Abstract
Purpose
The purpose of this study was to identify the characteristics of chest lesions that are missed in interpretations of neck computed tomography (CT) scans.
Materials and Methods
A total of 240 consecutive neck CT scans were retrospectively analyzed to determine whether chest lesions were included or not. All missed chest lesions, which had not been described on neck CT reports, were recorded, and classified according to their clinical significance (insignificant, indeterminate, or significant) and awareness (known or unknown) at the time of CT interpretation, and their radiologic patterns were analyzed.
Results
Eighty seven (36.3%) of 240 neck CT scans had 105 chest lesions, and 88 of these were not described on the neck CT reports. Thirty seven clinically known or insignificant lesions were excluded, resulting in a miss rate for chest lesions of 35.2% (37/105), with six of these (5.7%) being potentially significant. The most common location of missed chest lesions was the lung (56/88, 63.6%), and 45 (80.4%) of these missed lung lesions were visualized only with lung window settings.
With the increasing complexity of radiologic imaging in association with continuous advancement of the technical science, the demands for sub-specialized knowledge within radiology have increased greatly (1). However, in practice, we can’t afford to have all radiologic examinations interpreted by specialized radiologists. Occasionally, as in cases of neck or abdominal computed tomography (CT) scans, additional specific sites (i.e., a part of the chest) may inevitably be included and also need to be interpreted correctly. Incidental but potentially important findings outside the area of interest may be present but missed in any radiologic studies (23456). We have occasionally found chest lesions that were not reported on neck CT interpretations when follow-up neck or chest CT studies were performed and compared with a previous neck CT study. The authors are unaware of any published study that addresses this issue of chest lesions being missed in interpretations of neck CT scans. Therefore we have attempted to assess the characteristics, such as prevalence, clinical significance, and radiologic patterns, of chest lesions that are missed on neck CT interpretations. This may provide useful information for radiologists interpreting neck CT scans that include areas in the chest.
This retrospective study was approved by the Institutional Review Board, and the requirement for informed consent was waived. Three hundred ninety three (393) consecutive contrast enhanced neck CT scans of 393 patients that were performed from 1 to 31 May, 2014 at our institution were retrospectively reviewed. Of these, 153 neck CT scans of 112 patients who underwent chest CT scans on the same day and 41 patients who had follow-up neck CT scans during the selected study period were excluded. The remaining 240 neck CT scans were included in our study.
The CT scans were performed on 64 or 128 multidetector scanners (Light Speed VCT; GE Healthcare, Milwaukee, WI, USA, and Somatom Definition, Somatom Definition AS+, or Sensation 64; Siemens, Erlangen, Germany). The scanning volume covered the area from the skull base to the aortopulmonary window of the mediastinum in the cephalo-caudal direction, with 3-mm collimation, 3-mm reconstruction interval, 120 kVp, and 60 mAs. Enhanced images were acquired with a bolus contrast injection by using a mechanical injector at a rate of 2.5 mL/s, for a total dose of 100 mL.
The patients’ clinical information for disease status and management was obtained by reviewing medical charts. To detect chest lesions, neck CT scans were reviewed using both soft tissue and lung window settings. A consensus interpretation was made by two radiologists: one board-certified radiologist with 20 years of experience in reading chest CT scans and one radiology resident with 2 years’ experience in chest CT interpretations. Past records of neck CT reports were checked to determine whether those chest lesions were described or not. The original reports of neck CT scans were made by four board-certified radiologists with 5–20 years of experience in reading neck CT scans, or by radiology residents with 1–4 years of experience in reading neck CT scans with secondary confirmation by board-certified radiologists.
Missed (not described) and detected (described) chest lesions were recorded and classified according to their clinical significance (insignificant, indeterminate, or significant) and clinical awareness (known or unknown) at the time of the original neck CT interpretation. In addition, radiologic patterns, such as anatomic location, radiologic characteristics, and suggested disease were analyzed.
Clinical significance of the chest lesions was judged by the interpreting radiologists. Chest lesions requiring no further evaluation, treatment, or follow up were categorized as insignificant lesions. These included old tuberculosis (TB) scars, small subsegmental linear atelectasis, and small lung nodules with a high likelihood of benignity. Lesions requiring later radiological or clinical follow-up were categorized as indeterminate lesions. These included mild to moderate emphysema, mild bronchiectasis, indeterminate lung nodules, small pleural effusion, and nonspecific enlargement of mediastinal lymph nodes. Lesions requiring immediate further evaluation, treatment, or close follow-up were categorized as pneumonia, suspicious active TB, severe emphysema, pulmonary thromboembolism, or suspicious metastatic nodule. The anatomic locations of the chest lesions were classified as lung, pleura, mediastinum including cardiovascular system, or chest wall.
Clinical awareness of chest lesions at the time of the original neck CT interpretations was defined by whether those lesions were mentioned either in the previous imaging reports or in the medical chart.
The frequencies, anatomic locations, CT findings of the missed chest lesions were analyzed. The frequency of missed lung lesions that were visualized only with a lung window setting was also analyzed.
All data were entered into an Excel spreadsheet (Microsoft Office Excel 2007, Redmond, WA, USA), and descriptive statistical analyses were performed. A chi-square (χ2) test was used to compare incidences in anatomic distributions of missed chest lesions between patients with and without head and neck cancers. A p value of 0.05 or less was considered to indicate a statistically significant difference.
There were 111 men and 129 women, and patients’ ages ranged between 19 and 89 with a mean age of 57. Underlying conditions which led to neck CT scans of these patients were malignancies (n = 97) including head and neck cancers (n = 66), acute and chronic infection or inflammation of neck (n = 57), cervical lymphadenopathy (n = 32), and other various symptoms and signs (n = 54).
Of the total 240 neck CT scans, 87 scans showed 105 chest lesions (87/240, 36.3%) (Table 1). Among those 105 chest lesions, 88 (88/105, 83.8%) had not been described on the CT reports, and 50 (50/88, 56.8%) of these missed chest lesions were clinically unknown at the time of CT interpretation (Table 1). When clinically known lesions (n = 38) and unknown insignificant lesions (n = 13) were excluded from the 88 missed (not described) lesions, the miss rate of chest lesions was 35.2% (37/105). Seven (6.7%) of 105 chest lesions were clinically significant and previously unknown, and six (5.7%) were missed. These six included suspicious active TB (n = 2) (Fig. 1), bullous emphysema (n = 1) (Fig. 2), suspicious adenocarcinoma of the lung (n = 1) (Fig. 3), pulmonary thromboembolism (n = 1), and diffuse bony sclerosis associated with leukemia (n = 1).
Clinical, anatomic, and radiologic characteristics of all the chest lesions missed on neck CT scans are listed in Table 2. The most common location of the missed chest lesions was the lung (56/88, 63.6%), followed by the mediastinum including cardiovascular system, pleura, and chest wall (24/88, 27.3%; 5/88, 5.7%; 3/88, 3.4%, respectively). Three most commonly missed lung lesions were nodules (n = 13, 23.2%), emphysema (n = 14, 25.0%), and postinflammatory scarring (n = 16, 28.6%). Most (45/56, 80.4%) of the missed lung lesions were visualized only with lung window settings (Table 3, Fig. 3). The sclerotic bone lesion was seen only with a bone window setting.
There were 23 missed chest lesions in neck CT scans of 66 patients with head and neck cancers. These were comprised of fourteen pulmonary lesions, six mediastinal lesions, two pleural lesions, and one chest wall lesion. When these 23 missed chest lesions are compared to 65 missed chest lesions in 174 patients without head and neck cancers, the incidence of missed chest lesions is similar for the two groups (34.8% vs. 37.4%, respectively). Among the 23 missed chest lesions in patients with head and neck cancers, four were lung nodules: two were known metastatic nodules; one was an unknown indeterminate nodule; and one was a known benign nodule. The percentage of lung nodules in all missed chest lesions in patients with head and neck cancers was similar to that in patients without head and neck cancers [17.4% (4/23) vs. 13.8% (9/65), respectively]. In addition, the anatomic distributions of the missed chest lesions were not statistically different between the two groups with and without head and neck cancers (Table 4).
Errors during radiologic imaging studies are not uncommon and have long been recognized. These errors may lead to suboptimal management and consequently seriously impact a patient’s outcome (78). Since most errors occur during image interpretation, and perceptual misses (i.e., false-negative errors) are the most common misinterpretation made by radiologists (2910), we specifically focused on these false-negative missed chest lesions on neck CT scans.
Several articles have emphasized the importance of analyzing recurrent and common patterns of errors, to reduce or prevent repetition of the same error (7811). Other studies have reported that if the first radiologist misses a finding, the next radiologist will likely miss it as well (812). There are only a few studies which investigated common errors in the interpretation of head and neck CT scans, none of which focused on missed chest lesions (21314). One study showed that vascular lesions, such as aneurysm, were most commonly missed on head and neck CT angiography, and neck mass, sellar mass, and nasogastric tube malposition were also missed as well (13). In reading cranial CT and magnetic resonance imaging, the most common perceptual errors were extraaxial mass such as meningioma, thrombosis at dural venous sinus, and infarcts at posterior circulation (2). Lesions outside the area of primary examination can be more easily missed (234569), and careful attention should be paid to these "neglected" areas such as the chest in neck CT examinations. In our study, all original neck CT reports were directly or secondarily confirmed (after preliminary reading by residents) by board-certified radiologists. The missed chest lesions on these neck CT interpretations seem to be caused, not by lack of professionalism or experience, but by radiologists’ failure to pay attention.
In the present study, the most common site of the missed chest lesions was the lung. Significantly, 80% of these missed lung lesions were visualized only when lung window settings were used. Therefore it is reasonable to assume that separate reviews of the lungs with lung window settings might eliminate a similar proportion of missed lesions. Not many studies have addressed the importance of systemic review of all organs with appropriate window settings (149).
One recent study demonstrated that lung nodules were reported in 3% of abdominal CT studies, and 19% of lung nodules in patients with underlying malignancy were metastatic (15). Lung metastasis is also common in about 12% of patients with head and neck cancer (16), underscoring the importance of detecting lung nodules not only in abdominal CT scans but also in neck CT scans. In our study, four of the missed chest lesions in patients with head and neck cancer were pulmonary nodules, two of which were metastatic and fortunately clinically known. However, one clinically unknown, indeterminate nodule was also missed, which still has the potential for being metastatic. Since our study showed that the incidence of the missed chest lesions, including lung nodules in patients with head and neck cancer, is similar to that in patients without head and neck cancer. Thus it appears that the radiologist’s awareness of patients’ underlying diseases, such as head and neck cancer, does not influence the miss rate of chest lesions in neck CT interpretations. Another important point is that a small lung nodule can be "burned out" with a mediastinal window setting, so that a lung window setting should be used to avoid missing any pulmonary nodules (417). This problem may also apply to emphysema in that all 14 cases of emphysema were visualized only with a lung window setting in our study.
In the present study, the miss rate of the previously unknown significant chest lesions that would have influenced follow-up or management was 5.7% (6/105). This is comparable to reported interpretation error rates of 2–20% in previous imaging studies (181920). In a recent, large multifacility study of misinterpretation rates, an approximate 3.7% disagreement rate was detected, including 2.9% difficult cases and 0.8% non-difficult cases (21). That study also found that there were considerable differences in disagreement rates by modalities with CT showing a higher error rate of 7.2%. Similar error rates were observed in neuroradiologic imaging studies: 5.2% significant errors in reading head and neck CT angiography (13), 6% clinically consequential misinterpretation rate in non-contrast cranial CT (22), and 12–15% discordance rate between residents and neuroradiologists in interpretation of transverse and three-dimensional images (23).
The potentially significant and previously unknown missed chest lesions in our study were pulmonary thromboembolism, bullous emphysema, suspicious active TB, suspicious adenocarcinoma of the lung, and diffuse bony sclerosis associated with leukemia. Other studies have reported similar results, with frequently missed lesions on radiologic examinations being pulmonary embolism, venous thrombosis, unexpected gastrointestinal tumors, and bone and soft tissue lesions such as metastasis (239).
The present study has several limitations. First, it was a retrospective study, and our "gold standard" for missed chest lesions was expert consensus for the intrinsic false-negative results. This might have resulted in underestimation of the actual miss rate. Second, the clinical significance of the missed lesions was determined subjectively by the radiologists, not clinicians. However, it was carefully classified on the basis of all available radiologic and clinical data, combined with experiential knowledge while maintaining objectivity. Third, we did not assess adverse clinical outcomes that might have resulted from missed chest lesions. Lastly, since the imaging reconstruction algorithm for neck CT is slightly different from that of chest CT, and neck CT scans only include the upper third or quarter of the entire lung parenchyma, neck CT scans may provide incomplete interpretation of lung lesions. However, incidental detection of chest lesions on neck CT scans can provide the opportunity for further evaluation, which may include chest CT scans.
In conclusion, chest lesions were commonly identified and missed on the readings of neck CT scans, and a small percentage of them were potentially significant. Lung lesions accounted for the most common missed chest findings, and they were generally visualized only with lung window setting. The present study suggests performing a careful and systematic review of both neck and chest areas in reading neck CT scans, with additional use of lung window settings for optimal visualization of lung lesions.
Figures and Tables
Fig. 1
Neck CT image at the level of lung apex in a 42-year-old man presenting with tongue discomfort. Multiple clustered, centrilobular nodules are noted in the left upper lobe, raising the possibility of pulmonary tuberculosis, which were missed on neck CT interpretation.

Fig. 2
Neck CT at the level of lung apex in a 53-year-old man with peritonsilar abscess. CT image with lung window setting shows multiple variable sized bullae in the right lung apex, which was not described in neck CT report. Minimal centrilobular emphysema is also noted in the left upper lobe.

Fig. 3
Missed and significant chest lesion on neck CT in an 80-year-old man with thyroid cancer. The lower part of neck CT image with lung window setting (A) shows an irregular shaped peribronchial ground-glass opacity nodule (arrows) in the right upper lobe, suggesting adenocarcinoma of the lung. On mediastinal window setting (B), this lesion is not seen.

Table 1
Clinical Conditions of the 105 Chest Lesions Visualized on 240 Neck CT Scans
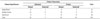
| Clinical Significance | Clinical Awareness | Total | |||
|---|---|---|---|---|---|
| Unknown | Known | ||||
| Missed | Detected | Missed | Detected | ||
| Insignificant | 13 | 1 | 8 | 1 | 23 |
| Indeterminate | 31 | 5 | 18 | 3 | 57 |
| Significant | 6 | 1 | 12 | 6 | 25 |
| Total | 50 | 7 | 38 | 10 | 105 |
Table 2
Clinical, Anatomic, and Radiologic Characteristics of the Chest Lesions Missed on Neck CT Interpretation

Table 3
Lung Lesions Visualized Only with Lung Window Settings

Table 4
Anatomic Distributions of the Missed Chest Lesions in Patients with and without Head and Neck Cancers

References
1. Briggs GM, Flynn PA, Worthington M, Rennie I, McKinstry CS. The role of specialist neuroradiology second opinion reporting: is there added value? Clin Radiol. 2008; 63:791–795.
2. Donald JJ, Barnard SA. Common patterns in 558 diagnostic radiology errors. J Med Imaging Radiat Oncol. 2012; 56:173–178.
3. Sosna J, Esses SJ, Yeframov N, Bernstine H, Sella T, Fraifeld S, et al. Blind spots at oncological CT: lessons learned from PET/CT. Cancer Imaging. 2012; 12:259–268.
4. Katz DS, Jorgensen MJ, Rubin GD. Detection and follow-up of important extra-arterial lesions with helical CT angiography. Clin Radiol. 1999; 54:294–300.
5. Koonce J, Schoepf JU, Nguyen SA, Northam MC, Ravenel JG. Extra-cardiac findings at cardiac CT: experience with 1,764 patients. Eur Radiol. 2009; 19:570–576.
6. Yee J, Kumar NN, Godara S, Casamina JA, Hom R, Galdino G, et al. Extracolonic abnormalities discovered incidentally at CT colonography in a male population. Radiology. 2005; 236:519–526.
7. Fitzgerald R. Error in radiology. Clin Radiol. 2001; 56:938–946.
8. Pinto A, Brunese L, Pinto F, Reali R, Daniele S, Romano L. The concept of error and malpractice in radiology. Semin Ultrasound CT MR. 2012; 33:275–279.
9. McCreadie G, Oliver TB. Eight CT lessons that we learned the hard way: an analysis of current patterns of radiological error and discrepancy with particular emphasis on CT. Clin Radiol. 2009; 64:491–499. discussion 500-501.
10. Renfrew DL, Franken EA Jr, Berbaum KS, Weigelt FH, Abu-Yousef MM. Error in radiology: classification and lessons in 182 cases presented at a problem case conference. Radiology. 1992; 183:145–150.
11. Robinson PJ. Radiology’s Achilles’ heel: error and variation in the interpretation of the Röntgen image. Br J Radiol. 1997; 70:1085–1098.
12. Kim YW, Mansfield LT. Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. AJR Am J Roentgenol. 2014; 202:465–470.
13. Lian K, Bharatha A, Aviv RI, Symons SP. Interpretation errors in CT angiography of the head and neck and the benefit of double reading. AJNR Am J Neuroradiol. 2011; 32:2132–2135.
14. Strub WM, Leach JL, Tomsick T, Vagal A. Overnight preliminary head CT interpretations provided by residents: locations of misidentified intracranial hemorrhage. AJNR Am J Neuroradiol. 2007; 28:1679–1682.
15. Alpert JB, Fantauzzi JP, Melamud K, Greenwood H, Naidich DP, Ko JP. Clinical significance of lung nodules reported on abdominal CT. AJR Am J Roentgenol. 2012; 198:793–799.
16. de Bree R, Deurloo EE, Snow GB, Leemans CR. Screening for distant metastases in patients with head and neck cancer. Laryngoscope. 2000; 110(3 Pt 1):397–401.
17. Albertyn LE. Extending the search pattern in computed tomography. Clin Radiol. 1987; 38:145–149.
18. Siegle RL, Baram EM, Reuter SR, Clarke EA, Lancaster JL, McMahan CA. Rates of disagreement in imaging interpretation in a group of community hospitals. Acad Radiol. 1998; 5:148–154.
19. Goddard P, Leslie A, Jones A, Wakeley C, Kabala J. Error in radiology. Br J Radiol. 2001; 74:949–951.
20. Berlin L. Radiologic errors and malpractice: a blurry distinction. AJR Am J Roentgenol. 2007; 189:517–522.
21. Borgstede JP, Lewis RS, Bhargavan M, Sunshine JH. RADPEER quality assurance program: a multifacility study of interpretive disagreement rates. J Am Coll Radiol. 2004; 1:59–65.
22. Arendts G, Manovel A, Chai A. Cranial CT interpretation by senior emergency department staff. Australas Radiol. 2003; 47:368–374.
23. Kim ES, Yoon DY, Lee HY, Ku YJ, Han A, Yoon SJ, et al. Comparison of emergency cranial CT interpretation between radiology residents and neuroradiologists: transverse versus three-dimensional images. Diagn Interv Radiol. 2014; 20:277–284.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download