Abstract
Hemangioma is rarely found in the mediastinum or lung. In the mediastinum, this tumor is usually located in the anterior mediastinum and manifests as a nonspecific soft tissue mass. In the lung, it usually presents as a well-defined nodule. To the best of our knowledge, there is no case of cavernous hemangioma concurrently involving the mediastinum and lung parenchyma, except for one case of concurrent cardiac and pulmonary hemangiomas. Here, we present an interesting case of cystic anterior and middle mediastinal masses together with multiple pulmonary nodules and ground glass opacities, which were diagnosed as cavernous hemangiomas. When similar findings are encountered, clinicians should consider hemangioma in the differential diagnosis.
Hemangioma occurs most commonly in the subcutaneous tissue, liver, bone, central nervous system, or spleen, but it rarely occurs in the mediastinum or lung (12). In the mediastinum, this tumor is usually located in the anterior mediastinum. When observed in the middle mediastinum, it is normally considered a continuation of disease from the anterior location (2). Intrapulmonary hemangioma is exceedingly rare, and it usually presents as a solitary mass or multiple masses. We present an interesting case of cavernous hemangioma concurrently involving both the anterior and middle mediastinum and the lung parenchyma. To the best of our knowledge, there is no reported case of this type.
A 61-year-old man visited our hospital for further evaluation of abnormal findings on chest radiography and computed tomography (CT) during health screening. The patient had a 100 pack-year history of smoking and had undergone a splenectomy because of sarcoidosis 2 years previously.
At the time of admission, chest radiography revealed a massive mediastinal mass and a prominent right hilum (Fig. 1). CT revealed thin-walled multiloculated cystic masses (approximately 1.5 cm to 8 cm) in the anterior mediastinum, and a mass with both cystic and soft tissue attenuation with punctate calcifications in the middle mediastinum. These masses compressed, but did not invade, the great vessels. None of the lesions in the anterior and middle mediastinum showed significant enhancement (less than 10 Hounsfield unit). The mass with soft tissue density in the middle mediastinum was contiguous with masses in the right hilum and was located along the bronchovascular bundle in the right upper lobe (RUL) (Figs. 2, 3). CT with a lung window setting revealed multiple ill-defined ground glass opacities (GGOs) and multiple nodules with GGO (Fig. 4) adjacent to the masses along the bronchovascular bundle. None of the involved bronchi were obstructed.
At this point in our investigation, we considered the possibility of malignant tumors such as lymphoma, thymic carcinoma, germ cell tumors, and small cell lung cancer because of concurrent involvement of the mediastinum and the lung parenchyma, in spite of the presence of multiple punctate calcifications in the masses. However, positron emission tomography-CT, which was performed to rule out the possibility of malignancy of the lesions, did not show significant fluorodeoxyglucose uptake.
Thoracotomy was performed for partial removal of the anterior and middle mediastinal masses and biopsy of the lesions in the right hilum and RUL. Biopsy of the RUL was performed for a consolidative lesion near the RUL bronchus. Macroscopic examination of the specimens obtained from the anterior mediastinum revealed multiloculated cysts filled with blood and serous material. The middle mediastinal masses resembled lymph nodes at the time of the operation, but they were confirmed as cysts filled with blood and serous material on histopathological examination. All specimens obtained from the anterior and middle mediastinum, right hilum, and RUL were pathologically confirmed as cavernous hemangiomas (Fig. 5).
On follow-up chest CT after 4 years, the number of mediastinal masses had decreased, probably due to the previous resection, and the stagnated multiple lung nodules and ground glass appearance remained unchanged (Fig. 6).
Mediastinal hemangioma is an uncommon benign vascular tumor accounting for less than 0.5% of all mediastinal masses (3). Mediastinal hemangioma usually manifests as a nonspecific soft tissue mass. Phleboliths, multiple enhanced vessels, and peripheral puddling of contrast enhancement may be potential diagnostic features (4). In the present case, all resected specimens were composed of cysts and no solid portion was found. Retrospectively, the lesion with soft tissue density in the middle mediastinum is thought to be the cystic portion filled with blood. Cystic changes have been reported in mediastinal hemangioma; to the best of our knowledge, they have been reported in only six cases (5678).
In the present case, biopsy specimens were also obtained from the masses in the RUL, and these specimens were pathologically confirmed as cavernous hemangiomas. Pulmonary hemangioma may arise anywhere in the lower respiratory tract, from the lung parenchyma to the airways and the bronchial tree (1). However, cavernous hemangioma occurring in the lung parenchyma is very rare. To the best of our knowledge, 30 cases have been reported in the literature to date and no characteristic radiological findings have been identified thus far. While most of the patients in these cases presented with a well-defined solitary nodule, only eight patients presented with multiple nodules. In some of the cases with a solitary nodule, the nodule showed ill-defined margins, and ten cases showed growth on follow-up images (9). The case presented herein exhibited ill-defined GGOs around the masses along the bronchovascular bundle and multiple nodules with GGO in the RUL. These lesions did not change during 4 years of follow up. Therefore, we supposed that the GGO and nodules were hemangiomas rather than inflammation. In this case, the pathologic picture did not fully explain why the hemangioma showed the GGO pattern as the GGO portion was not contained in the biopsy specimen. Therefore, GGO patterns could be not only hemangiomas but also other benign lesions such as fibrotic change. However, since hemangioma consists of large interconnecting vascular spaces and interspersed stromal elements such as fat, myxoid, or fibrous tissue (10), our possible theory is that the GGO pattern reflects these interspersed stromal elements in the lung parenchymal tissue. We expect that future research on hemangioma will investigate the direct correlation between CT findings and pathology.
In conclusion, hemangioma can concurrently involve both the mediastinum and the lung parenchyma. When similar findings are encountered, clinicians should consider hemangioma in the differential diagnosis.
Figures and Tables
Fig. 1
A chest radiograph (postero-anterior view) shows a massive mediastinal mass and a prominent right hilum.

Fig. 2
An unenhanced computed tomography scan shows homogeneously attenuated thin-walled multiloculated cystic masses in the anterior mediastinum. In the middle mediastinum, there is a mass with a cystic and soft tissue density with punctate calcifications (arrows), which are thought to be phleboliths.
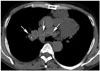
Fig. 3
A contrast-enhanced computed tomography scan obtained at the same level as that shown in Fig. 2. None of the lesions in the anterior and middle mediastinum show significant enhancement (less than 10 Hounsfield unit). The soft tissue density portion of the middle mediastinal mass is contiguous with masses in the right hilum and is located along the bronchovascular bundle in the right upper lobe (arrows).
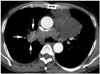
Fig. 4
A chest computed tomography scan with a lung window setting shows multiple ill-defined ground glass opacities and multiple nodules with ground glass opacity (arrowheads) in the right upper lobe adjacent to the masses along the bronchovascular bundle, which are contiguous with those in the right hilum and the middle mediastinum. Based on histopathological examination of biopsy specimens, the diagnosis is cavernous hemangioma.

Fig. 5
Photomicrograph of the mass in the RUL shows thin-walled cavities, formed by cystic dilatation of vascular lumens. The cavities share a single wall and red blood cells are present, consistent with cavernous hemangioma (hematoxylin-eosin stain; original magnification × 100). RUL = right upper lobe

References
1. Weissferdt A, Moran CA. Primary vascular tumors of the lungs: a review. Ann Diagn Pathol. 2010; 14:296–308.
2. Ceyhan M, Elmali M, Yildiz L. Mediastinal hemangioma and accompanying aortic arch anomaly. Pediatr Cardiol. 2008; 29:867–869.
3. Agarwal PP, Seely JM, Matzinger FR. Case 130: mediastinal hemangioma. Radiology. 2008; 246:634–637.
4. Cheung YC, Ng SH, Wan YL, Tan CF, Wong HF, Ng KK. Dynamic CT features of mediastinal hemangioma: more information for evaluation. Clin Imaging. 2000; 24:276–278.
5. Deepak J, Babu MN, Gowrishankar BC, Ramesh S. Mediastinal hemangioma: masquerading as pleural effusion. J Indian Assoc Pediatr Surg. 2013; 18:162–164.
6. Hammoumi MM, Sinaa M, Arsalane A, Oueriachi FE, Kabiri el H. Mediastinal cystic haemangiomas: a two cases report and review of the literature. Heart Lung Circ. 2014; 23:e118–e121.
7. Choi SJ, Kim GY, Park CH, Lee JI, An CH. Venous hemangioma presenting as a mediastinal cyst on CT. J Korean Radiol Soc. 2007; 56:483–486.
8. Kubokura H, Okamoto J, Hoshina H, Ishii H, Koizumi K, Shimizu K. Mediastinal cystic hemangioma presenting as bilateral bloody pleural effusion: a case report. J Nippon Med Sch. 2012; 79:381–384.
9. Miyamoto U, Tominaga M, Tomimitsu S, Nakanishi K, Hayashi A, Irie K. A case of multiple pulmonary cavernous hemangioma. Respirol Case Rep. 2015; 3:29–32.
10. Song HB, Park JC. Posterior mediastinal hemangioma mimicking Neurogenic tumor: a case report. J Korean Soc Radiol. 2015; 73:58–61.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download