Abstract
Purpose
To determine the computed tomography (CT) findings predictive of neurological deficits in thoracolumbar spine injuries.
Materials and Methods
One hundred two patients with thoracolumbar spinal burst fractures, after excluding the patients with brain and cervical cord injuries and unconsciousness, who underwent consecutive spine 128-multidetector CT scan formed the study group. The neurological findings were clinically classified as no deficit (n = 58), complete deficit with paraplegia (n = 22), and incomplete deficit with either motor or sensory impairment (n = 22). The following four CT imaging parameters were analyzed: the level of the main burst fracture as the cord (n = 44) and the cauda equina (n = 58) levels; the extent of canal encroachment as central canal ratios (CCRs) below 0.5 (n = 43) and above 0.5 (n = 59); the degree of laminar fracture as no fracture (n = 33), linear fracture (n = 7), separated fracture (n = 27), and displaced fracture (n = 35); fractured vertebra counted as single (n = 53) and multiple (n = 49).
Figures and Tables
 | Fig. 1The value of the central canal ratio is the narrowest diameter of the canal (b) divided by the normal anteroposterior diameter (a) on the axial CT scan. |
 | Fig. 2The grades of laminar fractures.
A. A 23-year-old woman with an incomplete neurological deficit. The axial CT scan shows a grade 1 linear laminar fracture of the 2nd lumbar vertebra (arrow).
B. A 48-year-old man with a complete neurological deficit. The axial CT scan shows a grade 2 separated laminar fracture of the 8th thoracic vertebra (arrow).
C. A 45-year-old woman with a complete neurological deficit. The axial CT scan shows a grade 3 displaced laminar fracture of the 11th thoracic vertebra (arrow).
|
 | Fig. 3A 52-year-old male with an incomplete neurological deficit in multiple vertebral injuries.
A. The sagittal CT scan demonstrates one burst fracture of the 1st lumbar vertebra (thick black arrow) and three compression fractures of the 2nd to the 4th lumbar vertebrae (thin black arrows).
B. The sagittal MR T2 image illustrates one burst fracture of the 1st lumbar vertebra (thick white arrow) and three compression fractures of the 2nd to the 4th lumbar vertebrae (thin white arrows).
|
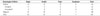
Table 1
Neurological Deficits Related with the Levels of Main Burst Fracture

| Neurological Deficits | Cord (Conus Medullaris) | Cauda Equina | Total |
|---|---|---|---|
| Positive | 27 (10) | 17 | 44 |
| Complete | 22 (5) | 0 | 22 |
| Incomplete | 5 (5) | 17 | 22 |
| Negative | 17 (12) | 41 | 58 |
| Total | 44 (22) | 58 | 102 |
Table 2
Neurological Deficits Related with the CCRs

| Neurological Deficits | CCR ≤ 0.5 | CCR > 0.5 | Total |
|---|---|---|---|
| Positive | 29 | 15 | 44 |
| Complete | 12 | 10 | 22 |
| Incomplete | 17 | 05 | 22 |
| Negative | 14 | 44 | 58 |
| Total | 43 | 59 | 102 |
Table 3
Neurological Deficits Related with the Laminar Fractures

| Neurological Deficits | Laminar Fractures | Total | |||
|---|---|---|---|---|---|
| Displaced* | Separated | Linear | No Fracture | ||
| Positive | 28 | 8 | 2 | 6 | 44 |
| Complete | 19* | 2 | 1 | 0 | 22 |
| Incomplete | 9 | 6 | 1 | 6 | 22 |
| Negative | 7 | 19 | 5 | 27 | 58 |
| Total | 35 | 27 | 7 | 33 | 102 |
References
1. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8:817–831.
2. Patel AA, Dailey A, Brodke DS, Daubs M, Harrop J, Whang PG, et al. Thoracolumbar spine trauma classification: the Thoracolumbar Injury Classification and Severity Score system and case examples. J Neurosurg Spine. 2009; 10:201–206.
3. Khurana B, Sheehan SE, Sodickson A, Bono CM, Harris MB. Traumatic thoracolumbar spine injuries: what the spine surgeon wants to know. Radiographics. 2013; 33:2031–2046.
4. Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970; 52:1534–1551.
5. Kim NH, Lee HM, Chun IM. Neurologic injury and recovery in patients with burst fracture of the thoracolumbar spine. Spine (Phila Pa 1976). 1999; 24:290–293. discussion 294.
6. Petersilge CA, Pathria MN, Emery SE, Masaryk TJ. Thoracolumbar burst fractures: evaluation with MR imaging. Radiology. 1995; 194:49–54.
7. Slosar PJ Jr, Patwardhan AG, Lorenz M, Havey R, Sartori M. Instability of the lumbar burst fracture and limitations of transpedicular instrumentation. Spine (Phila Pa 1976). 1995; 20:1452–1461.
8. Lee JY, Vaccaro AR, Lim MR, Oner FC, Hulbert RJ, Hedlund R, et al. Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci. 2005; 10:671–675.
9. Fontijne WP, de Klerk LW, Braakman R, Stijnen T, Tanghe HL, Steenbeek R, et al. CT scan prediction of neurological deficit in thoracolumbar burst fractures. J Bone Joint Surg Br. 1992; 74:683–685.
10. Mohanty SP, Bhat NS, Abraham R, Ishwara Keerthi C. Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008; 16:20–23.
11. Tisot RA, Avanzi O. Laminar fractures as a severity marker in burst fractures of the thoracolumbar spine. J Orthop Surg (Hong Kong). 2009; 17:261–264.
12. Lee IS, Kim HJ, Lee JS, Kim SJ, Jeong YJ, Kim DK, et al. Dural tears in spinal burst fractures: predictable MR imaging findings. AJNR Am J Neuroradiol. 2009; 30:142–146.
13. Saifuddin A, Burnett SJ, White J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine (Phila Pa 1976). 1998; 23:1452–1456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download