Abstract
Giant plexiform neurofibromas, which are rare in patients with neurofibromatosis type II (NFII), are difficult to manage surgically, as they are extensively infiltrative and highly vascularized. Preoperative embolization is performed to reduce intraoperative blood loss and operative time, increase resectability of lesions, and improve visualization of the operative field during surgery of hypervascular tumors such as renal cell carcinoma and intracranial meningioma. Preoperative intravascular embolization of a giant chest wall neurofibroma has not been reported in the English literature. We report successful treatment of a giant chest wall neurofibroma in a 45-year-old male with NFII by preoperative intravascular embolization followed by surgical resection.
Neurofibromas are common benign soft-tissue tumors arising within peripheral nerves, which are very rare in patients with neurofibromatosis type II (NFII) (1). Neurofibromas are classically divided into localized, diffuse, and plexiform types (2). Plexiform neurofibromas can undergo continuous enlargement and eventually become giant lesions (2). If giant plexiform neurofibromas cause symptoms, they require appropriate treatment. The management of patients with plexiform neurofibromas is not well-defined and is mostly limited to symptom control and surgical resection (3).
Neurofibromas exhibit hypervascular characteristics (4); hence, uncontrolled perioperative bleeding during surgical resection can be a serious problem. Preoperative embolization offers a number of potential benefits such as reducing blood loss during surgery (5). Therefore, preoperative embolization is expected to reduce complications such as massive bleeding during surgical resection of the neurofibroma.
We report here the successful treatment of a giant plexiform neurofibroma of the chest wall in a 45-year-old man with NFII by preoperative intravascular embolization followed by surgical resection.
Our Institutional Review Board (IRB) does not require approval for case reports involving fewer than three patients. However, this patient was included in an IRB approval research database.
A 45-year-old man complained of a right chest wall mass that rapidly increased in size over a period of one month. He was diagnosed with NFII 15 years ago at an outside hospital. Initial physical examination revealed a large, tender, soft tissue mass that originated in the upper thoracic region and overhung the right posterolateral chest wall (Fig. 1A). Chest computed tomography (CT) revealed a 16.8 × 15.8 × 7.3 cm sized, large soft tissue mass arising from the subcutaneous tissues of the right lateral chest wall with a chest wall and right rib deformity (Fig. 1B, C). Contrast-enhanced CT was not performed due to high levels of blood urea nitrogen (42 mg/dL) and creatinine (3.3 mg/dL).
He was referred for preoperative embolization before the scheduled surgery. In order to reduce bleeding during surgical resection, preoperative intra-arterial embolization was performed.
A retrograde right common femoral artery puncture was performed under local anesthesia. Thoracic aortography showed hypertrophy of the right lateral thoracic artery and large tumor staining in the area of the right chest wall (Fig. 2A), and selective angiography of the right lateral thoracic artery using a 2.2-Fr microcatheter (Progreat; Terumo, Tokyo, Japan) revealed tumor staining via the right lateral thoracic artery (Fig. 2B). Then, the right lateral thoracic artery was embolized with polyvinyl alcohol particles (250/355 and 355/500 microns, Contour; Boston Scientific, Natick, MA, USA). The post-embolization angiogram of the right subclavian artery showed complete obliteration of tumor feeders without the presence of another tumor feeding artery and disappearance of the tumor blush (Fig. 2C).
For seven days after preoperative embolization, tumor regression was satisfactory, with small areas of skin necrosis and no associated systemic complications. At nine days after preoperative intravascular embolization, the patient underwent surgical resection without intraoperative blood transfusion and complication.
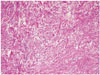
Grossly, the specimen was a cystic mass containing blood clots and was surrounded by myxoid-like black pigmented tissue; it measured 23 × 20 × 4 cm. Histologic examination revealed a plexiform neurofibroma with no evidence of malignancy (Fig. 3). The patient was discharged without complications. A follow-up CT scan after one year did not reveal any local recurrence (Fig. 2D).
Neurofibromatosis (NF) is an autosomal dominant disorder mainly characterized by abnormalities in the nervous system and skin (6). Neurofibromatosis type I (NFI) and NFII are the best described variants. NFII is known as central NF and is generally characterized by bilateral vestibular schwannomas, unlike NFI, which is known as peripheral NF (6).
NFII is a dominantly inherited genetic disorder resulting from mutations involving the NFII gene on chromosome 22 (7). It is a rare condition and its prevalence is estimated to be about 1 in 50000 (7). Neurofibromas develop frequently in individuals with NF, and they are very rare in patients with NFII. Neurofibromas are poorly circumscribed, unencapsulated tumors, which diffusely infiltrate the nerve and the adjacent fat and muscle (8). Plexiform neurofibromas characteristically show diffuse irregular infiltration into the adjacent muscle and fat (8). This tumor has a locally aggressive behavior, but its infiltrative pattern is not indicative of malignancy (8). When a plexiform neurofibroma grows rapidly or clinical neurologic symptoms are present, an appropriate treatment such as surgical resection is required.
Neurofibroma is a typical hypervascular tumor, and a few reports suggest that the bleeding tendency observed in neurofibromas occasionally causes a large amount of bleeding during surgery (4). Hence, a giant neurofibroma makes the operative field narrow and limited. Preoperative embolization is an established technique to reduce intraoperative blood loss in hypervascular tumors such as renal cell carcinoma, intracranial meningioma, and spinal tumor (9). Furthermore, it is also effective in reducing operative time, increasing resectability of tumors, and improving visualization of the operative field (10). Taking this into account, we decided to perform preoperative intravascular embolization for the treatment of a giant chest wall neurofibroma.
Preoperative embolization is generally a safe procedure and reports low complication rates (10). However, serious complications can occur, including stroke, ischemic attack, and necrosis (10). Therefore, identification of dangerous anastomoses and careful manipulation of the catheter and injection of the embolic material are crucial to avoid serious complications.
To the best of our knowledge, this is the first report of preoperative embolization and surgical resection of a giant neurofibroma of the chest wall in a patient with NFII. Technical and clinical success was achieved, without evidence of complications such as massive perioperative blood loss.
In this case, we achieved success in the treatment with preoperative intra-arterial embolization and surgical resection in a NFII patient who developed a giant plexiform neurofibroma involving his right chest wall.
In conclusion, our report demonstrates that preoperative intravascular embolization of a giant plexiform neurofibroma of the chest wall is not only technically feasible, but it can also reduce blood loss and morbidity at the time of surgery. Therefore, we recommend that embolization should be performed prior to surgical resection for a giant plexiform neurofibroma.
Figures and Tables
Fig. 1
A 45-year-old man with NFII shows a right chest wall mass.
A. Preoperative clinical image shows a large mass in the right posterior chest region.
B, C. Preoperative noncontrast axial (B) and coronal (C) computed tomography scans show a large soft tissue mass (16.8 × 15.8 × 7.3 cm) (white arrowheads) in the right lateral chest.
NFII = neurofibromatosis type II

Fig. 2
A giant plexiform neurofibroma of the right chest wall was treated by preoperative intravascular embolization followed by surgical resection.
A. Thoracic aortography shows hypertrophy of the right lateral thoracic artery (white arrow) and tumor blush in the right lateral chest.
B. Selective right lateral thoracic arteriography (white arrow) shows increased vascularity and intense tumor blush (white arrowhead).
C. Complete angiography of the right subclavian artery after embolization shows complete obliteration of the right lateral thoracic artery without the presence of another tumor feeding artery.
D. The 4 month follow-up postoperative non-contrast axial computed tomography scan does not show recurrence or neurofibroma.

References
1. Jones RG, Kiatisevi P, Morris DC, Munk PL, Clarkson PW, Masri BA. Intravascular embolisation and surgical resection of a giant neurofibroma with intratumoural haemorrhage. Br J Radiol. 2010; 83:e225–e229.
2. Vélez R, Barrera-Ochoa S, Barastegui D, Pérez-Lafuente M, Romagosa C, Pérez M. Multidisciplinary management of a giant plexiform neurofibroma by double sequential preoperative embolization and surgical resection. Case Rep Neurol Med. 2013; 2013:987623.
3. Ji Y, Xu B, Wang X, Liu W, Chen S. Surgical treatment of giant plexiform neurofibroma associated with pectus excavatum. J Cardiothorac Surg. 2011; 6:119.
4. Kashyap RR, Gogineni SB. Hypervascular neurofibromas in a case of neurofibromatosis type 1 - a case report. J Clin Exp Dent. 2011; 3:Suppl 1. e356–e359.
5. Shah AH, Patel N, Raper DM, Bregy A, Ashour R, Elhammady MS, et al. The role of preoperative embolization for intracranial meningiomas. J Neurosurg. 2013; 119:364–372.
6. Cihangiroglu M, Yilmaz S, Topsakal C, Gok U, Altinsoy B, Cobanoglu B. Laryngeal neurofibroma associated with neurofibromatosis type 2. AJNR Am J Neuroradiol. 2002; 23:1637–1639.
7. Pendse NA, Menghani V. Neurofibromatosis 2 - a case report. Indian J Radiol Imaging. 2003; 13:99–101.
8. Hourani R, Rizk T, Kung S, Boudghène F. Elephantiasis neuromatosa in neurofibromatis type I. MRI findings with review of the literature. J Neuroradiol. 2006; 33:62–66.
9. Shakir M, Blossom G, Lippert J. Anterior mediastinal paraganglioma: a case for preoperative embolization. World J Surg Oncol. 2012; 10:134.
10. Nair S, Gobin YP, Leng LZ, Marcus JD, Bilsky M, Laufer I, et al. Preoperative embolization of hypervascular thoracic, lumbar, and sacral spinal column tumors: technique and outcomes from a single center. Interv Neuroradiol. 2013; 19:377–385.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download