Abstract
Purpose
We aimed to retrospectively evaluate the risk factors for hypertensive attack during adrenalectomy in patients with pheochromocytoma. Despite the development of newer surgical and anesthetic techniques for the management of pheochromocytoma, intraoperative hypertensive attack continues to present a challenge.
Materials and Methods
Data from 53 patients diagnosed with pheochromocytoma at Kyungpook National Uriversity Medical Center between January 2000 and June 2012 were retrospectively analyzed. The subjects were divided into 2 groups depending on the presence or absence of hypertensive attack at the time of surgery. Patient demographic characteristics and preoperative evaluations were assessed for their prognostic relevance with respect to hypertensive attack. A univariate analysis was conducted, and a multivariate logistic regression analysis was also performed.
Results
In the univariate analysis, systolic blood pressure at presentation, preoperative hormonal status (including epinephrine, norepinephrine, vanillylmandelic acid, and metanephrine levels in a 24-hour urine sample), tumor size, and postoperative systolic blood pressure were significantly associated with the development of hypertensive attack. In the multivariate analysis, preoperative epinephrine level and tumor size were independent factors that predicted hypertensive attack. The highest odds ratio for tumor size (2.169) was obtained at a cutoff value of 4.25 cm and the highest odds ratio for preoperative epinephrine (1.020) was obtained at a cutoff value of 166.3 µg/d.
Pheochromocytoma is a tumor of the catecholamine-producing cells of the adrenal medulla. The unregulated secretion of catecholamines can cause hypertension, palpitations, and headaches. Patients with pheochromocytoma may develop myocardial infarction, cerebral vascular accidents, acute renal failure, and in rare cases acute respiratory distress syndrome [1].
Most patients diagnosed with pheochromocytoma will require surgical resection of the adrenal gland [23]. Historically, the surgical mortality rate for patients with pheochromocytoma has been high owing to a lack of adequate monitoring for hypertensive crises [456]. However, improvements in preoperative management and in surgical and anesthetic techniques have led to decreases in perioperative mortality for patients undergoing surgical resection for pheochromocytoma [78]. The recent development of and widespread experience with techniques involving a laparoscopic approach have resulted in the establishment of laparoscopic adrenalectomy as the standard treatment for adrenal tumors [9101112]. Despite the aforementioned advances, however, intraoperative hypertensive crises continue to occur.
Accordingly, in the present study, we performed a retrospective evaluation of the risk factors for hypertensive attack during adrenalectomy for pheochromocytoma.
We retrospectively analyzed 53 consecutive patients with pheochromocytoma who underwent unilateral adrenalectomy (either open or laparoscopic) from January 2000 to June 2012 at Kyungpook National Uriversity Medical Center. Patients were divided into 2 groups depending on the presence or absence of hypertensive attack at the time of surgery. The surgical approach in each case was based on the preferences of both the patient and the surgeons. Surgery was performed by an experienced surgeon in all cases. The choice of surgical procedure was based on referrals and surgeon preference.
The diagnosis of pheochromocytoma was based on clinical manifestations, levels of plasma catecholamines and urine methoxylated derivatives, and computed tomography or nuclear magnetic resonance imaging findings. Patients diagnosed with pheochromocytoma and administered the antihypertensive drug doxazosin for at least 2 weeks before adrenalectomy to achieve normalization of blood pressure irrespective of previous hypertension history were included in the study. Adequate pretreatment was defined by a target blood pressure of 130/85 mmHg [13].
Intraoperatively, systolic and diastolic arterial blood pressure and heart rate values were automatically, continuously, and digitally recorded by invasive measurement through an arterial line in the radial artery. Central venous pressure was monitored in all patients. Systolic arterial pressure (SAP)>160 mmHg was treated with intravenous boluses of nicardipine 2–4 mg to maintain SAP between 120 and 160 mmHg. Intravenous boluses of esmolol 1–1.5 mg/kg were used if the heart rate exceeded 100 beats/min.
Laparoscopic adrenalectomy was performed by an anterior transperitoneal approach in all cases. Pneumoperitoneum was achieved by using a Veress needle, and three or four ports were inserted into the abdominal cavity with the patient in the semilateral position. For a left adrenal tumor, the phrenocolic ligament was incised and the peritoneal incision was extended transversely beside the transverse colon and vertically along the spleen and descending colon. The next step was lateral dissection of the spleen. Dissection was continued up to the diaphragm close to the greater curvature of the stomach. After the spleen was completely mobilized, it fell away medially and opened the approach to the adrenal gland. After reflecting the colon, the adrenal vein was dissected out and transected. On the right side, a wide incision of the peritoneum was made and the right hepatic triangular ligament was mobilized. Dissection continued up to the diaphragm, allowing more effective medial retraction of the liver. After the adrenal gland was dissected, the adrenal vein was transected. The lower pole of the gland was lifted, and the several small arteries and veins in this region were dissected. The lateral side of the adrenal gland was then separated from the perinephric fat, followed by separation of the upper pole from the diaphragm in the same way. The upper medial part of the adrenal gland was separated from the surrounding structures. All procedures were performed without touching the adrenal mass if possible.
Open adrenalectomy was performed through either a flank or a subcostal incision. Subcutaneous tissue and abdominal muscle were dissected and divided. After blunt dissection of the pararenal space, the peritoneum was incised, and the posterior peritoneum and Gerota's fascia were divided. On approach to the adrenal vein area, the adrenal vein was ligated and cut, and then the adrenal gland was dissected. All procedures were performed without touching the adrenal mass if possible.
Demographic characteristics of the patients and preoperative evaluations were assessed for their prognostic relevance for intraoperative hemodynamic fluctuation. The variables considered were age, sex, body mass index (BMI), the presence or absence of symptoms, American Society of Anesthesiologists (ASA) score, underlying disease, tumor laterality, mean tumor size, surgical approach, treatment with antihypertensive medication, and mean duration of hypertension. Both preoperative blood pressure and hormonal status were evaluated as risk factors.
Hypertension was defined as a systolic blood pressure>140 mmHg or a diastolic blood pressure>90 mmHg. Hypertensive attack was defined as a systolic blood pressure>180 mmHg at any time during surgery. Postoperative hypertension was assessed approximately 1 to 2 weeks after surgery, and fractionated catecholamines and metanephrines were measured by collection of a 24-hour urine specimen.
Statistical analyses were conducted to determine the prognostic relevance of preoperative factors for hypertensive attack. Continuous variables were compared by using independent Student t-tests, and categorical variables were assessed by use of chi-square tests. A multivariate logistic regression analysis was conducted to determine the independent risk factors affecting hypertensive attack, and receiver operating characteristic curve analyses were used to confirm the predictive value of the identified factors. All p-values were two-sided, and a value of p<0.05 was considered significant. Analyses were conducted by using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA).
Of the 53 patients diagnosed with pheochromocytoma, 28 were men and 25 were women. The patients' mean age was 47.5 years. The tumor affected the right and the left adrenal gland in 24 and 29 patients, respectively. The mean tumor size was 5.6 cm and the mean patient BMI was 23.3 kg/m2. Twenty-five patients had preoperative symptoms such as headaches, palpitations, or cold sweats. A laparoscopic approach was used for 44 patients and an open approach was used for 9 patients. Forty-two patients had been treated with antihypertensive medications for over 3 months before undergoing adrenalectomy. In contrast, 11 patients diagnosed with pheochromocytoma following adrenalectomy had normal blood pressure and did not undergo management of hypertension but had been administered the antihypertensive drug doxazosin for at least 2 weeks before adrenalectomy.
The hypertensive attack group (HA group) and the non-hypertensive-attack group (non-HA group) included 33 and 20 patients, respectively. The 2 groups did not differ significantly in age, sex, or BMI. Additionally, patient characteristics such as the presence or absence of preoperative symptoms, ASA score, presence of diabetes mellitus and/or coronary vascular disease, tumor laterality, surgical approach, preoperative hypertensive medications, mean duration of hypertensive management, and postoperative complications also did not differ statistically between the groups. Mean tumor size was significantly correlated with HA (Table 1).
Systolic blood pressure at presentation was significantly different between the HA and non-HA groups, although no significant differences were found in diastolic blood pressure at presentation or in systolic and diastolic blood pressure after antihypertensive pharmacotherapy (alpha-blocker). Whether hypertension was controlled through antihypertensive pharmacotherapy before surgery was also not significantly different between the groups. Indicators of patient preoperative hormonal status, including levels of epinephrine, norepinephrine, vanillylmandelic acid, and metanephrine from a 24-hour urine specimen, were higher in the HA group, with the exception of serum dopamine (Table 2).
The rate of complications did not differ significantly between the HA and non-HA groups. Additionally, no major complications required conversion to an open procedure or reoperation. We graded the complications according to the classification system suggested by Clavien et al. [14].
Of the investigated risk factors, systolic blood pressure at presentation, preoperative hormonal status (including epinephrine, norepinephrine, vanillylmandelic acid, and metanephrine from a 24-hour urine specimen), and tumor size were found to be significantly associated with the development of hypertensive attack according to the results of a univariate analysis (Tables 1 and 2). A multivariate analysis revealed that preoperative epinephrine and tumor size were the independent factors associated with hemodynamic fluctuation (Table 3).
With regard to tumor size as a predictor of intraoperative hypertensive attack, the highest odds ratio (2.169) was obtained at a cutoff value of 4.25 cm, and the sensitivity and specificity at this cutoff were 87.9% and 85.0%, respectively, with an area under the curve (AUC) of 0.823. Regarding preoperative epinephrine, the highest odds ratio (1.020) was obtained at a cutoff value of 166.3 µg/day, and the sensitivity and specificity at this cutoff were 75.8% and 100%, respectively, with an AUC of 0.874 (Fig. 1).
Pheochromocytoma is found in approximately 0.1%–0.3% of patients with hypertension [1], and surgical management is required for blood pressure control in these cases. The high perioperative mortality rate associated with pheochromocytoma has been widely recognized, and surgical procedures to alleviate pheochromocytoma have even been considered life threatening due to hypertensive attack and multiorgan failure. Recently, minimally invasive approaches (i.e., laparoscopy) have provided effective and safe adrenalectomy results, whereas anesthetic care has been improved through the increasing variety of anesthetic techniques and drugs. Accordingly, the perioperative mortality rates for pheochromocytoma resection have decreased from 20% in 1951 to 2%–4% recently [15]. Although the operative and anesthetic techniques have undergone improvements, significant intraoperative hemodynamic changes continue to occur [16171819]. The results of several studies have indicated that the incidence of hemodynamic fluctuation ranges from 39.1% to 100% [20]. However, only a few studies have explored the risk factors for intraoperative fluctuation.
Kinney et al. [21] analyzed predictive factors for perioperative marked hypertensive events in pheochromocytoma. Perioperative events, such as episodic periods of marked hypertension, were found to be related to tumor size and catecholamine activity. It is likely that large tumors required increased manipulation during tumor dissection and resection, resulting in high catecholamine release and significant hemodynamic fluctuation.
In another study, Scholten et al. [22] compared patients with non-multiple endocrine neoplasia (non-MEN) and MEN type 2-related pheochromocytoma to assess risk factors for hemodynamic instability. In a multivariate analysis, those authors found tumor size to be an independent risk factor for the total group.
Bruynzeel et al. [23] reported that a high plasma norepinephrine concentration and large tumor size were risk factors for hemodynamic instability during surgery for pheochromocytoma. This result suggested that intraoperative catecholamine release due to anesthesia and tumor manipulation was related to tumor size.
The results described by Tauzin-Fin et al. [24] suggested that perioperative treatment with an alpha-blocker was effective in providing hemodynamic control during surgery for pheochromocytoma. However, a correlation between hypertensive events and plasma catecholamine levels was not detected. Kocak et al. [25] reported that pretreatment with any type of alpha-blocker affected intraoperative and postoperative blood pressure.
Yang et al. [26] analyzed the characteristics of perioperative hemodynamics in pheochromocytoma secreting different types of catecholamine. Patients with highly epinephrinesecreting pheochromocytoma were shown to be prone to have larger blood fluctuations during the operation. Patients with highly norepinephrine- and dopamine-secreting pheochromocytoma were shown to be liable to suffer from persisting postoperative hypotension.
In the present study, higher levels of preoperative urinary catecholamines or metabolites, with the exception of dopamine, were found to be associated with hypertensive attack in a univariate analysis. A multivariate analysis showed that preoperative epinephrine was a strong risk factor (odds ratio [OR], 1.020, p=0.027). Furthermore, the mean tumor size was found to be larger in the HA group than in the non-HA group. In the multivariate analysis, mean tumor size was identified as a significant risk factor for the development of intraoperative hypertensive attack (OR, 2.169; p=0.045). Both systolic and diastolic blood pressure at presentation were also found to be significant risk factors in the univariate analysis. However, these variables were not significant risk factors in the multivariate analysis.
Desmonts and Marty [27] suggested two potential causes of hypertensive attack during pheochromocytoma resection. First, noxious stimuli, such as intubation and skin incision, induce catecholamine release from excessive stores in adrenergic nerve endings. Additionally, tumor manipulation itself can produce hemodynamic fluctuation. Therefore, careful surgical handling of the tumor is necessary to prevent a hypertensive response.
Guerrero et al. [28] showed that tumor size is directly correlated with hormone levels such that smaller tumors have a tendency to secrete lower levels of catecholamines and larger tumors have the highest hormonal ratios, although these ratios are associated with wide ranges of secretory variation.
Kiernan et al. [29] evaluated predictors of hemodynamic instability during surgery for pheochromocytoma. In that study, tumor size, operative approach, and selective alphablockade were associated with intraoperative hemodynamic instability during pheochromocytoma resection.
In the current study, tumor size and preoperative epinephrine were associated with intraoperative hypertensive attack. These findings are likely attributable to the high probability of tumor manipulation during resection of large tumors and the ability of large tumors to produce and secrete high levels of hormones.
The limitations of the current study included its retrospective design and the relatively small sample sizes observed at our institution. Therefore, the study results may not fully or definitively elucidate all possible risk factors for hypertensive attack during the performance of adrenalectomy in patients with pheochromocytoma. In addition, we investigated clinical factors that affect intraoperative systolic blood pressure above 180 mmHg. Increasing systolic blood pressure above 180 mmHg during pheochromocytoma operation may be common as indicated in the present study. Usually, intraoperative temporal blood pressure above 180 mmHg may be safely managed by most anesthesiologists. We hardly ever experienced ventricular fibrillation, pulseless ventricular tachycardia, or uncontrollable hypertension during operation for pheochromocytoma. However, our study has significance considering that there are currently no reports related to the risk factors for hypertensive attack during adrenalectomy in Korea.
In the current study, large tumor size and higher preoperative urinary epinephrine levels were found to be risk factors for intraoperative hypertensive attack in patients with pheochromocytoma. These results may help urologists and anesthesiologists provide patients with more accurate expectations regarding surgical hemodynamic instability. Furthermore, these study results strongly suggest that pheochromocytoma is an aggressive disease requiring intensive intraoperative care.
Figures and Tables
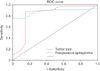 | Fig. 1Receiver operating characteristic (ROC) curve of multiple cutoff values of tumor size and preoperative epinephrine. |
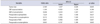
Table 1
Characteristics of pheochromocytoma patients in the HA and non-HA groups

Table 2
Perioperative blood pressure and urinary catecholamines and catecholamine metabolites in the HA and non-HA groups

Table 3
Prognostic factors for the development of hypertensive attack in patients undergoing adrenalectomy for pheochromocytoma (multivariate logistic regression analysis)
References
1. Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005; 366:665–675.
2. Plouin PF, Duclos JM, Soppelsa F, Boublil G, Chatellier G. Factors associated with perioperative morbidity and mortality in patients with pheochromocytoma: analysis of 165 operations at a single center. J Clin Endocrinol Metab. 2001; 86:1480–1486.
3. Manger WM, Gifford RW Jr, Hoffman BB. Pheochromocytoma: a clinical and experimental overview. Curr Probl Cancer. 1985; 9:1–89.
4. Lo CY, van Heerden JA, Grant CS, Soreide JA, Warner MA, Ilstrup DM. Adrenal surgery in the elderly: too risky? World J Surg. 1996; 20:368–373.
5. Sutton MG, Sheps SG, Lie JT. Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin Proc. 1981; 56:354–360.
6. Apgar V, Papper EM. Pheochromocytoma. Anesthetic management during surgical treatment. AMA Arch Surg. 1951; 62:634–648.
7. van Heerden JA. First encounters with pheochromocytoma. The story of Mother Joachim. Am J Surg. 1982; 144:277–279.
8. van Heerden JA, Roland CF, Carney JA, Sheps SG, Grant CS. Long-term evaluation following resection of apparently benign pheochromocytoma(s)/paraganglioma(s). World J Surg. 1990; 14:325–329.
9. Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992; 327:1033.
10. Smith CD, Weber CJ, Amerson JR. Laparoscopic adrenalectomy: new gold standard. World J Surg. 1999; 23:389–396.
11. Duh QY, Siperstein AE, Clark OH, Schecter WP, Horn JK, Harrison MR, et al. Laparoscopic adrenalectomy. Comparison of the lateral and posterior approaches. Arch Surg. 1996; 131:870–875.
12. Brunt LM, Doherty GM, Norton JA, Soper NJ, Quasebarth MA, Moley JF. Laparoscopic adrenalectomy compared to open adrenalectomy for benign adrenal neoplasms. J Am Coll Surg. 1996; 183:1–10.
13. Pacak K. Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab. 2007; 92:4069–4079.
14. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.
15. Saegesser F. César Roux (1857-1934) and his times. Rev Med Suisse Romande. 1984; 104:403–464.
16. Winfield HN, Hamilton BD, Bravo EL, Novick AC. Laparoscopic adrenalectomy: the preferred choice? A comparison to open adrenalectomy. J Urol. 1998; 160:325–329.
17. Suzuki K, Kageyama S, Hirano Y, Ushiyama T, Rajamahanty S, Fujita K. Comparison of 3 surgical approaches to laparoscopic adrenalectomy: a nonrandomized, background matched analysis. J Urol. 2001; 166:437–443.
18. Bonjer HJ, Sorm V, Berends FJ, Kazemier G, Steyerberg EW, de Herder WW, et al. Endoscopic retroperitoneal adrenalectomy: lessons learned from 111 consecutive cases. Ann Surg. 2000; 232:796–803.
19. Suzuki K, Ushiyama T, Ihara H, Kageyama S, Mugiya S, Fujita K. Complications of laparoscopic adrenalectomy in 75 patients treated by the same surgeon. Eur Urol. 1999; 36:40–47.
20. Zhang X, Lang B, Ouyang JZ, Fu B, Zhang J, Xu K, et al. Retroperitoneoscopic adrenalectomy without previous control of adrenal vein is feasible and safe for pheochromocytoma. Urology. 2007; 69:849–853.
21. Kinney MA, Warner ME, vanHeerden JA, Horlocker TT, Young WF Jr, Schroeder DR, et al. Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesth Analg. 2000; 91:1118–1123.
22. Scholten A, Vriens MR, Cromheecke GJ, Borel Rinkes IH, Valk GD. Hemodynamic instability during resection of pheochromocytoma in MEN versus non-MEN patients. Eur J Endocrinol. 2011; 165:91–96.
23. Bruynzeel H, Feelders RA, Groenland TH, van den Meiracker AH, van Eijck CH, Lange JF, et al. Risk factors for hemodynamic instability during surgery for pheochromocytoma. J Clin Endocrinol Metab. 2010; 95:678–685.
24. Tauzin-Fin P, Sesay M, Gosse P, Ballanger P. Effects of perioperative alpha1 block on haemodynamic control during laparoscopic surgery for phaeochromocytoma. Br J Anaesth. 2004; 92:512–517.
25. Kocak S, Aydintug S, Canakci N. Alpha blockade in preoperative preparation of patients with pheochromocytomas. Int Surg. 2002; 87:191–194.
26. Yang RL, Liu DW, Long Y, Shi Y, Chai WZ, Li HZ, et al. Perioperative hemodynamics in pheochromocytoma secreting different types of catecholamine. Zhonghua Yi Xue Za Zhi. 2008; 88:816–819.
27. Desmonts JM, Marty J. Anaesthetic management of patients with phaeochromocytoma. Br J Anaesth. 1984; 56:781–789.
28. Guerrero MA, Schreinemakers JM, Vriens MR, Suh I, Hwang J, Shen WT, et al. Clinical spectrum of pheochromocytoma. J Am Coll Surg. 2009; 209:727–732.
29. Kiernan CM, Du L, Chen X, Broome JT, Shi C, Peters MF, et al. Predictors of hemodynamic instability during surgery for pheochromocytoma. Ann Surg Oncol. 2014; 21:3865–3871.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download