Abstract
Purpose
This article describes a novel technique for the repair of penile urethral strictures and establishes the safety, feasibility, and efficacy of this innovative surgical approach.
Materials and Methods
Patients with urethral strictures underwent a one-sided anterior dorsal oral mucosal graft urethroplasty through a penoscrotal inversion technique. The clinical outcome was considered a failure when any instrumentation was needed postoperatively, including dilatation.
Results
Five patients underwent the novel procedure. The patients' mean age was 58 years. The cause of stricture was instrumentation in 2 cases (40%), lichen sclerosis in 1 case (20%), and failed hypospadias repair in 2 cases (40%). The mean stricture length was 3 cm. The overall mean (range) follow-up was 6 months (range, 3–9 months). Of the 5 patients, 4 (80%) had a successful outcome and 1 (20%) had a failed outcome. The failure was successfully treated by use of a meatotomy.
The concept of developing an epithelialized tube from a buried strip of skin in the management of urethral strictures was first described by Duplay [1] and later Browne [2]. This principle is the foundation of urethral reconstruction. Johanson [3] used this principle in the management of urethral stricture in his description of a staged urethroplasty, which was later modified by Leadbetter Jr [4]. These principles are still considered to be the gold standard of management of penile urethral strictures, particularly complex strictures associated with failed urethroplasty, lichen sclerosis, and hypospadias.
In 1980, Monseur [5] described the first dorsal urethroplasty. In 1996, Barbagli et al. [6] expanded the technique by placing buccal mucosa into the dorsal defect. This surgical technique, although meant exclusively for the repair of bulbar urethral strictures, opened the door for further advancements in urethral reconstruction. In 2000, Kulkarni et al. [7] described a 1-stage buccal mucosal graft urethroplasty in patients with panurethral strictures due to lichen sclerosis. Asopa et al. [8] described a dorsal inlay technique 1 year later. These 1-stage techniques are becoming more commonly used by reconstructive experts and represent an alternative to traditional 2-stage repairs for penile urethral strictures.
The procedure described was performed between August 2014 and September 2015. The data were prospectively collected and retrospectively reviewed. Preoperative evaluation included history, physical examination, urine culture, postvoid residual urine measurements, uroflowmetry, and retrograde cystourethrography.
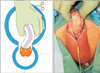
The patient was placed in a frog-leg supine position, with pillows under the knees for support. Compressive stockings and sequential compression devices were placed on the lower extremities. The skin of the suprapubic region and scrotum was shaved and this region was prepared and draped appropriately. The oral mucosal graft was harvested from the cheek according to the standard technique. A glans stitch was placed and used as a stay suture. A transverse incision was made at the penoscrotal junction (Fig. 1). A selfretaining retractor was used to aid the dissection. The dartos fascia was dissected off the underlying urethra and corpora. Once identified, the penis was inverted bluntly, although scissor dissection could be utilized when necessary (Fig. 2). Once the penis was fully inverted and the urethra exposed, a stay stitch was placed in the right side of the glans lateral to the urethra. Only the ventral side of the penis was degloved. Along the right side, the urethra remained attached to the corpora cavernosa for its full length, thus preserving its lateral vascular blood supply. The urethra was dissected and rolled off the underlying tunica albuginea of the corpora cavernosa from left to right in the region of the stricture (Fig. 3). Any circumflex vessels were secured with bipolar cautery. If the stricture extended to the meatus or fossa navicularis, the dissection was carried to the coronal sulcus.
When the stricture extended to the meatus, the penis was returned to its natural position and a dorsal urethrotomy was made along the glans and fossa navicularis (Fig. 4). The width of the urethrotomy should be 1 cm. The dorsal incision was carried as proximal as possible via the meatus. A catheter or forceps could be placed into the meatus as it was invaginated, and the dorsal incision was continued into the exposed urethra (Fig. 5). If the stricture did not involve the meatus or fossa navicularis, once the urethra had been rolled off the corpora, a catheter was placed to the level of the stricture and used as a guide to incise the dorsal urethra at the midline. The dorsal urethral incision was carried as proximal as necessary to expose the entire stricture. If there was hypospadias, the skin on the ventral side of the urethra often could not be dissected and therefore was left intact. The dorsal urethral plate could be sufficiently incised for graft placement by working from the distal and proximal end until 1 cm of albuginea was exposed. This was due to the short nature of the hypospadias cases described herein; longer hypospadias repairs would not allow this approach.
Once the entire stricture had been incised, the length and width of the remaining urethral plate were measured. The oral mucosal graft was trimmed to an appropriate size according to the length and width of the urethrotomy. If the meatus was involved, the graft was first sutured to the distal extent of the dorsal incision and quilted down in the region of the glans (Fig. 6). The graft was then tucked into the urethra and the penis was invaginated, at which point the graft was spread fixed over the underlying tunica (Fig. 7). The graft was quilted. The left margin of the graft was secured to the right lateral aspect of the exposed urethral plate. The right margin of the graft was sutured to the left margin of the urethral plate. A second layer was closed over the defect. If the meatus of the fossa navicularis was not involved, the graft could be placed in a standard dorsal onlay approach. There may be a small section where the graft cannot be reached to quilt, usually at the level of the fossa. Here, the options are to create a ventral meatotomy in order to quilt, or, as performed herein, to use surgical glue to secure this portion of the graft (Fig. 8). Once the glue was in place, a catheter was quickly passed into the urethra, and pressure was held for a time according to the recommendations of the glue being used. The remaining glue was used to secure the penile skin where it was dissected off the urethra (Fig. 9). The incision was then closed in a running, two-layer fashion. A final catheter was placed and left in situ for 3 weeks (Fig. 10). The patient was discharged on the same day of the procedure. All patients received lowdose suppressive antibiotics until the catheter was removed.
At 3 weeks after surgery, the bladder was filled with contrast, the catheter was removed, and voiding cystourethrography was obtained. Uroflowmetry and postvoid residual urine were repeated every 4 months for 1 year, then yearly. When symptoms of decreased force of stream were present and uroflowmetry was less than 10 mL/s, retrograde urethrography was performed.
Five patients (mean age, 58 years; range, 46–67 years) underwent a one-sided dorsal oral mucosal graft urethroplasty for penile urethral strictures through the penoscrotal inversion technique. The cause of stricture was previous urethral instrumentation in 2 cases (40%), lichen sclerosis in 1 case (20%), and hypospadias in 2 cases (40%). The mean stricture length was 3 cm (range, 2.5–5 cm). All 5 patients had received previous dilations or urethrotomies; 2 patients (the hypospadias patients) had undergone prior urethroplasties.
Mean follow-up was 6 months (range, 3–9 months). Clinical outcome was considered a failure if any postoperative instrumentation was needed, including dilation. In all patients, postoperative voiding cystourethrography was normal.
Of the 5 patients, 4 had successful outcomes and 1 had a failed outcome during the follow-up period. The one treatment failure was in a patient with a prior hypospadias repair. He had been performing self-dilation for several years before he researched the penile inversion approach to stricture repair. He was counseled on all the options, including a staged repair given the nature of his stricture; however, he elected to attempt to undergo the dorsal onlay approach. He developed a penile hematoma that became infected. Once the infection was drained and cleared, his catheter was removed, and a distal stricture recurred. Surprisingly, the graft was mostly intact, and he was managed with a short 0.5-cm meatotomy. One patient with a 5-cm lichen sclerosis stricture experienced postoperative chordee that has since resolved.
The success of the dorsal onlay technique, using a onesided dissection, for bulbar and panurethral strictures has been well described via a perineal incision [1011]. This is the first report of a penoscrotal incision to access the penile urethra for dorsal onlay graft urethroplasties. The potential advantages of this approach will be explored.
Because the penoscrotal inversion technique allows the patient to stay in the supine position, the complication of neurapraxia is theoretically the same as with any supine surgical procedure. By contrast, if the perineal incision is utilized, the peroneal nerve neurapraxia rate has been reported at 15.8% [1213]. In a second study, lower-extremity complications were reported at 10% [14]; this included a 6.5% neurapraxia rate, a 1% rate of rhabdomyolysis, and a 1% rate of compartment syndrome. More contemporary reports with improved positioning have shown a lower rate of these complications. For example, Whitson et al. [13] reported a series of 124 patients in low lithotomy with a neurapraxia rate of 3.4% and compartment syndrome seen in only 1 patient; complications were also noted to increase if the lithotomy position was over 5 hours. However, with the aforementioned supine approach, then this operation has clear advantages over approaching the stricture through a perineal incision.
A 1-stage repair has several advantages over a 2-stage repair. First, a patient must void through a proximal urethral defect or empty the bladder via a suprapubic tube after the first stage for some time until the urethra is stable enough for the second stage of repair. Second, a 2-stage repair is associated with a high revision rate. In a recent report on staged urethroplasty, only 56% underwent the retubularization procedure, 26% required revision of the first- or second-stage procedure, and the success rate was 90% (including those who underwent 1-stage repair) [15]. Others have demonstrated a 62% revision rate [16]. Finally, while the previous report noted a 90% success rate [15], others have not noted as much success with staged urethroplasty. A direct comparison between 1-stage buccal mucosal graft urethroplasty and 2-stage urethroplasty for long segment strictures showed a success rate of 83% versus 64% [11]. Traditionally, a staged repair was recommended for cases of lichen sclerosis. However, when the above authors reported their success in patients treated for lichen sclerosis with a 1-stage buccal mucosal repair versus a 2-stage operation, the success favored the 1-stage approach: 86% success versus 52%, respectively [11].
Penile skin complications are not uncommon after penile urethral stricture repairs. Fistula can occur in up to 3% to 20% of cases of fasciocutaneous flap urethroplasty [1718] and up to 10% of staged urethroplasty [16]. Patients who undergo a fasciocutaneous flap experience a higher rate of complications compared to buccal mucosal urethroplasty [11]. Complications include torsion, hematoma, sacculations, penile skin necrosis, complaints of irregular skin elevation, and penile skin scarring [1119]. Additional complications of 2-stage urethroplasty include 10% wound dehiscence and 5% wound infection or abscess [162021]. Using a penoscrotal approach limits skin complications of the penile urethra. One case in our series developed a penile hematoma that converted to an abscess requiring drainage. After this, we began to use surgical glue to secure the penile skin over the urethra after the repair was complete. Surgical glue has been shown to decrease wound complications in urethral reconstructions [22]. Since we started using the glue, we have had no additional cases of hematomas.
There were several limitations to the present report. The few numbers of patients and the short follow-up are clearly the limiting factors of this surgical approach. The idea of a penile inversion has been well described, although not through a penoscrotal approach. Although the advantages listed previously are present, they have not been fully tested with a large number of patients with long-term follow-up.
Next, for the most complicated urethral strictures, the use of 1-stage urethroplasty is not recommended. This includes previous failed urethroplasty and obliterated urethral strictures. Previously, lichen sclerosis was included on this list; however, Kulkarni et al. [10] has shown that onesided buccal mucosal urethroplasty is an effective treatment for cases of lichen sclerosis. Herein, we used the approach for a distal stricture associated with lichen sclerosis with success. There was one case of early postoperative chordee, but this has since resolved.
We also performed the procedure on 2 patients with failed hypospadias. Patient preference and the short nature of the strictures were the impetus for attempting the 1-stage approach. One case was successful, and the second had a distal recurrence at the level of the meatus, distal to the initial stricture site. The ventral dissection was not possible at the site of previous repair given the adherent nature of the penile skin to the underlying tubularized urethra. However, the length of the urethral stricture was short and therefore access to the dorsal plate was possible. The dorsal plate was opened sufficiently to allow passage and securing of the graft. One patient did fail distally at the meatus, requiring a 0.5-cm meatotomy. This was the same patient who experienced an infection. The original stricture site was intact and viable on last follow-up. The dorsal approach would not be possible in failed hypospadias if the stricture was longer or the prior hypospadias repair was longer. As a routine, the use of this approach would not be recommended in the setting of failed hypospadias.
Figures and Tables
References
1. Duplay S. Sur le traitment chirurgical de l'hypospadias et de l'epispadias. Arch Gen Med. 1880; 145:257–274.
2. Browne D. An operation for hypospadias. Proc R Soc Med. 1949; 42:466–468.
3. Johanson B. The reconstruction in stenosis of the male urethra. Z Urol. 1953; 46:361–375.
4. Leadbetter GW Jr. A simplified urethroplasty for strictures of the bulbous urethra. J Urol. 1960; 83:54–59.
5. Monseur J. Widening of the urethra using the supra-urethral layer (author's transl). J Urol (Paris). 1980; 86:439–449.
6. Barbagli G, Selli C, Tosto A, Palminteri E. Dorsal free graft urethroplasty. J Urol. 1996; 155:123–126.
7. Kulkarni S, Kulkarni J, Kirpekar D. A new technique of urethroplasty for balanitis xerotica obliterans [abstract]. J Urol. 2000; 163:Suppl. 352. Abstract No. V331.
8. Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology. 2001; 58:657–659.
9. Austoni E, Altieri VM, Tenaglia R. Trans-scrotal penile degloving, a new procedure for corporoplasties. Urologia. 2012; 79:200–210.
10. Kulkarni S, Barbagli G, Kirpekar D, Mirri F, Lazzeri M. Lichen sclerosus of the male genitalia and urethra: surgical options and results in a multicenter international experience with 215 patients. Eur Urol. 2009; 55:945–954.
11. Warner JN, Malkawi I, Dhradkeh M, Joshi PM, Kulkarni SB, Lazzeri M, et al. A multi-institutional evaluation of the management and outcomes of long-segment urethral strictures. Urology. 2015; 85:1483–1487.
12. Angermeier KW, Jordan GH. Complications of the exaggerated lithotomy position: a review of 177 cases. J Urol. 1994; 151:866–868.
13. Whitson JM, McAninch JW, Elliott SP, Alsikafi NF. Long-term efficacy of distal penile circular fasciocutaneous flaps for single stage reconstruction of complex anterior urethral stricture disease. J Urol. 2008; 179:2259–2264.
14. Anema JG, Morey AF, McAninch JW, Mario LA, Wessells H. Complications related to the high lithotomy position during urethral reconstruction. J Urol. 2000; 164:360–363.
15. Kozinn SI, Harty NJ, Zinman L, Buckley JC. Management of complex anterior urethral strictures with multistage buccal mucosa graft reconstruction. Urology. 2013; 82:718–722.
16. Andrich DE, Greenwell TJ, Mundy AR. The problems of penile urethroplasty with particular reference to 2-stage reconstructions. J Urol. 2003; 170:87–89.
17. Andrich DE, Dunglison N, Greenwell TJ, Mundy AR. The long-term results of urethroplasty. J Urol. 2003; 170:90–92.
18. Al-Qudah HS, Santucci RA. Extended complications of urethroplasty. Int Braz J Urol. 2005; 31:315–323.
19. Greenwell TJ, Venn SN, Mundy AR. Changing practice in anterior urethroplasty. BJU Int. 1999; 83:631–635.
20. Meeks JJ, Erickson BA, Fetchev P, Crawford SE, Fine NA, Gonzalez CM. Urethroplasty with abdominal skin grafts for long segment urethral strictures. J Urol. 2010; 183:1880–1884.
21. Joseph JV, Andrich DE, Leach CJ, Mundy AR. Urethroplasty for refractory anterior urethral stricture. J Urol. 2002; 167:127–129.
22. Morris MS, Morey AF, Stackhouse DA, Santucci RA. Fibrin sealant as tissue glue: preliminary experience in complex genital reconstructive surgery. Urology. 2006; 67:688–691.




 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download