Abstract
Purpose
To evaluate the safety and efficacy of ultrasound-guided percutaneous core needle biopsy of splenic lesions.
Materials and Methods
This retrospective study included 30 patients who underwent percutaneous core needle biopsy of their splenic lesions using 18- or 20-gauge needles between January 2001 and July 2016 in a single tertiary care center. The characteristics of the splenic lesions were determined by reviewing the ultrasound and computed tomography examinations. Acquisition rate and diagnostic accuracy were calculated, using pathologic results of the splenectomy specimen, clinical course and/or imaging follow-up as a reference standard. Post-procedure complications were identified from electronic medical records, laboratory findings and computed tomography images. Seventy-three specimens were obtained from the 30 patients and splenectomy was performed in 2 patients.
Figures and Tables
Fig. 1
A 66-year-old male with perisplenic hemorrhage after core needle biopsy.
A. Axial computed tomography (CT) obtained for evaluation of fever shows mild splenomegaly (maximal diameter, 13 cm).
B. Axial fused positron emission tomography-CT image shows mildly increased 18F-fluorodeoxyglucose uptake in the spleen (maximum standardized uptake value, 3.0). The differential diagnoses included infection and hematologic malignancy.
C. Percutaneous ultrasound-guided core needle biopsy of the spleen was performed using an 18-G needle. The arrowheads indicate the tip of the biopsy needle. Histopathologic examination showed inflammatory infiltrates without evidence of malignancy.
D. Follow-up CT scan obtained 1 day after the procedure to evaluate a decrease in blood hemoglobin levels (8.0 g/dL to 6.3 g/dL) shows perisplenic hemorrhage (arrowheads) and probable active extravasation of contrast media (arrow). The patient showed no hemodynamic instability and improved with supportive management.
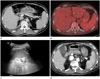
Fig. 2
A 66-year-old female patient with known lung cancer: case with a nondiagnostic histopathologic result.
A. Axial CT shows multiple low density lesions in the spleen, which were considered as possible splenic metastases.
B. US examination shows a 1.4-cm hypoechoic lesion in the spleen. The index mass and other lesions were poorly visualized owing to poor sonic window. Needle approach was hindered by narrow intercostal space of the patient. The histopathologic result was nondiagnostic, and splenectomy revealed sclerosing angiomatoid nodular transformation.
CT = computed tomography, US = ultrasound
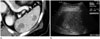
Fig. 3
A 43-year-old male patient with splenic hemangiomas: case with a favorable result.
A. Axial CT shows numerous hypointense lesions in the spleen.
B. US examination shows multiple hyperechoic lesions in the spleen, one of which was biopsied using an 18-G core needle. The histopathologic diagnosis was hemangioma.
CT = computed tomography, US = ultrasound

Table 1
Clinical and Radiological Characteristics of 30 Patients and Their Splenic Lesions

Table 2
Histopathologic Results of Ultrasound-Guided Core Needle Biopsy of Splenic Lesions in 30 Patients

Table 3
Radiologic Impression, Histopathologic Results, Modalities of Further Evaluation and Final Diagnosis in 6 Patients with Nondiagnostic Results on Ultrasound-Guided Percutaneous Core Needle Biopsy

References
1. Compérat E, Bardier-Dupas A, Camparo P, Capron F, Charlotte F. Splenic metastases: clinicopathologic presentation, differential diagnosis, and pathogenesis. Arch Pathol Lab Med. 2007; 131:965–969.
2. Cadili A, de Gara C. Complications of splenectomy. Am J Med. 2008; 121:371–375.
3. Lehne G, Hannisdal E, Langholm R, Nome O. A 10-year experience with splenectomy in patients with malignant non-Hodgkin's lymphoma at the Norwegian Radium Hospital. Cancer. 1994; 74:933–939.
4. Machado NO, Grant CS, Alkindi S, Daar S, Al-Kindy N, Al Lamki Z, et al. Splenectomy for haematological disorders: a single center study in 150 patients from Oman. Int J Surg. 2009; 7:476–481.
5. Keogan MT, Freed KS, Paulson EK, Nelson RC, Dodd LG. Imaging-guided percutaneous biopsy of focal splenic lesions: update on safety and effectiveness. AJR Am J Roentgenol. 1999; 172:933–937.
6. Quinn SF, vanSonnenberg E, Casola G, Wittich GR, Neff CC. Interventional radiology in the spleen. Radiology. 1986; 161:289–291.
7. Solbiati L, Bossi MC, Bellotti E, Ravetto C, Montali G. Focal lesions in the spleen: sonographic patterns and guided biopsy. AJR Am J Roentgenol. 1983; 140:59–65.
8. Gómez-Rubio M, López-Cano A, Rendón P, Muñoz-Benvenuty A, Macías M, Garre C, et al. Safety and diagnostic accuracy of percutaneous ultrasound-guided biopsy of the spleen: a multicenter study. J Clin Ultrasound. 2009; 37:445–450.
9. Lieberman S, Libson E, Maly B, Lebensart P, Ben-Yehuda D, Bloom AI. Imaging-guided percutaneous splenic biopsy using a 20- or 22-gauge cutting-edge core biopsy needle for the diagnosis of malignant lymphoma. AJR Am J Roentgenol. 2003; 181:1025–1027.
10. Muraca S, Chait PG, Connolly BL, Baskin KM, Temple MJ. US-guided core biopsy of the spleen in children. Radiology. 2001; 218:200–206.
11. Venkataramu NK, Gupta S, Sood BP, Gulati M, Rajawanshi A, Gupta SK, et al. Ultrasound guided fine needle aspiration biopsy of splenic lesions. Br J Radiol. 1999; 72:953–956.
12. Olson MC, Atwell TD, Harmsen WS, Konrad A, King RL, Lin Y, et al. Safety and accuracy of percutaneous image-guided core biopsy of the spleen. AJR Am J Roentgenol. 2016; 206:655–659.
13. McInnes MD, Kielar AZ, Macdonald DB. Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology. 2011; 260:699–708.
14. Liang P, Gao Y, Wang Y, Yu X, Yu D, Dong B. US-guided percutaneous needle biopsy of the spleen using 18-gauge versus 21-gauge needles. J Clin Ultrasound. 2007; 35:477–482.
15. Patel N, Dawe G, Tung K. Ultrasound-guided percutaneous splenic biopsy using an 18-G core biopsy needle: our experience with 52 cases. Br J Radiol. 2015; 88:20150400.
16. Civardi G, Vallisa D, Bertè R, Giorgio A, Filice C, Caremani M, et al. Ultrasound-guided fine needle biopsy of the spleen: high clinical efficacy and low risk in a multicenter Italian study. Am J Hematol. 2001; 67:93–99.
17. Kim SH, Min YI, Lee IC, Lee MG, Auh YH, Hyun CD. Fine-needle aspiration of splenic lesions. J Korean Radiol Soc. 1994; 31:921–924.
18. Lindgren PG, Hagberg H, Eriksson B, Glimelius B, Magnusson A, Sundström C. Excision biopsy of the spleen by ultrasonic guidance. Br J Radiol. 1985; 58:853–857.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download