Abstract
Placement of an implantable venous access port (IVAP) is a popular procedure for repeated and intermittent chemotherapy in patients with malignancy. In this article, we present various IVAP related complications. In addition, we review the technical tips to prevent and manage the complications. It is important that the operator should keep the mechanism of the complications in mind, perform a careful procedure for prevention, and manage the complication properly and immediately in case of its development for safety and satisfaction of the patients.
Figures and Tables
Fig. 2
Chest PA shows placement of an implantable venous access port (IVAP) with an asymmetric shape via the right axillary vein. The radiopaque "CT" marking indicates good position and availability of the IVAP without flip.

Fig. 3
A 68-year-old woman with stomach cancer presented with swelling in the right infraclavicular area 3 weeks after placement. She had a history of warfarinization after placement. Sonographic examination shows a heterogeneous echoic hematoma around the cuff (arrow).

Fig. 4
Clamping of the peel-away sheath is useful for prevention of air embolism during removal of the dilator and insertion of the catheter.

Fig. 5
A 77-year-old man with lung cancer presented with malfunction of the port due to occlusion 1 month after placement. Cathetogram shows leakage of contrast media into the axillary vein. Inspection of the catheter after removal showed a small laceration of the catheter that correlated with the direction of teeth of Kelly and the suggestive cause of catheter leakage was pinching of the catheter during placement.
Fig. 6
A 66-year-old man with colon cancer presented with pain, swelling and discoloration around the puncture site after the first infusion of the chemotherapeutic agent. Inspection of the catheter after removal showed perforation of the catheter near the apex of the curve and the suggestive cause of catheter leakage was puncture of the catheter during suturing of the vein puncture site. The lesion healed with local wound care.

Fig. 8
Adhesive dermatitis. Erythema of the skin is correlated with the application site of the plaster for dressing.

Fig. 9
The photogram obtained 7 days after placement in a 59-year-old woman shows vesicle at the upper margin of the application site of the plaster for dressing (arrow).

Fig. 10
The photogram obtained the next day after closing the wound with Histoacryl shows complete approximation and good cosmetic results without any stitch marks caused by the suture.

Fig. 11
Neck CT obtained after placement via posterior triangular access shows the direction of the catheter (arrows) towards the posteromedial side lateral to the sternocleidomastoid muscle.
M = sternocleidomastoid muscle, V = right internal jugular vein
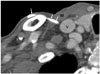
Fig. 12
The photogram of the patient with an infection of the pocket shows erythema and a small hole covered by a clot on skin over the implantable venous access port. There was pus-like discharge during removal.

Fig. 14
Chest PA obtained just after placement in a 72-year-old woman with colon cancer shows the location of the catheter tip at the junction of the right internal jugular and subclavian veins (A). Axial (B) and coronal reformatted (C) images of the chest CT obtained 2 months after placement show thrombosis of the right internal jugular vein (arrowheads) around the catheter (thin arrow) and stenosis of the right brachiocephalic vein (white arrows).

Fig. 15
Chest PA obtained after placement with puncture of the subclavian vein with use of an anatomical landmark by the surgeon shows extrinsic compression of the catheter (arrow) at the crossing point of the clavicle and the first rib. Pinch-off syndrome may develop due to repeated stress.

Fig. 16
Chest PA after placement via the right internal jugular vein in a 58-year-old woman with pendulous breast shows extravascular migration of the implantable venous access port and location of the catheter in the infraclavicular area.

Fig. 17
Chest PA obtained just after placement shows the catheter tip in the superior vena cava (SVC) (arrow) (A). Follow-up image obtained after 2 months shows location of the catheter tip (arrow) at the junction of both brachiocephalic veins due to failure of return to the SVC and downward migration of the implantable venous access port chamber (white arrows) (B).
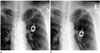
Fig. 18
Chest PA shows intravascular migration of the catheter into the right internal jugular vein.

Fig. 19
Chest lateral view shows the base of the port towards the anterior direction due to flipping over.

References
1. Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. 1982; 92:706–712.
2. Morris SL, Jaques PF, Mauro MA. Radiology-assisted placement of implantable subcutaneous infusion ports for long-term venous access. Radiology. 1992; 184:149–151.
3. Deogaonkar K, Shokrollahi K, Dickson WA. Haemothorax: a potentially fatal complication of subclavian cannulation--a case report. Resuscitation. 2007; 72:161–163.
4. Simpson KR, Hovsepian DM, Picus D. Interventional radiologic placement of chest wall ports: results and complications in 161 consecutive placements. J Vasc Interv Radiol. 1997; 8:189–195.
5. Ballarini C, Intra M, Pisani Ceretti A, Cordovana A, Pagani M, Farina G, et al. Complications of subcutaneous infusion port in the general oncology population. Oncology. 1999; 56:97–102.
6. Schwarz RE, Groeger JS, Coit DG. Subcutaneously implanted central venous access devices in cancer patients: a prospective analysis. Cancer. 1997; 79:1635–1640.
7. Di Carlo I, Cordio S, La Greca G, Privitera G, Russello D, Puleo S, et al. Totally implantable venous access devices implanted surgically: a retrospective study on early and late complications. Arch Surg. 2001; 136:1050–1053.
8. Skolnick ML. The role of sonography in the placement and management of jugular and subclavian central venous catheters. AJR Am J Roentgenol. 1994; 163:291–295.
9. Dariushnia SR, Wallace MJ, Siddiqi NH, Towbin RB, Wojak JC, Kundu S, et al. Quality improvement guidelines for central venous access. J Vasc Interv Radiol. 2010; 21:976–981.
10. Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001; 286:700–707.
11. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 1993; 87:1557–1156.
12. Song D, Yun S, Cho S. Posterior triangle approach for lateral in-plane technique during hemodialysis catheter insertion via the internal jugular vein. Ann Surg Treat Res. 2015; 88:114–117.
13. Dilisio R, Mittnacht AJ. The "medial-oblique" approach to ultrasound-guided central venous cannulation--maximize the view, minimize the risk. J Cardiothorac Vasc Anesth. 2012; 26:982–984.
14. Seo TS, Song MG, Kang EY, Lee CH, Yong HS, Doo K. A single-incision technique for placement of implantable venous access ports via the axillary vein. J Vasc Interv Radiol. 2014; 25:1439–1446.
15. Walser EM. Venous access ports: indications, implantation technique, follow-up, and complications. Cardiovasc Intervent Radiol. 2012; 35:751–764.
16. Patel IJ, Davidson JC, Nikolic B, Salazar GM, Schwartzberg MS, Walker TG, et al. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2012; 23:727–736.
17. Thomopoulos T, Meyer J, Staszewicz W, Bagetakos I, Scheffler M, Lomessy A, et al. Routine chest X-ray is not mandatory after fluoroscopy-guided totally implantable venous access device insertion. Ann Vasc Surg. 2014; 28:345–350.
18. Vesely TM. Air embolism during insertion of central venous catheters. J Vasc Interv Radiol. 2001; 12:1291–1295.
19. Hsu M, Trerotola SO. Air embolism during insertion and replacement of tunneled dialysis catheters: a retrospective investigation of the effect of aerostatic sheaths and over-the-wire exchange. J Vasc Interv Radiol. 2015; 26:366–371.
20. Kolbeck KJ, Stavropoulos SW, Trerotola SO. Over-the-wire catheter exchanges: reduction of the risk of air emboli. J Vasc Interv Radiol. 2008; 19:1222–1226.
21. Eiferman RA, Snyder JW. Antibacterial effect of cyanoacrylate glue. Arch Ophthalmol. 1983; 101:958–960.
22. Narang U, Mainwaring L, Spath G, Barefoot J. In-vitro analysis for microbial barrier properties of 2-octyl cyanoacrylate-derived wound treatment films. J Cutan Med Surg. 2003; 7:13–19.
23. Jan HC, Chou SJ, Chen TH, Lee CI, Chen TK, Lou MA. Management and prevention of complications of subcutaneous intravenous infusion port. Surg Oncol. 2012; 21:7–13.
24. Venkatesan AM, Kundu S, Sacks D, Wallace MJ, Wojak JC, Rose SC, et al. Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. Written by the Standards of Practice Committee for the Society of Interventional Radiology and Endorsed by the Cardiovascular Interventional Radiological Society of Europe and Canadian Interventional Radiology Association [corrected]. J Vasc Interv Radiol. 2010; 21:1611–1630.
25. Baskin KM, Jimenez RM, Cahill AM, Jawad AF, Towbin RB. Cavoatrial junction and central venous anatomy: implications for central venous access tip position. J Vasc Interv Radiol. 2008; 19:359–365.
26. Taxbro K, Berg S, Hammarskjöld F, Hanberger H, Malmvall BE. A prospective observational study on 249 subcutaneous central vein access ports in a Swedish county hospital. Acta Oncol. 2013; 52:893–901.
27. Yildizeli B, Laçin T, Batirel HF, Yüksel M. Complications and management of long-term central venous access catheters and ports. J Vasc Access. 2004; 5:174–178.
28. Shim J, Seo TS, Song MG, Cha IH, Kim JS, Choi CW, et al. Incidence and risk factors of infectious complications related to implantable venous-access ports. Korean J Radiol. 2014; 15:494–500.
29. Fischer L, Knebel P, Schröder S, Bruckner T, Diener MK, Hennes R, et al. Reasons for explantation of totally implantable access ports: a multivariate analysis of 385 consecutive patients. Ann Surg Oncol. 2008; 15:1124–1129.
30. Bouza E, Burillo A, Muñoz P. Catheter-related infections: diagnosis and intravascular treatment. Clin Microbiol Infect. 2002; 8:265–274.
31. Balestreri L, De Cicco M, Matovic M, Coran F, Morassut S. Central venous catheter-related thrombosis in clinically asymptomatic oncologic patients: a phlebographic study. Eur J Radiol. 1995; 20:108–111.
32. De Cicco M, Matovic M, Balestreri L, Panarello G, Fantin D, Morassut S, et al. Central venous thrombosis: an early and frequent complication in cancer patients bearing long-term silastic catheter. A prospective study. Thromb Res. 1997; 86:101–111.
33. Bern MM, Lokich JJ, Wallach SR, Bothe A Jr, Benotti PN, Arkin CF, et al. Very low doses of warfarin can prevent thrombosis in central venous catheters. A randomized prospective trial. Ann Intern Med. 1990; 112:423–428.
34. Beathard GA. Catheter thrombosis. Semin Dial. 2001; 14:441–445.
35. Hoshal VL Jr, Ause RG, Hoskins PA. Fibrin sleeve formation on indwelling subclavian central venous catheters. Arch Surg. 1971; 102:353–358.
36. Puel V, Caudry M, Le Métayer P, Baste JC, Midy D, Marsault C, et al. Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports. Cancer. 1993; 72:2248–2252.
37. Song MG, Seo TS, Kang EY, Yong HS, Seo JH, Choi YY. Innominate vein stenosis in breast cancer patients after totally implantable venous access port placement. J Vasc Access. 2015; 16:315–320.
38. Schwarz RE, Coit DG, Groeger JS. Transcutaneously tunneled central venous lines in cancer patients: an analysis of device-related morbidity factors based on prospective data collection. Ann Surg Oncol. 2000; 7:441–449.
39. Yerdel MA, Karayalcin K, Aras N, Bozatli L, Yildirim E, Anadol E. Mechanical complications of subclavian vein catheterization. A prospective study. Int Surg. 1991; 76:18–22.
40. Owens CA, Bui JT, Knuttinen MG, Gaba RC, Carrillo TC. Pulmonary embolism from upper extremity deep vein thrombosis and the role of superior vena cava filters: a review of the literature. J Vasc Interv Radiol. 2010; 21:779–787.
41. Daeihagh P, Jordan J, Chen J, Rocco M. Efficacy of tissue plasminogen activator administration on patency of hemodialysis access catheters. Am J Kidney Dis. 2000; 36:75–79.
42. Kuo YS, Schwartz B, Santiago J, Anderson PS, Fields AL, Goldberg GL. How often should a port-A-cath be flushed? Cancer Invest. 2005; 23:582–585.
43. Vescia S, Baumgärtner AK, Jacobs VR, Kiechle-Bahat M, Rody A, Loibl S, et al. Management of venous port systems in oncology: a review of current evidence. Ann Oncol. 2008; 19:9–15.
44. Hinke DH, Zandt-Stastny DA, Goodman LR, Quebbeman EJ, Krzywda EA, Andris DA. Pinch-off syndrome: a complication of implantable subclavian venous access devices. Radiology. 1990; 177:353–356.
45. Surov A, Wienke A, Carter JM, Stoevesandt D, Behrmann C, Spielmann RP, et al. Intravascular embolization of venous catheter--causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr. 2009; 33:677–685.
46. Song MG, Seo TS, Kim YH, Cho SB, Jung E, Chung HH, et al. Effectiveness of breast fixation to reduce migration of the tip of a totally implantable venous access port in women. J Vasc Access. 2016; 06. 01. [Epub ahead of print]. DOI: 10.5301/jva.5000565.
47. Rasuli P, Hammond DI, Peterkin IR. Spontaneous intrajugular migration of long-term central venous access catheters. Radiology. 1992; 182:822–824.
48. Ahn KS, Yoo K, Cha IH, Seo TS. Spontaneously migrated tip of an implantable port catheter into the axillary vein in a patient with severe cough and the subsequent intervention to reposition it. Korean J Radiol. 2008; 9:S81–S84.
49. McNulty NJ, Perrich KD, Silas AM, Linville RM, Forauer AR. Implantable subcutaneous venous access devices: is port fixation necessary? A review of 534 cases. Cardiovasc Intervent Radiol. 2010; 33:751–775.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download