectively or retrospectively and whether it is self-reported or documented by the surgical team. Most clinical definitions of a PH are based upon the finding of a protrusion in the vicinity of the stoma, but studies differ greatly in terms of how the examinations were performed, i.e., supine or upright with or without Valsalva maneuvers. Recently several studies have used similar definitions for PH and reported rates of approximately 27%–50% after 12 months of follow-up [210]. While PH have been reported as late as 27 years after surgery [11], the majority occur within the first 2 years after surgery [1213]. A minimum follow-up of 12 months after the index operation is needed to accurately assess for the presence of PH [9]. The most appropriate clinical definition of PH is any palpable defect or bulge adjacent to the stoma when the patient is supine with legs elevated or when straining when upright. If cross-sectional imaging is added to the clinical exam, PH can be defined as any intra-abdominal content protruding along the ostomy [14].
Radiologic evaluation of the stoma site with cross-sectional imaging has been used as an aid to clinical exam to improve detection rates of PH. Radiographic criteria have the advantage of being objective, less impacted by physical factors such as body habitus during physical exam, and less subject to bias in the retrospective setting. Additionally, cross-sectional imaging allows for objective measures of the sizes of the stoma aperture and hernia sac longitudinally over time, which is imperative to understanding the natural history of PH. Cingi et al. [15] described a radiographic PH (rPH) rate of 78% and a clinical PH (cPH) rate of 52% in a series of 23 patients evaluated with both computed tomography (CT) scans and directed physical examination, suggesting that cross-sectional imaging appears superior to clinical exam in detecting PH. Moreno-Matias et al. [16] described a classification system for radiographic evidence of PH which has been successfully applied in a randomized, controlled trial setting [17] and in multiple retrospective series [218]. The classification system is based upon the relationship between the hernia sac and the bowel forming the stoma. A type 1 PH is defined as a hernia sac that contains prolapsed bowel forming the stoma, while a type 2 PH contains abdominal fat or omentum herniating through the abdominal wall defect created by the stoma. A type 3 hernia contains herniated loops of bowel other than that forming the stoma [16] (Fig. 1).
One concern regarding radiographic classification systems for PH is whether clinically insignificant hernias are being identified due to the increased sensitivity of cross-sectional imaging. Though experience with this radiographic classification system is limited, there appears to be good concordance between radiographically evident PH and clinical symptoms. Seo et al. [18] described the rates of cPH and rPH in 83 patients undergoing end-colostomy. All patients with type 3 rPH (n=12) were clinically detectable and all were symptomatic; 80% of type 2 rPH were clinically detectable and 75% were symptomatic; and 60% of type 1 rPH were clinically detectable with 63% being symptomatic. In other series, radiographic type 3 hernias have been universally identified on physical exam, while type 2 hernias have a concordance rate of 60%–80% with physical exam, suggesting radiographic identification of PH can be a relevant means for reporting clinically significant incidence rates, especially in the retrospective setting [2161819].
The size of the abdominal fascia trephine or aperture has been evaluated as a potential risk factor for the development of PH after stoma formation and correlations have been made between increasing size of the aperture and the presence of clinical symptoms. Seo et al. [18] reported significant differences in the diameter of the stomal fascial defect in symptomatic versus asymptomatic patients (76.45 mm vs. 49.41 mm, p=0.0000) and additionally noted significant correlation between aperture size and rPH type (type 2 rPH, 62.69 mm, type 3 rPH, 81.01; p=0.003). In a review of 108 patients undergoing end-colostomy with a median follow-up of 25 months, Hong et al. [19] identified aperture size to be a significant risk factor for the eventual development of PH. Aperture size was measured at the time of the first postoperative CT scan. The mean aperture size was 2.9 cm (range, 1.8–4.8 cm) and on multivariable analysis, aperture size (odds ratio [OR], 4.278; p<0.001) proved to be a significant and independent predictor of PH development along with female gender (OR, 4.406; p=0.005) and age (OR, 1.077; p=0.008). Similarly, Hotouras et al. [20] reported a rPH rate of 58% in 43 patients followed for a median of 26 months. The median aperture diameter in patients with rPH was 35 mm (range, 25–58 mm) and 22 mm (range, 10–36 mm) in those without evidence of rPH (p<0.0001). These authors noted no patient with rPH had an aperture diameter <25 mm.
While several studies describe a correlation between larger stoma aperture size and the risk of developing a symptomatic PH, there is not enough evidence to define an ideal trephine size at the time of stoma formation that will preclude the development of PH. The classical teaching has been to create an abdominal wall defect large enough to accommodate '2 fingers', which correlates to a fascial defect of approximately 3.5 cm for the average surgeon with size 7.5 gloves [2021]. To correct for the imprecise nature of stoma formation, some authors have suggested the use of a circular stapling device to create a more accurate trephine [22]. Using this technique to create a precise fascial defect of various sizes (17 mm, 25 mm, 32 mm), Resnick et al. reported only 1 out of 32 patients developed a cPH after 7 years of follow-up [2223]. The size of the abdominal wall defect needs to be taken into account at the time of index surgery. Pilgrim et al. [24] reported that for every 1-mm increase in size of the abdominal wall stoma above 35 mm there is a corresponding 10% increased risk of developing a cPH.
The bulk of literature dedicated to understanding PH comes from the colorectal community and PH rates have been difficult to compare between end-stomas and loop stomas, since many loop stomas are created with the intent of later reversal and follow-up times vary significantly between different series. Loop-ileostomies have the lowest reported rates of PH, likely because elective reversal of the stoma occurs before significant numbers of PH will develop. In contrast, intestinal conduit urinary diversion is rarely reversed and may provide some insight into this question. The type of conduit formed (end-stoma versus Turnbull loop stoma) has been described in retrospective series and no differences in clinical or rPH rates have been reported. Klein et al. [25] described stomal complications in 319 patients undergoing RC and intestinal conduit urinary diversion at their institution over an 11-year period of time; 65% of patients (n=206) had end-stomas and 35% (n=113) Turnbull loop stomas. They noted no difference in cPH rates at median follow-up of 33 months and 49 months for end- and loop-stomas, respectively. Additionally, all other complication rates were similar for both types of stomas. Similar to Klein et al. [25], our analysis did not find the type of stoma (end-stoma versus loop-stoma) to be a significant risk factor for clinical or rPH development on univariable or multivariable analyses [2].
The use of anchoring sutures fixing the conduit to the fascia has not been shown to reduce PH rates but remains a commonly performed aspect of the procedure. Pisters and colleagues described the impact of anterior fascial fixation sutures in 496 consecutive patients undergoing IC between 1995–2012 at MD Anderson Cancer Center. At a median follow-up of 16 months, they noted cPH in 61 patients (12.2%). The cPH rate was significantly higher in patients having anterior fascial sutures placed compared to those having no supporting sutures (15.3% vs. 7.3%, p=0.02) and the investigators noted the use of anterior fascial sutures was an independent risk factor on multivariable analysis for cPH development (OR, 2.3; 95% confidence interval [CI], 1.03–5.14; p=0.04). The authors concluded that the use of anterior fascial sutures did not appear to reduce cPH rates and that they should be avoided for ileal conduit (IC) surgery [26]. Multiple published reports in the colorectal literature support the lack of need to place fascial supporting sutures since they have not been shown to reduce PH rates [927282930].
Radiographic classifications offer an insight into the natural history of rPH, especially with respect to changes in rPH size and time to progression to a greater degree or type of rPH. We previously described a cohort of 386 patients having had an open RC and IC at our institution and reported on risk factors for the development of rPH. We noted that progression to a higher grade or type of hernia on subsequent CT scans occurred in over a third of patients when followed longitudinally [2]. Of 90 patients whose first evidence of rPH was classified as a type 2 hernia, 30 patients progressed to a type 3 rPH; 4 of 5 type 1 rPH progressed to type 3 rPH, although the small number of events in this second group precludes us from drawing conclusions about progression. The progression-free survival rate from a type 2 rPH to type 3 rPH is illustrated in Fig. 2. These data are consistent with the clinical observations that the natural history of PH is for progression and enlargement in many patients over time [11].
The etiology of PH is multifactorial and influenced by both technical and patient related factors. Technical factors, such as the type of stoma created, the size and location of the stoma, the use of fascial anchoring sutures, and preoperative marking by a wound-ostomy nurse may alter the risk of PH formation [12182024263132]. Patient-related factors believed to be associated with PH development include obesity, female gender, age, prior abdominal surgery, smoking, poor nutrition, emergency surgery, postoperative sepsis, corticosteroid use, and malignancy [2312131819333435]. Obesity, female gender, poor nutrition, and stoma aperture size have been found on multivariable analyses to be independent risk factors for rPH formation in retrospective series [2181920]. Our experience demonstrated several risk factors associated with the development of rPH. On multivariable analysis females (hazard ratio [HR], 2.25; 95% CI, 1.58–3.21; p<0.0001), patients with a higher body mass index (HR, 1.08 per unit increase; 95% CI, 1.05–1.12; p<0.0001) and lower preoperative albumin (HR, 0.43 per gm/dL; 95% CI, 0.25–0.75; p=0.003) were more likely to develop a rPH after adjusting for factors such as age, diabetes, smoking history, presence of chronic obstructive pulmonary disease, estimated intraoperative blood loss, prior abdominal surgery, preoperative radiation therapy, neoadjuvant chemotherapy and stoma type (end-stoma vs. Turnbull technique). Because body mass index (BMI) was analyzed as a continuous variable, there is not a specific value to which we can point that places a patient at an increased risk for developing a rPH, however, multiple series have documented this same concept of increasing risk with higher BMI. In our series, 75 patients had a BMI≥30 kg/m2 and ultimately 66 of these patients developed a rPH [2]. Liu et al. [3] found severely obese patients (>40 kg/m2) were at 4 times greater risk of developing a PH than those with a normal BMI (adjusted HR, 4.26; 95% CI, 1.52–11.93, p=0.006) while others have described increasing PH rates at BMI values>25 kg/m2 [336].
At question is whether the risk factors cited above are relevant across all patient populations or are specific to Western patients where many of these reports originated. Korean researchers have reported female gender (HR, 3.29; 95% CI, 1.77–6.11; p<0.0001), age over 60 years (HR, 2.37; 95% CI, 1.26–4.46; p=0.01), hypertension (HR 2.08; 95% CI, 1.14–3.81; p=0.02), BMI >25 kg/m2 (HR, 1.8; 95% CI, 1.02–3.16; p=0.04) [36], and aperture size (OR, 4.278; p<0.001) as risk factors associated with PH development [19]. Funahashi et al. [37] reported on 80 Japanese patients having an end-colostomy, 27.5% of whom developed a cPH after 2.6 years of median follow-up; median BMI for this cohort was 21.4 kg/m2 (range, 15.0–32.8 kg/m2). The median BMI for those who developed a cPH was 23.5 kg/m2 and 21.64 kg/m2 for those who did not. On multivariable analysis, they identified BMI (OR, 45.61; 95% CI, 1.698–1916; p=0.022), laparoscopic compared to open surgical approach (OR, 7.213; 95% CI, 1.061–66.283; p=0.043) and transperitoneal compared to extraperitoneal stoma approach (OR, 3.964; 95% CI, 1.226–13.975; p=0.021) as independent risk factors for PH development. These studies suggest that many of the risk factors for PH development are consistent regardless of geography, environmental, or genetic differences.
While most patients with PH are asymptomatic, up to a third will undergo surgical repair of the PH on an elective basis for bothersome symptoms or occasionally in emergent circumstances due to strangulation or bowel obstruction [13]. In a report of 782 ostomy patients with a median follow-up of 10.5 years, Ripoche et al. [11] identified cPH in 25.6% of patients. Only 24% of patients with cPH denied the presence of symptoms and in the three quarters who were symptomatic, 46% reported pain, 37% stomal appliance problems, 36% leakage, 29% skin irritation, and 20% described psychological and aesthetic concerns secondary to the PH. Stomal prolapse occurred in 18% and at least one episode of obstruction was observed in 15% of patients. Liu et al. [3] reported a cPH rate of 29% at a median follow-up of 29 months, 45% of whom underwent surgical repair for abdominal pain (58%), acute strangulation or bowel obstruction (15%), partial small bowel obstruction (15%), or for elective reasons (12%). In our series, we noted a cPH rate of 24%, 40% of whom were symptomatic. Of the 93 patients with a cPH, an abdominal hernia belt or binder was prescribed for 75 patients (81%) and 16 (17%) were referred for possible PH repair. Only 8 patients (9%) with symptomatic cPH underwent PH repair, two of which were performed emergently due to bowel strangulation. Three of 8 PH repairs developed a recurrent cPH a median of 13 months (range, 10–22 months) later. The low rates of referral may reflect the need to balance the competing issues of advanced disease and short life expectancy in some patients with high recurrence rates and potential morbidity associated with PH repair [2].
Up to 30% of patients who develop a PH will undergo surgical repair, most often due to pain, difficulties with the stoma appliance, leakage, and rarely in the emergent setting due to bowel strangulation or obstruction. Local repair using native tissues has been associated with unacceptably high recurrence rates as high as 76% [59112738394041] and relocation of the stoma to another quadrant of the abdomen still requires closure of the original stoma defect, placing both sites at risk for hernias in up to 60% of patients [27]. The use of mesh has been adopted for PH repair with varying techniques demonstrating roughly equal improvements over local tissue repair. Mesh-based PH repairs have reported recurrence rates of approximately 10% in small, nonrandomized reports with relatively short follow-up [27].
There are 4 basic approaches to mesh-based PH repairs, each corresponding to the location of where the mesh is placed with respect to the layers of the body wall: onlay – mesh is placed on the anterior fascial aponeurosis; inlay – mesh is cut to the size of the defect and sutured to the wound edge at the margins of the stomal defect; sublay (retro-rectus) – mesh is placed dorsal to the rectus muscle, anterior to the posterior rectus sheath; and intraperitoneal onlay – mesh is placed intraperitoneally on the peritoneum (Fig. 3). For all approaches other than the inlay technique, the size of the mesh will extend approximately 5–10 cm beyond the hernia defect circumferentially. The onlay technique attaches the mesh to the anterior rectus sheath and requires significant mobilization of the subcutaneous tissue, thereby increasing the risk of seroma formation adjacent to the mesh. The inlay technique has largely been abandoned for incisional hernias due to unacceptably high recurrence rates. The intraperitoneal onlay technique allows for contact between the mesh and abdominal contents, which impacts the choice of mesh used for repairs. Meshes that induce an inflammatory response cannot be placed in contact with abdominal contents without a high risk of fistula formation, adhesions, and septic complications. Mesh constructed of 2 layers is therefore typically preferred for this technique with the non-absorbable surface of the mesh being oriented toward the abdominal wall to allow for integration and the absorbable, nonreactive side of the mesh oriented toward the visceral contents. These concepts are particularly important for those considering prophylactic mesh placement at the time of minimally-invasive, intracorporeal urinary diversion. The sublay technique has been proposed as the most advantageous technique for mesh-based repairs of PH. The anatomic plane between the posterior aspect of the rectus muscle and the underlying fascia and peritoneum is often preserved and intraabdominal pressure does not allow the mesh to be displaced.
The negative quality of life issues, morbidity of surgical repair, and relatively high recurrences rates have prompted surgeons to attempt to prevent PH from the time of the index operation. There have been 5 prospective, randomized studies where mesh was placed at the time of stoma formation in an attempt to prevent PH, all of which have demonstrated significant reductions in the cPH or rPH rates without associated postoperative complications or long-term morbidity [17424344] (Table 1). Four studies used partially absorbable mesh and the fifth was a phase I trial of a biologic mesh in patients undergoing loop ileostomy with planned reversal six months later. The most comprehensive and mature series comes from Janes et al. [4245] who reported short and long-term results from their randomized trial. After both 12-month and 5-year follow-up for patients in their randomized trial, they reported significant reductions in the rates of cPH for patients receiving prophylactic mesh compared to standard surgery. At a minimum of 5-year follow-up, the cPH rate for those alive with mesh was 13% compared to 81% who had standard surgery (p< 0.001). Over a mean of 72 months of follow-up, no fistulas, strictures, and mesh infections were noted and no patient has required mesh removal [45].
Not all randomized trials of prophylactic mesh placement at the time of stoma formation have demonstrated equivalent results. Vierimaa et al. [46] reported on 83 patients randomized to have a dual layer mesh placed in the intraperitoneal onlay position at the time of laparoscopic end-colostomy formation versus traditional stoma formation. The primary endpoints for the trial were both cPH and rPH rates with secondary endpoints being stoma-related morbidity and need for PH repair. The authors noted a significant reduction in cPH rates for those receiving mesh compared to those having standard surgery (14.3% vs. 32.3%, p=0.049), however, the rates of rPH as assessed by CT imaging was not different (51.4% vs. 53.1%, p=1.00). The extent of rPH was similar according to the European Hernia Society classification system (p=0.41) and colostomy related morbidity did not differ between the groups (32.3% vs. 14.3%, p=0.14).
Nonrandomized series of consecutive patients receiving prophylactic mesh at the time of index surgery have recently been published. Styrke et al. [47] reported a single institution, 10-year consecutive series of 114 patients having prophylactic mesh placed in the sublay position at the time of RC and IC formation. After a median follow-up of 35 months, they reported a cPH rate of 14% in 58 evaluable patients and no mesh-related complications. In contrast to other investigators, Nikberg et al. [48] did not identify a difference in cPH or rPH rates after introducing prophylactic sublay mesh for all patients undergoing end-colostomy at their institution beginning in 2007. When compared to matched patients having traditional surgery (n=135) between 1997–2007, those having prophylactic mesh (n=71) after 2007 had the exact same cPH rates (25%, p=0.953) and rPH rates (53%, p=0.176). The degree of herniation on cross-sectional imaging (containing omentum or bowel in the hernia sac) was similar for those having mesh placed and those having standard surgery (80% vs. 61%, p=0.155). On multivariable analysis, these authors found BMI to be an independent risk factor for development of PH (HR, 1.09, 95 % CI, 1.00–1.18).
Beginning September 2013, we have offered prophylactic mesh placement at the time of IC construction in patients at high-risk for PH development. Based upon risk factors identified in a previously published report [2], men with BMI >30 kg/m2 and all women regardless of BMI have been consented for prophylactic mesh placement at open RC. The median follow-up for the first 33 patients (16 men and 17 women) having prophylactic mesh placed is 479 days, two-thirds of whom have had more than 1 year of follow-up. Despite having a number of wound and infectious complications physically remote from the mesh, there have been no mesh infections, fistulas, or strictures identified and no patient has required removal of mesh to date. When compared to a matched group of 220 historic controls having traditional surgery, complication rates and types were no different for patients having mesh placed. At 1 year, 4 of 33 prophylactic mesh patients (12%) developed rPH, compared to 59 of 220 (27%) of historic controls, representing a 56% relative risk reduction (p=0.043).
There is increasing interest and utilization of minimally invasive techniques for RC and urinary diversion. To date, there are no reports of prophylactic mesh placement with the intent of reducing PH rates at the time of minimally invasive intracorporeal urinary diversion. The technique of prophylactic mesh placement in the sublay position is impractical for those undergoing intracorporeal diversion since access to and visualization of the retro-rectus space would be severely limited. Prophylactic mesh would need to be placed in the intraperitoneal onlay position in this setting. The choice of mesh is important, since bowel contents will be in direct contact with the foreign body and the nonreactive side should be oriented toward the visceral contents. One mesh designed for this approach is the Dynamesh IPST implant (FEG Textiltechnik, Aachen, Germany), which is a 3-dimensional preshaped, open-pore and monofilament mesh consisting of polyvinylidene fluoride (PVDF) and polypropylene. The PVDF side of the dual-component mesh has a funnel extending from its central aspect through which the conduit is placed. The funnel is oriented toward the visceral side of the abdomen and encircles the conduit and a portion of its mesentery as it exits the abdominal wall. Surrounding the funnel is a border of mesh that is secured to the anterior abdominal wall peritoneum. The polypropylene layer of the mesh is oriented away from the abdominal contents to reduce the risk of adhesions or erosion. This technique has been described for laparoscopic repair and revision of PH [49], but the same technique would potentially apply if used in the prophylactic setting for either open or minimally invasive surgery.
Parastomal hernias represent a clinically significant problem for patients undergoing conduit urinary diversion. While many patients are asymptomatic, PH can negatively impact on quality of life and up to a third of patients undergo repair due to bothersome symptoms or in the emergent setting. The morbidity of PH repair and relatively high recurrence rates have prompted surgeons to attempt maneuvers at the time of index surgery to reduce PH rates. Prophylactic mesh placement appears effective in reducing cPH and rPH rates based upon evidence from randomized trials in patients undergoing end-colostomy surgery. Urinary diversion may present a set of unique potential complications due to the presence of both bowel and uretero-intestinal anastomoses. Early experience with this technique suggests that placement of prophylactic, partially absorbable mesh in IC patients at high risk for PH formation appears feasible and safe. The degree to which placement of prophylactic mesh at the time of IC construction reduces PH rates should be established in the setting of a randomized, controlled trial.
Figures and Tables
 | Fig. 1Radiographic classification of parastomal hernia: (A) type 1, hernia sac that contains prolapsed bowel forming the stoma; (B) type 2, hernia sac contains abdominal fat or omentum herniating through the abdominal wall defect created by the stoma; (C) type 3, hernia sac contains herniated loops of bowel other than that forming the stoma. |
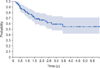 | Fig. 2Progression in years from type 2 to type 3 radiographic parastomal hernia (n=90 patients). A type 2 radiographic parastomal hernia contains abdominal fat or omentum herniating through the abdominal wall defect created by the stoma. A type 3 parastomal hernia contains herniated loops of bowel other than that forming the stoma. |
 | Fig. 3Four basic approaches for mesh-based hernia repairs. (A) Onlay – mesh is placed on the anterior fascial aponeurosis; (B) inlay – mesh is cut to the size of the defect and sutured to the wound edge at the margins of the stomal defect; (C) sublay (retro-rectus) – mesh is placed dorsal to the rectus muscle, anterior to the posterior rectus sheath; and (D) intraperitoneal onlay – mesh is placed intraperitoneally on the peritoneum. |
Table 1
Randomized controlled trials of prophylactic mesh placement

| Source | Type of stoma | Type of mesh | Placement technique | No. of patients | Median follow-up | Primary endpoint | PH rate | Mesh-related complications |
|---|---|---|---|---|---|---|---|---|
| Janes et al. [10] | Permanent end colostomy | Partially absorbable (Vypro) | Sublay | Mesh, 27; control, 27 | 14 months (95% CI, 12–17) | Clinical PH | At 12 months: | None reported |
| Mesh, 0/16 (0%); control; 8/18 (44.4%) | ||||||||
| Serra-Aracil et al. [17] | Permanent end colostomy | Partially absorbable (Ultrapro) | Sublay | Mesh, 27; control, 27 | 29 mo (range, 13–49 mo) | Clinical PH | At 29 months (median) | None reported |
| Radiographic PH | Clinical PH | |||||||
| Mesh, 4/27 (14.8%); control; 11/27 (40.7%) | ||||||||
| Radiographic PH | ||||||||
| Mesh: 6/27 (22.2%); control; 12/27 (44.4%) | ||||||||
| Hammond et al. [43] | Loop stoma | Xenogenic collagen | Sublay | Implant, 10; control, 10 | 6.5 mo | Clinical PH | At 12 months: | None reported |
| Implant: 0/10 (0%); control; 3/10 (33.3%) | ||||||||
| Lambrecht et al. [44] | Permanent end colostomy | Polypropylene | Sublay | Mesh, 32; control, 26 | 40 mo (range, 3–87 mo) | Clinical PH | At 24 months: | None reported |
| Mesh, 2/32 (6.3%); control; 12/26 (46.2%) | ||||||||
| Vierimaa et al. [46] | Permanent end colostomy | Partially absorbable (Dyna-Mesh IPOM) | Intraperitoneal Onlay | Mesh, 35; control, 35 | 12 mo | Clinical PH | At 12 months: | None reported |
| Radiographic PH | Clinical PH | |||||||
| Mesh, 5/35 (14.3%); control; 12/32 (32.3%) | ||||||||
| Radiographic PH | ||||||||
| Mesh, 18/35 (51.4%); control; 17/32 (53.1%) |
ACKNOWLEDGMENTS
We would like to express our thanks to Simon Kimm, M.D. for assistance in creating the images and illustrations for this manuscript.
References
1. Gerharz EW, Mansson A, Hunt S, Skinner EC, Månsson W. Quality of life after cystectomy and urinary diversion: an evidence based analysis. J Urol. 2005; 174:1729–1736.
2. Donahue TF, Bochner BH, Sfakianos JP, Kent M, Bernstein M, Hilton WM, et al. Risk factors for the development of parastomal hernia after radical cystectomy. J Urol. 2014; 191:1708–1713.
3. Liu NW, Hackney JT, Gellhaus PT, Monn MF, Masterson TA, Bihrle R, et al. Incidence and risk factors of parastomal hernia in patients undergoing radical cystectomy and ileal conduit diversion. J Urol. 2014; 191:1313–1318.
4. Farnham SB, Cookson MS. Surgical complications of urinary diversion. World J Urol. 2004; 22:157–167.
5. Kouba E, Sands M, Lentz A, Wallen E, Pruthi RS. Incidence and risk factors of stomal complications in patients undergoing cystectomy with ileal conduit urinary diversion for bladder cancer. J Urol. 2007; 178(3 Pt 1):950–954.
6. Wood DN, Allen SE, Hussain M, Greenwell TJ, Shah PJ. Stomal complications of ileal conduits are significantly higher when formed in women with intractable urinary incontinence. J Urol. 2004; 172(6 Pt 1):2300–2303.
7. Bloom DA, Grossman HB, Konnak JW. Stomal construction and reconstruction. Urol Clin North Am. 1986; 13:275–283.
8. Fontaine E, Barthelemy Y, Houlgatte A, Chartier E, Beurton D. Twenty-year experience with jejunal conduits. Urology. 1997; 50:207–213.
9. Israelsson LA. Parastomal hernias. Surg Clin North Am. 2008; 88:113–125.
10. Janes A, Cengiz Y, Israelsson LA. Experiences with a prophylactic mesh in 93 consecutive ostomies. World J Surg. 2010; 34:1637–1640.
11. Ripoche J, Basurko C, Fabbro-Perray P, Prudhomme M. Parastomal hernia. A study of the French federation of ostomy patients. J Visc Surg. 2011; 148:e435–e441.
12. Martin L, Foster G. Parastomal hernia. Ann R Coll Surg Engl. 1996; 78:81–84.
13. Marimuthu K, Vijayasekar C, Ghosh D, Mathew G. Prevention of parastomal hernia using preperitoneal mesh: a prospective observational study. Colorectal Dis. 2006; 8:672–675.
14. Jänes A, Weisby L, Israelsson LA. Parastomal hernia: clinical and radiological definitions. Hernia. 2011; 15:189–192.
15. Cingi A, Cakir T, Sever A, Aktan AO. Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum. 2006; 49:1559–1563.
16. Moreno-Matias J, Serra-Aracil X, Darnell-Martin A, Bombardo-Junca J, Mora-Lopez L, Alcantara-Moral M, et al. The prevalence of parastomal hernia after formation of an end colostomy. A new clinico-radiological classification. Colorectal Dis. 2009; 11:173–177.
17. Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, Darnell A, Mora-Lopez L, Alcantara-Moral M, et al. Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg. 2009; 249:583–587.
18. Seo SH, Kim HJ, Oh SY, Lee JH, Suh KW. Computed tomography classification for parastomal hernia. J Korean Surg Soc. 2011; 81:111–114.
19. Hong SY, Oh SY, Lee JH, Kim DY, Suh KW. Risk factors for parastomal hernia: based on radiological definition. J Korean Surg Soc. 2013; 84:43–47.
20. Hotouras A, Murphy J, Power N, Williams NS, Chan CL. Radiological incidence of parastomal herniation in cancer patients with permanent colostomy: what is the ideal size of the surgical aperture? Int J Surg. 2013; 11:425–427.
21. Keeling NJ, Ataullah CM, Wastell C. A survey of glove preferences of general and orthopaedic surgeons in North West Thames Regional Health Authority. J Hosp Infect. 1995; 30:305–308.
22. Resnick S. New method of bowel stoma formation. Am J Surg. 1986; 152:545–548.
23. Koltun L, Benyamin N, Sayfan J. Abdominal stoma fashioned by a used circular stapler. Dig Surg. 2000; 17:118–119.
24. Pilgrim CH, McIntyre R, Bailey M. Prospective audit of parastomal hernia: prevalence and associated comorbidities. Dis Colon Rectum. 2010; 53:71–76.
25. Klein EA, Montie JE, Montague DK, Novick AC, Straffon RA. Stomal complications of intestinal conduit urinary diversion. Cleve Clin J Med. 1989; 56:48–52.
26. Pisters AL, Kamat AM, Wei W, Leibovici D, Liu J, Grossman HB, et al. Anterior fascial fixation does not reduce the parastomal hernia rate after radical cystectomy and ileal conduit. Urology. 2014; 83:1427–1431.
27. Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg. 2003; 90:784–793.
28. Makela JT, Turku PH, Laitinen ST. Analysis of late stomal complications following ostomy surgery. Ann Chir Gynaecol. 1997; 86:305–310.
29. Londono-Schimmer EE, Leong AP, Phillips RK. Life table analysis of stomal complications following colostomy. Dis Colon Rectum. 1994; 37:916–920.
30. Leong AP, Londono-Schimmer EE, Phillips RK. Life-table analysis of stomal complications following ileostomy. Br J Surg. 1994; 81:727–729.
31. Emmott D, Noble MJ, Mebust WK. A comparison of end versus loop stomas for ileal conduit urinary diversion. J Urol. 1985; 133:588–590.
32. McGrath A, Porrett T, Heyman B. Parastomal hernia: an exploration of the risk factors and the implications. Br J Nurs. 2006; 15:317–321.
33. Carne PW, Frye JN, Robertson GM, Frizelle FA. Parastomal hernia following minimally invasive stoma formation. ANZ J Surg. 2003; 73:843–845.
34. Sjödahl R, Anderberg B, Bolin T. Parastomal hernia in relation to site of the abdominal stoma. Br J Surg. 1988; 75:339–341.
35. Gögenur I, Mortensen J, Harvald T, Rosenberg J, Fischer A. Prevention of parastomal hernia by placement of a polypropylene mesh at the primary operation. Dis Colon Rectum. 2006; 49:1131–1135.
36. Sohn YJ, Moon SM, Shin US, Jee SH. Incidence and risk factors of parastomal hernia. J Korean Soc Coloproctol. 2012; 28:241–246.
37. Funahashi K, Suzuki T, Nagashima Y, Matsuda S, Koike J, Shiokawa H, et al. Risk factors for parastomal hernia in Japanese patients with permanent colostomy. Surg Today. 2014; 44:1465–1469.
38. Goligher JC, Lloyd-Davies OV, Robertson CT. Small-gut obstructions following combined excision of the rectum with special reference to strangulation round the colostomy. Br J Surg. 1951; 38:467–473.
39. Cuthbertson AM, Collins JP. Strangulated para-ileostomy hernia. Aust N Z J Surg. 1977; 47:86–87.
40. Rubin MS, Schoetz DJ Jr, Matthews JB. Parastomal hernia. Is stoma relocation superior to fascial repair? Arch Surg. 1994; 129:413–418.
41. Horgan K, Hughes LE. Para-ileostomy hernia: failure of a local repair technique. Br J Surg. 1986; 73:439–440.
42. Janes A, Cengiz Y, Israelsson LA. Randomized clinical trial of the use of a prosthetic mesh to prevent parastomal hernia. Br J Surg. 20040; 91:280–282.
43. Hammond TM, Huang A, Prosser K, Frye JN, Williams NS. Parastomal hernia prevention using a novel collagen implant: a randomised controlled phase 1 study. Hernia. 2008; 12:475–481.
44. Lambrecht JR, Larsen SG, Reiertsen O, Vaktskjold A, Julsrud L, Flatmark K. Prophylactic mesh at end-colostomy construction reduces parastomal hernia rate: a randomized trial. Colorectal Dis. 2015; 17:O191–O197.
45. Janes A, Cengiz Y, Israelsson LA. Preventing parastomal hernia with a prosthetic mesh: a 5-year follow-up of a randomized study. World J Surg. 2009; 33:118–121.
46. Vierimaa M, Klintrup K, Biancari F, Victorzon M, Carpelan-Holmstrom M, Kossi J, et al. Prospective, randomized study on the use of a prosthetic mesh for prevention of parastomal hernia of permanent colostomy. Dis Colon Rectum. 2015; 58:943–949.
47. Styrke J, Johansson M, Granåsen G, Israelsson L. Parastomal hernia after ileal conduit with a prophylactic mesh: a 10 year consecutive case series. Scand J Urol. 2015; 49:308–312.
48. Nikberg M, Sverrisson I, Tsimogiannis K, Chabok A, Smedh K. Prophylactic stoma mesh did not prevent parastomal hernias. Int J Colorectal Dis. 2015; 30:1217–1222.
49. Köhler G, Emmanuel K, Schrittwieser R. Single-port parastomal hernia repair by using 3-D textile implants. JSLS. 2014; 18:pii: e2014.00034.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download