Abstract
Adrenal hemorrhage following blunt trauma is a rare occurrence. We report here the case of a 5-year-old child with adrenal hemorrhage, which developed as a result of an accidental fall. Embolization treatment of adrenal hemorrhage was successfully performed. To the best of our knowledge, this is the first report of adrenal hemorrhage occurring in a child which was treated with transcatheter embolization.
Traumatic adrenal hemorrhage is rare because of the small size and retroperitoneal location of the adrenal glands, and because the adrenal gland is surrounded by the paraspinal muscles, the rib cage, and liver (1). Recently, because of the widespread and frequent use of computed tomography (CT), a high incidence of adrenal injury, up to 25%, has been detected in cases of severe abdominal trauma (2). In pediatric patients, isolated post-traumatic adrenal injuries are infrequent and they are usually accompanied by multi-organ injuries, which have been perceived as incidental findings (3).
The management of adrenal injuries generally depends on the concomitant injuries, while isolated adrenal injury is usually managed conservatively or may require transcatheter embolization (4). Particularly in pediatric patients, conservative management is generally performed, even in cases of adrenal bleeding requiring transfusion (5).
We report a case of pediatric adrenal hemorrhage treated with transcatheter embolization.
A 5-year-old boy fell from a height of about 5 m. Upon admission to the emergency room of our hospital, he did not complain of any symptoms, except for headache and some bruises on his face and back. Plain radiography of the skull and CT of the brain revealed right occipital and parietal bone fractures without intracranial hemorrhage. Chest CT showed multifocal lung contusions. Abdominal CT demonstrated a small right suprarenal and retroperitoneal hematoma with contrast extravasation into the right adrenal gland as well as multifocal lacerations in the right lobe of the liver and segmental renal infarction in the anterosuperior aspect of the right kidney (Fig. 1). Laboratory tests revealed a slightly decreased hemoglobin level of 11.2 g/dL (mean, 12.5 g/dL) and slightly elevated liver enzymes. He was alert and his vital signs were stable, except for a markedly increased pulse rate of 124/min. The following several reasons led us to perform transcatheter embolization therapy: 1) a definite active bleeding focus in the right adrenal gland; 2) possibility of additional active bleeding; 3) the patient was assigned the major trauma category according to the injury severity score (ISS) of more than 15 (medical score to assess trauma severity) (6); 4) unpredictable status, including vital signs of the pediatric patient.
Access was achieved via the right common femoral artery puncture with a 4-Fr vascular sheath (Terumo, Tokyo, Japan) and a 21-G puncture needle under ultrasonographic guidance. Non-selective aortography was performed with a 4-Fr pig-tail catheter (Cook Inc., Bloomington, IN, USA), which revealed no demonstrable abnormality. A 4-Fr Cobra catheter (Terumo, Tokyo, Japan) was used for selective right renal arteriography to demonstrate the arterial supply of the adrenal gland. There was no arterial supply to the adrenal gland from the right renal artery. Additional selective right inferior phrenic artery (RIPA) arteriography was performed in the same way, and it revealed that the superior, middle, and inferior adrenal arteries originated from the RIPA with extravasation of contrast medium (Fig. 2). We primarily embolized the superior and middle adrenal arteries with a mixture of N-butyl cyanoacrylate (Histoacryl; B.Braun, Tuttlingen, Germany) and lipiodol (Guerbet, Paris, France) at a dilution of 1:4. On follow-up RIPA arteriography, contrast extravasation into the adrenal gland was still detected via the middle and inferior adrenal arteries. Additional embolization was performed via the proximal branch of the superior and middle adrenal arteries. There was no evidence of definite extravasation of contrast medium, but subtle parenchymal staining in the right adrenal gland was detected on additional follow-up RIPA arteriography. To prevent delayed hemorrhage and to obtain a temporary embolic effect, we performed embolization via the common trunk of the RIPA with a gelatin sponge (Alicon, Zhejiang, China). During the procedure, a pseudoaneurysm in the adrenal parenchyma was newly detected via the inferior adrenal artery. We performed additional embolization of the inferior adrenal artery with a mixture of N-butyl cyanoacrylate and lipiodol at a dilution of 1:4. Embolization treatment of adrenal hemorrhage was successfully performed and active bleeding was no longer detected (Fig. 3). After 1 week, follow-up abdominal CT demonstrated no active bleeding in the right adrenal gland. Furthermore, the patient remained clinically well on the out-patient follow-up examination one month later.
Traumatic adrenal injury rarely occurs in the pediatric or the general population (5). Several studies have reported that the incidence of traumatic adrenal injury in the pediatric population was 0.03–4.95% (7), 3–5% (5), and 7.5% (8), which increased with the use of multi-detector CT (2).
The following three possible mechanisms for the occurrence of adrenal hemorrhage have been proposed: 1) Compression of the adrenal gland against the spinal column; 2) An acute increase in the intra-adrenal venous pressure due to compression of the inferior vena cava. This may explain why the right adrenal gland is more commonly affected; and 3) Shearing of small vessels that perforate the adrenal capsule, resulting from secondary deceleration forces (9).
The management of adrenal hemorrhage may be either surgical or conservative according to the extent of the injury and the patient's hemodynamic stability (10). The modern management of blunt adrenal trauma is usually non-operative (2). Embolization treatment is occasionally reported in patients with an isolated adrenal gland injury (5). Several previous studies have reported that several pediatric patients with traumatic adrenal hemorrhage were successfully cured with conservative treatment (37). In our case, we decided to perform transcatheter embolization therapy with consideration for a definite active bleeding focus, possibility of additional active bleeding, trauma severity, and unpredictable status including vital signs of pediatric patient. In our literature search, we could not identify any pediatric patient who was treated with transcatheter embolization for post-traumatic adrenal hemorrhage.
Embolization can be performed with various agents, including coil, glue, and gelatin sponge. Embolic agents must be applied on a case by case basis, considering the clinical purpose, preference of the radiologists, and accessibility of the agent (9). In our case, we preferred N-butyl cyanoacrylate glue for primary superior and middle adrenal arterial embolization because the vessels are of small-caliber and relatively tortuous. After we embolized the proximal branch of the superior and middle adrenal arteries, we used a gelatin sponge, a temporary agent for additional preventive embolization. It is inevitable that we would have to embolize via the common trunk of the RIPA because a pseudoaneurysm was unfortunately discovered in the adrenal parenchyma. However, the contralateral adrenal gland was so intact that the procedure was performed without any special complications. The patient was healthy after 1 month despite right adrenal infarction.
In conclusion, transcatheter embolization may be a treatment option for post-traumatic adrenal hemorrhage in pediatric patients.
Figures and Tables
Fig. 1
Contrast-enhanced computed tomography demonstrating a retroperitoneal hematoma with contrast extravasation into the right adrenal gland (solid arrows), segmental renal infarction in the right kidney (arrowhead), and multifocal liver lacerations (open arrows).
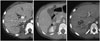
Fig. 2
RIPA arteriography demonstrating the superior (solid arrow), middle (arrowhead), and inferior (open arrow) adrenal arteries originating from the RIPA and extravasation of contrast medium.
RIPA = right inferior phrenic artery

Fig. 3
Follow-up RIPA arteriography (A) revealing adrenal parenchymal staining via the inferior adrenal artery (arrows), but extravasation of contrast medium was unclear. During preventive embolization via the common trunk of the RIPA (B), a pseudoaneurysm (arrowheads) was detected. Additional embolization was performed. Final angiography (C) revealing complete embolization of the pseudoaneurysm in the adrenal parenchyma. There is no further evidence of active bleeding.
RIPA = right inferior phrenic artery

References
1. Dinc H, Sims¸ek A, Ozyavuz R, Ozgür GK, Gümele HR. Endovascular treatment of massive retroperitoneal haemorrhage due to inferior adrenal artery injury. A case report. Acta Radiol. 2002; 43:326–328.
2. Agrawal N, Rao S, Zellweger R, Knight T. Adrenal pseudoaneurysm due to blunt trauma. Indian J Surg. 2013; 75:Suppl 1. 155–157.
3. Gabal-Shehab L, Alagiri M. Traumatic adrenal injuries. J Urol. 2005; 173:1330–1331.
4. To'o KJ, Duddalwar VA. Imaging of traumatic adrenal injury. Emerg Radiol. 2012; 19:499–503.
5. Roupakias S, Papoutsakis M, Mitsakou P. Blunt adrenal gland trauma in the pediatric population. Asian J Surg. 2011; 34:103–110.
6. Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988; 28:69–77.
7. Sivit CJ, Ingram JD, Taylor GA, Bulas DI, Kushner DC, Eichelberger MR. Posttraumatic adrenal hemorrhage in children: CT findings in 34 patients. AJR Am J Roentgenol. 1992; 158:1299–1302.
8. Choi SJ, Kim JE, Ryu Il, Kim JJ, Choi HY. MDCT findings of traumatic adrenal injury in children. J Korean Soc Radiol. 2011; 64:191–195.
9. Fowler AM, Burda JF, Kim SK. Adrenal artery embolization: anatomy, indications, and technical considerations. AJR Am J Roentgenol. 2013; 201:190–201.
10. Rammelt S, Mucha D, Amlang M, Zwipp H. Bilateral adrenal hemorrhage in blunt abdominal trauma. J Trauma. 2000; 48:332–335.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download