Abstract
Active surveillance (AS) is a management strategy involving close monitoring the course of disease with the expectation to intervene if the cancer progress, in a super-selected group of low-risk prostate cancer (PCa) patients. Determining AS candidates should be based on careful individualized weighing of numerous factors: life expectancy, general health condition, disease characteristics, potential side effects of treatment, and patient preference. Several protocols have been developed to determine insignificant PCa for choosing ideal AS candidates. Results regarding disease reclassification during AS have been also reported. In an effort to enhance accuracy during selection of AS candidate, there were several reports on using magnetic resonance imaging for prediction of insignificant PCa. Currently, there is an urgent need for further clinical studies regarding the criteria for recommending AS, the criteria for reclassification on AS, and the schedule for AS. Considering the racial differences in behavior of PCa between Western and Asian populations, more stringent AS protocols for Asian patients should be established from additional, well-designed, large clinical studies.
Active surveillance (AS) is a management strategy in a superselect group of low-risk prostate cancer (PCa) patients involving close monitoring of the course of disease with the expectation to intervene if cancer progresses. By delaying intervention for indolent tumors and treating only when more clinically-significant PCa is detected, AS minimizes overtreatment. Compared with watchful waiting, which involves monitoring the course of PCa with the expectation of delivering palliative therapy for development of symptoms, change in exam, or prostate specific antigen (PSA) that suggests symptoms are imminent, AS is mainly applicable to younger men with seemingly indolent cancer, with the goal of deferring treatment and its potential side effects (Table 1). Because such patients have a longer life expectancy, they should be followed closely, and treatment should start promptly before the cancer progresses so as not to miss the chance for cure.
Such a unique concept of treatment is based on concerns about overdiagnosis and overtreatment related to the increased diagnosis of PCa due to the widespread use of PSA for early detection or screening. The debate regarding the need to diagnose and treat every man with PCa is originated from: the high prevalence of PCa on prostate autopsy and the discrepancy between incidence and mortality rates of PCa [1234]. The controversy regarding the value of PSA screening for early detection of PCa [3456789] was emphasized by the Goteborg study, a subset of the European Randomized Study for Screening of Prostate Cancer (ERSPC) [10]. Although the study showed a 40% absolute cumulative risk reduction of PCa mortality (compared to ERSPC 20% and PLCO [Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial] 0%), 293 men needed to obtain screening visits and 12 needed to be diagnosed in order to prevent one PCa death. Moreover, the estimated probability of overtreatment ranged from 23% to 42% of all screen-detected cancers [11], and cancer detection was responsible for up to 12.3 years of lead-time bias [12].
In the 2015 National Comprehensive Cancer Network (NCCN) guidelines, AS is recommended in men with very-low-risk PCa (T1c, Gleason score [GS]≤6, PSA<10 ng/mL, fewer than three biopsy cores positive, ≤50% cancer in any core, PSA density [PSAD]<0.15 ng/mL/g) and life expectancy ≤20 years. The European Association of Urology guidelines [13] are similar: clinically confined PCa (T1-T2), GS≤6, three or fewer biopsies involved with cancer, ≤50% of each biopsy involved with cancer, and PSA<10 ng/mL.
The NCCN recommendation for follow-up schedule during AS includes PSA no more often than every 6 months unless clinically indicated, digital rectal examination (DRE) no more often than every 12 months unless clinically indicated, and repeat prostate biopsy considered annually to assess for disease progression (Biopsy should be repeated within 6 months of diagnosis if initial biopsy was <10 cores or assessment discordant; for example, palpable tumor contralateral to the side of positive biopsy). A repeat prostate biopsy is indicated when DRE change or PSA increase, although neither parameter is very reliable for detecting PCa progression.
The panel recommends starting intervention when GS 4 or 5 cancer is found upon repeat prostate biopsy, when PCa is found in a greater number of prostate biopsies, or when PCa occupies a greater extent of the prostate biopsy, as these findings are regarded as cancer progression. Different criteria have been applied to define cancer progression [14], although most groups used the following criteria: PSA-doubling time (DT) with a cutoff ranging between ≤2 and ≤4 years, GS progression to ≤7 at rebiopsy (at intervals ranging from 1 to 4 years), PSA progression >10 ng/mL, although the role of PSA-DT in identifying the need for intervention has recently been challenged [151617].
The advantages of AS include: (1) avoiding the side effects of definitive therapy that may not be necessary; (2) maintaining quality of life and normal activities; (3) minimizing the risk of unnecessary treatment for small, indolent cancers; and (4) low initial costs. The disadvantages of AS include: (1) possibility of missing an opportunity for cure; (2) possibility of progression or metastasis of the cancer before treatment; (3) increased difficulty in the treatment of more aggressive cancer with greater side effects; (4) increased difficulty of the nerve-sparing technique during radical prostatectomy; (5) increased anxiety of living with untreated cancer; (6) need to examine and undergo frequent prostate biopsies; (7) uncertain long-term natural history of untreated PCa; and (8) undetermined timing and value of periodic imaging studies.
Patients with insignificant PCa might be ideal AS candidates, considering its indolent nature. Currently, there are no biological markers to clearly differentiate tumors that will progress or be indolent. Hence, statistical models have been developed to predict tumor aggressiveness. Epstein et al. [1819] suggested a model using preoperative clinical and pathologic features that can predict "insignificant PCa" (tumor volume<0.2 mL, GS<7, and organ-confined tumor). The preoperative parameters used in this model include no GS 4 or 5 in biopsy pathology, PSAD≤0.1 ng/mL/g, less than three involved biopsy cores (with a minimum of six total cores being obtained), no core with >50% involvement or PSAD of 0.1 to 0.15 ng/mL/g, and cancer <3 mm in only one prostate biopsy core specimen. Stamey et al. [20] proposed that tumors <0.5 mL could probably be regarded as insignificant with respect to the long DT. Recently, Wolters et al. [21] challenged this widely accepted definition of insignificant PCa. The authors reported that clinically insignificant PCa might include index GS 6 and pT2 disease with index volume ≤1.3 mL and total volume ≤2.5 mL.
An appropriate, reliable definition of "insignificant PCa" is crucial for the following reasons. If the definition is too stringent, a significant proportion of insignificant PCa patients would be ineligible for AS and become the object of unnecessary intervention [22]. Conversely, without a stringent definition, treatment of low-risk PCa could probably be suboptimal, especially in this era of robotic surgery and focal therapies with relatively low morbidities.
However, there are numerous studies reporting the risks of unfavorable pathological features such as upgrading of GS and pathologic upstaging in prostatectomy specimens from patients who were initially regarded as having insignificant PCa according to preoperative Epstein criteria; the frequency of such features ranged from 16% to 42% [23]. The risk of GS upgrading was approximately 30% in a previous meta-analysis [24]. Other series [2526] have shown that up to 8% of cancers that qualified as being insignificant according to the Epstein criteria were not organ-confined in the postoperative pathologic reports.
These findings suggested the need for caution against using this protocol as it is, and many variations regarding this definition have been suggested (reviewed by Bastian et al. [27]).
Several contemporary AS protocols are shown in Table 2 from Johns Hopkins Medical Institution (JHMI) [28], Memorial Sloan-Kettering Cancer Center (MSKCC) [29], University of California at San Francisco (UCSF) [30], Prostate Cancer Research International: Active Surveillance (PRIAS) [31], University of Miami (UM) [32], and One Asian protocol [33].
During AS, some of patients in the favorable-risk group are at risk, owing to pre-existing higher-risk disease that was not obvious at initial diagnosis or to disease progression over time. These patients can be detected by close monitoring such as serial measurement of PSA value or prostate biopsy and reclassified into the higher-risk group.
The Toronto group, JHMI group, and UCSF group recently reported the follow-up results of their AS patients (Table 3). Approximately one-third of these patients were reclassified as higher-risk and treated over time. The PCa mortality was quite low in an intermediate time frame (5-10 years). As for the active treatments during AS, radical prostatectomy or radiation therapy +/- androgen deprivation therapy was performed. In the Toronto group, the 5-year biochemical recurrence-free survival rates in the surgery and radiation treatment groups were only 62% and 43%, respectively. However, in the Johns Hopkins group [31], the 5-year biochemical recurrence-free survival rates were 96% and 75% for the surgery and radiation treatment groups, respectively. In addition, Ha et al. [36] reported their early experience with AS. They concluded PSA-DT was not associated with cancer progression, suggesting the need to perform regular prostate biopsy. They also emphasized that application of AS strategy to Korean patients should carry very careful considerations.
Considering the clinicopathological differences in PCa between Western and Korean populations [37], there have been concerns about the validity of Western AS protocols in Korean PCa patients [3839]. Kim et al. [38] evaluated several Western AS protocols by applying these protocols to their RP series and compared the pre- and postoperative pathologic characteristics. Of 1,006 patients, GS upgrading occurred in 41.6% to 50.6%, extracapsular extension in 4.1% to 8.5%, seminal vesicle invasion in 0.5% to 1.6%, pathologic upstaging in 4.5% to 9.3%, and misclassification in 44.5% to 54.8% of patients. These data suggest the possibility of underestimation of Korean PCa by current Western AS protocols.
Several studies have compared the current Western AS protocols to determine their reliability [224041424344]. Lee et al. [44] analyzed several contemporary AS protocols (from JHMI, UCSF, MSKCC, UM, and PRIAS) with regard to sensitivity, specificity, and accuracy in order to determine the validity of these criteria for Korean PCa patients. According to their analysis, the PRIAS protocol was most appropriate among five Western protocol for Korean men to determine AS candidates.
In 2013, Lim et al. [45] suggested new AS criteria for Korean patients: cT1-cT2, GS≤6, PSA≤10 ng/mL, ≤1 positive biopsy core, and ≤50% core involvement. KaKehi et al. [33] developed AS protocols for Japanese patients: T1c, PSA≤20 ng/mL, ≤2 positive cores, GS≤6, and ≤50% cancer involvement in any of the positive cores. Goto et al. [43] reported that the JHMI and PRIAS criteria were most helpful for use in Japanese Pca patients. In addition, Jin et al. [46] reported the strong correlation between PSAD and GS upgrading after RP, emphasizing the use of PSAD for choosing ideal AS candidates. According to their analysis, the optimal PSAD cutoff value was 0.13 ng/mL2.
In an effort to enhance accuracy during selection of AS candidates, there have been several reports on the use of magnetic resonance imaging (MRI) for prediction of insignificant PCa. Some authors [4748] have reported that the use of apparent diffusion coefficient from diffusion-weighted magnetic resonance imaging (DW-MRI) might be helpful for choosing AS candidates. Early experience supports the use of multiparametric MRI in biopsy protocols for better risk-stratification of patients on AS [4950]. Recently, Park et al. [51] reported associations between adverse pathological features in PCa patients eligible for AS and clear tumor identification on 3.0-T multiparametric MRI (combination of T2WI, DCEI, and DWI). Lee et al. [52] reported preliminary results that a simple measurement of the diameter of a suspicious tumor lesion on DW-MRI improves the prediction of insignificant PCa. According to their study, the possibility of insignificant Pca increased when tumor diameter was smaller than 1 cm.
Determination of AS candidates should be based on careful individualized weighing of numerous factors: life expectancy, general health condition, disease characteristics, potential side effects of treatment, and patient preference. The timing of intervention should be based on change in PSA or pathology or clinical disease progression. Patients with clinically localized PCa who are candidates for definitive treatment but choose AS should undergo regular follow-up. In addition, follow-up should be more rigorous in younger men than in older men due to the higher life expectancy in the former group.
Currently, NCCN panels emphasize the urgent need for further clinical studies regarding the criteria for recommending AS, the criteria for reclassification on AS, and the schedule for AS, especially as it is associated with prostate biopsy, which unfortunately come within an increasing burden. Literatures report that up to 7% of men undergoing prostate biopsy will experience side effects [7], those with urinary tract infection are often quinoloneresistant [53], and surgery may become difficult after multiple prostate biopsies [54].
Considering the racial differences in behavior of PCa between Western and Asian populations, more stringent AS protocols for Asian patients should be established from additional, well-designed, large clinical studies.
Figures and Tables
Table 1
Active surveillance versus watchful waiting

Table 2
Contemporary active surveillance protocols
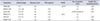
| Institution | Clinical stage | Gleason score | PSA (ng/mL) | PSAD | No. of positive cores | Single core involvement (%) |
|---|---|---|---|---|---|---|
| JHMI [28] | T1c | ≤6 | - | ≤0.15 | ≤2 | ≤50 |
| MSKCC [29] | T1c-T2a | ≤6 | ≤10 | - | ≤3 | ≤50 |
| UCSF [30] | T1c-T2 | ≤6 | ≤10 | - | ≤33% (at least 6) | ≤50 |
| PRIAS [31] | T1c-T2 | ≤6 | ≤10 | ≤0.2 | ≤2 | - |
| UM [32] | T1c-T2 | ≤6 | ≤15 | - | ≤2 | ≤20 |
| Kakehi [33] | T1c | ≤6 | ≤20 | - | ≤2 | ≤50 |
Table 3
Reports on disease reclassification during active surveillance

| Variable | University of Toronto [34] | JHMI [28] | UCSF [35] |
|---|---|---|---|
| Median age (y) | 70 | 66 | 63 |
| No. of patients | 450 | 769 | 513 |
| Median follow-up (mo) | 6.8 | 2.7 | 3.6 |
| Conversion to intervention (%) | 30 | 33 | 24 |
| Median time to treatment (y) | - | 2.2 | 3.5 |
| Overall survival | 68 | 98 | 98 |
| Cancer-specific survival | 97 | 100 | 100 |
| Primary reason for treatment | |||
| PSA increase | 14a | - | 26b |
| GS change | 8 | 14 | 38 |
| Anxiety | 3 | 9 | 8 |
References
1. Sakr WA, Grignon DJ, Crissman JD, Heilbrun LK, Cassin BJ, Pontes JJ, et al. High grade prostatic intraepithelial neoplasia (HGPIN) and prostatic adenocarcinoma between the ages of 20-69: an autopsy study of 249 cases. In Vivo. 1994; 8:439–443.
2. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004; 350:2239–2246.
3. Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med. 2012; 366:981–990.
4. Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009; 360:1320–1328.
5. Klotz L. Active surveillance for prostate cancer: for whom? J Clin Oncol. 2005; 23:8165–8169.
6. Andriole GL, Crawford ED, Grubb RL 3rd, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009; 360:1310–1319.
7. Andriole GL, Bostwick DG, Brawley OW, Gomella LG, Marberger M, Montorsi F, et al. Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010; 362:1192–1202.
8. Andriole GL, Crawford ED, Grubb RL 3rd, Buys SS, Chia D, Church TR, et al. Prostate cancer screening in the randomized Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial: mortality results after 13 years of follow-up. J Natl Cancer Inst. 2012; 104:125–132.
9. Sandblom G, Varenhorst E, Rosell J, Lofman O, Carlsson P. Randomised prostate cancer screening trial: 20 year follow-up. BMJ. 2011; 342:d1539.
10. Hugosson J, Carlsson S, Aus G, Bergdahl S, Khatami A, Lodding P, et al. Mortality results from the Göteborg randomised population-based prostate-cancer screening trial. Lancet Oncol. 2010; 11:725–732.
11. Draisma G, Etzioni R, Tsodikov A, Mariotto A, Wever E, Gulati R, et al. Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst. 2009; 101:374–383.
12. Draisma G, Boer R, Otto SJ, van der Cruijsen IW, Damhuis RA, Schroder FH, et al. Lead times and overdetection due to prostate-specific antigen screening: estimates from the European Randomized Study of Screening for Prostate Cancer. J Natl Cancer Inst. 2003; 95:868–878.
13. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intentupdate 2013. Eur Urol. 2014; 65:124–137.
14. Klotz L. Active surveillance for prostate cancer: a review. Curr Urol Rep. 2010; 11:165–171.
15. Krakowsky Y, Loblaw A, Klotz L. Prostate cancer death of men treated with initial active surveillance: clinical and biochemical characteristics. J Urol. 2010; 184:131–135.
16. Al Otaibi M, Ross P, Fahmy N, Jeyaganth S, Trottier H, Sircar K, et al. Role of repeated biopsy of the prostate in predicting disease progression in patients with prostate cancer on active surveillance. Cancer. 2008; 113:286–292.
17. Ross AE, Loeb S, Landis P, Partin AW, Epstein JI, Kettermann A, et al. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J Clin Oncol. 2010; 28:2810–2816.
18. Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994; 271:368–374.
19. Epstein JI, Chan DW, Sokoll LJ, Walsh PC, Cox JL, Rittenhouse H, et al. Nonpalpable stage T1c prostate cancer: prediction of insignificant disease using free/total prostate specific antigen levels and needle biopsy findings. J Urol. 1998; 160(6 Pt 2):2407–2411.
20. Stamey TA, Freiha FS, McNeal JE, Redwine EA, Whittemore AS, Schmid HP. Localized prostate cancer. Relationship of tumor volume to clinical significance for treatment of prostate cancer. Cancer. 1993; 71:3 Suppl. 933–938.
21. Wolters T, Roobol MJ, van Leeuwen PJ, van den Bergh RC, Hoedemaeker RF, van Leenders GJ, et al. A critical analysis of the tumor volume threshold for clinically insignificant prostate cancer using a data set of a randomized screening trial. J Urol. 2011; 185:121–125.
22. Kane CJ, Im R, Amling CL, Presti JC Jr, Aronson WJ, Terris MK, et al. Outcomes after radical prostatectomy among men who are candidates for active surveillance: results from the SEARCH database. Urology. 2010; 76:695–700.
23. Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm MO, et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol. 2011; 60:291–303.
24. Cohen MS, Hanley RS, Kurteva T, Ruthazer R, Silverman ML, Sorcini A, et al. Comparing the Gleason prostate biopsy and Gleason prostatectomy grading system: the Lahey Clinic Medical Center experience and an international meta-analysis. Eur Urol. 2008; 54:371–381.
25. Jeldres C, Suardi N, Walz J, Hutterer GC, Ahyai S, Lattouf JB, et al. Validation of the contemporary epstein criteria for insignificant prostate cancer in European men. Eur Urol. 2008; 54:1306–1313.
26. Bastian PJ, Mangold LA, Epstein JI, Partin AW. Characteristics of insignificant clinical T1c prostate tumors: a contemporary analysis. Cancer. 2004; 101:2001–2005.
27. Bastian PJ, Carter BH, Bjartell A, Seitz M, Stanislaus P, Montorsi F, et al. Insignificant prostate cancer and active surveillance: from definition to clinical implications. Eur Urol. 2009; 55:1321–1330.
28. Tosoian JJ, Trock BJ, Landis P, Feng Z, Epstein JI, Partin AW, et al. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. J Clin Oncol. 2011; 29:2185–2190.
29. Adamy A, Yee DS, Matsushita K, Maschino A, Cronin A, Vickers A, et al. Role of prostate specific antigen and immediate confirmatory biopsy in predicting progression during active surveillance for low risk prostate cancer. J Urol. 2011; 185:477–482.
30. Whitson JM, Porten SP, Hilton JF, Cowan JE, Perez N, Cooperberg MR, et al. The relationship between prostate specific antigen change and biopsy progression in patients on active surveillance for prostate cancer. J Urol. 2011; 185:1656–1660.
31. van den Bergh RC, Roemeling S, Roobol MJ, Aus G, Hugosson J, Rannikko AS, et al. Outcomes of men with screen-detected prostate cancer eligible for active surveillance who were managed expectantly. Eur Urol. 2009; 55:1–8.
32. Soloway MS, Soloway CT, Eldefrawy A, Acosta K, Kava B, Manoharan M. Careful selection and close monitoring of low-risk prostate cancer patients on active surveillance minimizes the need for treatment. Eur Urol. 2010; 58:831–835.
33. Kakehi Y, Kamoto T, Shiraishi T, Ogawa O, Suzukamo Y, Fukuhara S, et al. Prospective evaluation of selection criteria for active surveillance in Japanese patients with stage T1cN0M0 prostate cancer. Jpn J Clin Oncol. 2008; 38:122–128.
34. Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol. 2010; 28:126–131.
35. Dall'Era MA, Konety BR, Cowan JE, Shinohara K, Stauf F, Cooperberg MR, et al. Active surveillance for the management of prostate cancer in a contemporary cohort. Cancer. 2008; 112:2664–2670.
36. Ha JY, Kim BH, Park CH, Kim CI. Early experience with active surveillance in low-risk prostate cancer treated. Korean J Urol. 2014; 55:167–171.
37. Byun SS, Lee S, Lee SE, Lee E, Seo SI, Lee HM, et al. Recent changes in the clinicopathologic features of Korean men with prostate cancer: a comparison with Western populations. Yonsei Med J. 2012; 53:543–549.
38. Kim TH, Jeon HG, Choo SH, Jeong BC, Seo SI, Jeon SS, et al. Pathological upgrading and upstaging of patients eligible for active surveillance according to currently used protocols. Int J Urol. 2014; 21:377–381.
39. Choo SH, Jeon HG, Jeong BC, Seo SI, Jeon SS, Choi HY, et al. Predictive factors of unfavorable prostate cancer in patients who underwent prostatectomy but eligible for active surveillance. Prostate Int. 2014; 2:70–75.
40. Iremashvili V, Pelaez L, Manoharan M, Jorda M, Rosenberg DL, Soloway MS. Pathologic prostate cancer characteristics in patients eligible for active surveillance: a head-to-head comparison of contemporary protocols. Eur Urol. 2012; 62:462–468.
41. Sugimoto M, Shiraishi T, Tsunemori H, Demura T, Saito Y, Kamoto T, et al. Pathological findings at radical prostatectomy in Japanese prospective active surveillance cohort. Jpn J Clin Oncol. 2010; 40:973–979.
42. Mufarrij P, Sankin A, Godoy G, Lepor H. Pathologic outcomes of candidates for active surveillance undergoing radical prostatectomy. Urology. 2010; 76:689–692.
43. Goto Y, Nozumi K, Miyazaki K, Matsumoto A, Inoue A, Kito H, et al. Active surveillance criteria for prostate cancer: can they be applied to Japanese patients? Int J Urol. 2012; 19:163–166.
44. Lee DH, Jung HB, Lee SH, Rha KH, Choi YD, Hong SJ, et al. Comparison of pathological outcomes of active surveillance candidates who underwent radical prostatectomy using contemporary protocols at a high-volume Korean center. Jpn J Clin Oncol. 2012; 42:1079–1085.
45. Lim SK, Kim KH, Shin TY, Chung BH, Hong SJ, Choi YD, et al. Yonsei criteria: a new protocol for active surveillance in the era of robotic and local ablative surgeries. Clin Genitourin Cancer. 2013; 11:501–507.
46. Jin BS, Kang SH, Kim DY, Oh HG, Kim CI, Moon GH, et al. Pathological upgrading in prostate cancer patients eligible for active surveillance: does prostate-specific antigen density matter? Korean J Urol. 2015; 56:624–629.
47. Kim TH, Jeong JY, Lee SW, Kim CK, Park BK, Sung HH, et al. Diffusion-weighted magnetic resonance imaging for prediction of insignificant prostate cancer in potential candidates for active surveillance. Eur Radiol. 2015; 25:1786–1792.
48. Jeong CW, Park YH, Hwang SI, Lee S, Jeong SJ, Hong SK, et al. The role of 3-tesla diffusion-weighted magnetic resonance imaging in selecting prostate cancer patients for active surveillance. Prostate Int. 2014; 2:169–175.
49. Bonekamp D, Bonekamp S, Mullins JK, Epstein JI, Carter HB, Macura KJ. Multiparametric magnetic resonance imaging characterization of prostate lesions in the active surveillance population: incremental value of magnetic resonance imaging for prediction of disease reclassification. J Comput Assist Tomogr. 2013; 37:948–956.
50. Mullins JK, Bonekamp D, Landis P, Begum H, Partin AW, Epstein JI, et al. Multiparametric magnetic resonance imaging findings in men with low-risk prostate cancer followed using active surveillance. BJU Int. 2013; 111:1037–1045.
51. Park BH, Jeon HG, Choo SH, Jeong BC, Seo SI, Jeon SS, et al. Role of multiparametric 3.0-Tesla magnetic resonance imaging in patients with prostate cancer eligible for active surveillance. BJU Int. 2014; 113:864–870.
52. Lee DH, Koo KC, Lee SH, Rha KH, Choi YD, Hong SJ, et al. Tumor lesion diameter on diffusion weighted magnetic resonance imaging could help predict insignificant prostate cancer in patients eligible for active surveillance: preliminary analysis. J Urol. 2013; 190:1213–1217.
53. Feliciano J, Teper E, Ferrandino M, Macchia RJ, Blank W, Grunberger I, et al. The incidence of fluoroquinolone resistant infections after prostate biopsy: are fluoroquinolones still effective prophylaxis? J Urol. 2008; 179:952–955.
54. Fujita K, Landis P, McNeil BK, Pavlovich CP. Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance. J Urol. 2009; 182:2664–2669.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download