INTRODUCTION
Plain radiography is still very important in the management of newborn babies, especially in premature babies who were born earlier than expected (1). Prematurity involves various lung problems, including respiratory distress syndrome (RDS), patent ductus arteriosus, infection, chronic lung disease, and etc. Transient tachypnea of the newborn (TTN) (also known as wet lung) and meconium aspiration syndromes are more often seen in term or near-term babies. Many tubes and catheters as well as monitoring devices are used for newborn infants on intensive care and the plain radiography is essential for identifying their proper position (2).
BASIC CONSIDERATION
At birth, rapid clearing of the fetal lung fluid takes place in most normal infants. However, in some infants, fluid clearance may be delayed and a small amount of fluid can remain in the alveoli, which may lead to air space disease. In severely immature infants, it can be more pronounced with hazy lungs mimicking RDS or pneumonia.
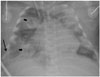
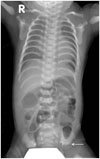
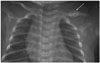
Plain chest radiographs in normal newborn infants show relatively hyperlucent lung, small hilum, and increased cardiothoracic ratios even in cases with no specific cardiac problems (1). The heart is often rounded in appearance due to persistent right heart dominancy. The thymus is relatively prominent in the infants and draped around the heart constituting the cardiothymic silhouette. Sometimes it shows triangular projection laterally, which is known as a "sail" sign (Fig. 1A). When the thymus is large and the patient is rotated, it may mimic atelectasis or other pathology (Fig. 1B). The thymic size varies with the infant's condition or respiratory status. In the newborn infants, especially in premature babies, the skin can be easily folded, resulting in linear artifacts on radiography simulating pneumothorax (Fig. 2).
In neonates under intensive care, chest anterior-posterior (AP) radiographs are taken in supine position, which results in relatively prominent cardiothymic silhouette. The cross-table lateral projection can help to detect a small amount of pneumothorax seen in the non-dependent anterior chest. The plain chest examination is commonly extended to cover the abdomen to visualize the status of bowel loops simultaneously, although its routine use is not recommended because of radiation overexposure.
Various tubes and catheters are seen on plain radiographs and determining whether their position is optimal or not is important to avoid serious complications. The endotracheal tube should be positioned in the middle of the clavicles and carina level, which is approximately 2 cm above the carina. Tube position is affected by neck flexion or rotation. The central venous catheter is considered optimal with its tip position in the region of the superior vena cava (or inferior vena cava) and right atrium junction. The umbilical arterial catheter (UAC) goes downwardly first and then upwardly via the internal iliac artery and common iliac artery before entering the aorta (Fig. 3). So, the UAC always shows a hairpin turn below the umbilicus. On the other hand, the umbilical venous catheter (UVC) proceeds directly upward and then enters the left portal vein at the umbilical portion. After joining the left portal vein, the UVC goes up to the inferior vena cava through the ductus venosus and hepatic vein. The localization of the tip of the UAC should be in avoidance of the major branches such as the arch vessels and renal arteries: high-type UAC in between T6 and T9 vertebral body levels and low-type at L3–4 level. The tip of UVC is proper when it is at the inferior vena cava and right atrium junction near the right hemidiaphragm. Malpositioned UVC tip increases complication rates such as venous thrombosis or hepatic parenchymal necrosis (3). When the UVC is placed too high, it can reach even up to the pulmonary vein across the patent foramen ovale (Fig. 4).
NEONATAL RESPIRATORY DISTRESS
Clinically, respiratory distress in the newborn presents with nasal flaring, subcostal retraction, tachypnea or apnea, grunting, cyanosis, and poor feeding. Neonatal respiratory distress has diverse etiologies of intrapulmonary or extrapulmonary origin. The first postnatal chest radiography is very important to suspect or exclude intrapulmonary, intrathoracic, or extrathoracic etiologies. Clinical information about prenatal history and gestational age is helpful to classify the disease together with lung volume (over or underaeration). Among the long list of the differential diagnoses of respiratory distress in newborns, we discuss relatively common medical diseases (RDS, TTN, meconium aspiration syndrome, and neonatal pneumonia) and surgical conditions (congenital diaphragmatic hernia and esophageal atresia). In addition, we briefly review complications during intensive care including air leaks and bronchopulmonary dysplasia (BPD).
Respiratory Distress Syndrome (Hyaline Membrane Disease)
RDS, also known as hyaline membrane disease or surfactant deficiency disease, is seen typically in neonates of 26 through 33 gestational weeks and low birth weight. The pathogenesis of RDS is closely related to lung maturity and ability of surfactant synthesis. Surfactant is a lipoprotein for diminishing alveolar surface tension and enhancing lung compliance. Surfactant deficiency leads to atelectasis, hypoventilation, ventilation-perfusion mismatches, hypoxemia, and acidosis. The risk factors for RDS include prematurity, fetal distress, maternal diabetes, cesarean section, patent ductus arteriosus, etc. (4). Postnatal surfactant and steroid as well as prenatal steroid to a woman with premature labor are used for treatment.
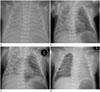
On chest radiographs, RDS show underaerated lungs with variable degrees of opacities from granular lungs to total white-out (Fig. 5A). The lung volumes are typically small since its pathophysiology is essentially underinflated alveoli and microatelectasis. Small lung volume is a very useful finding that can be differentiated from other respiratory diseases of newborn babies. Air bronchograms are commonly seen in the central regions and are more pronounced when the endotracheal tube is placed. The mechanical ventilation and exogenous surfactant are the basis of therapy and improvement in lung aeration with clearing of lung opacifications is observed on serial films after surfactant treatment (Fig. 5B). Transient asymmetric clearing of the both lungs is common (5). Complications of RDS may be seen on follow-up radiographs, including air leak, pulmonary edema and/or hemorrhage. The chest radiographic findings may be superimposed by patent ductus arteriosus with pulmonary edema or infection.
Transient Tachypnea of the Newborn
Wet lung, or TTN, is seen in term or near-term babies. It involves fluid retention in alveolar spaces and interstitium. The fetal lung fluid is removed via lymphatics, capillaries, and through the trachea at delivery. Persistent lung fluid from any etiology leads to clinical syndrome with signs of varying degree respiratory distress. The risk factors include cesarean section, breech presentation, low birth weight, and maternal diabetes. Radiographic findings are those of pulmonary congestion and interstitial edema with cardiomegaly, hyperaeration and pleural effusion (Fig. 6A). Engorged lymphatics may account for streaky or strand like densities. The right minor fissure is commonly accentuated, due to interposed pleural fluid. Rapid clearing is typical within 24 to 48 hours (Fig. 6B).
Meconium Aspiration Syndrome
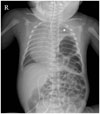
Meconium is thick and viscous material contained in the fetal colon that is passed either as normal process or a response to fetal distress. Fetal distress causes bowel movements and meconium passage in utero; subsequently, contaminated meconium may be aspirated into the baby's airway in utero or during delivery (6). Meconium passage represents neuronal stimulation by maturation of the gastrointestinal tract; hence, meconium is rarely found in amniotic fluid before 34 gestational weeks of age. This can explain why this syndrome is more commonly found in term or near-term babies. Lung changes occur by ways of airway obstruction and chemical irritation of meconium. Aspirated meconium particles mechanically occlude the bronchioles. So, chest radiographs show mixed areas of emphysema and atelectasis with coarse irregular densities (Fig. 7). Overall lung volume is usually increased. Air leak including pneumothorax is common and pulmonary hypertension is a major prognostic determinant. Chemical pneumonitis can follow and superimposed infection is also frequent: therefore, follow-up radiographs should be interpreted with caution.
Neonatal Pneumonia
Pneumonia significantly affects the morbidity and mortality in newborn infants and is closely related to neonatal sepsis. Neonatal pneumonia can be acquired from the mother in utero (congenital), during delivery, or from postnatal infection in relation to NICU care. The pathogen for neonatal pneumonia is most commonly bacterial although many viruses and fungi can infect neonatal lungs (7). However, the specific diagnosis is a challenge because identification of specific pathogen is difficult regardless of antibiotic therapy and clinical manifestations are nonspecific in neonates. The single most common pathogen for neonatal pneumonia is group B beta hemolytic streptococcus (GBS), which is known to mimick RDS on radiographs. Unilateral lung involvement and presence of pleural effusion favor GBS pneumonia rather than RDS. Radiographic features of neonatal pneumonia are also nonspecific with a wide spectrum of chest findings mimicking RDS, TTN, or meconium aspiration. Pneumonia may coexist with RDS or meconium aspiration syndrome. Infants with bacterial pneumonia may show retriculo-nodular densities or asymmetric haziness involving one or both sides of the lungs: pleural effusion, cavitation, or pneumatocele can be associated (Fig. 8).
Air Leak
In the newborn infants with ventilator therapy, barotrauma and alveolar overdistension may lead to air leak. The positive pressure ventilation applied to the non-compliant lung of premature infants increases the chance of air leak. Overinflated terminal bronchioles and alveoli rupture and air dissects through the interstitium (pulmonary interstitial emphysema), which in turn, moves into the mediastinum (pneumomediastinum) or pleural spaces (pneumothorax) (Fig. 9). Interstitial emphysema is fixed in appearance throughout the respiratory cycle and the lung volumes are generally increased. High frequency oscillatory ventilation is often used for alleviating barotraumas and air leak phenomena.
Localized gas collection in the posterior mediastinum may be encountered in some cases on ventilation therapy mostly in association with pneumomediastinum (Fig. 10). It has been described as inferior pulmonary ligament air or infraazygos pneumomediastinum although the two conditions are not exactly the same in terms of the anatomic space (8). Retrocardiac location, oval shape and outer convexity to the left side are characteristic findings on chest AP radiographs; linear or elongated air collection can be identified below the hilum on the lateral radiograph (Fig. 10B). As pneumomediastinum resolves, this inferior pulmonary ligament air also decreases despite a possible time lag (Fig. 10C).
Bronchopulmonary Dysplasia
BPD is a chronic pulmonary syndrome in premature babies who have been treated with oxygen and positive pressure ventilation for RDS, persistent pulmonary hypertension, or other pulmonary disease (9). Longstanding respiratory difficulty requiring oxygen therapy along with characteristic radiographic findings are used in the diagnosis of BPD. The pathogenesis of BPD is still not fully understood but is likely to be closely related to barotraumas, oxygen toxicity, inflammation with its mediators, infection, volume overload, and nutrition. In clinical practice, this results in a vicious cycle of lung damage and ventilator need. Majority of infants with BPD survive and chest radiographic findings appear to improve with time. Cor pulmonale can be associated and recurrent viral infection is problematic in infants with BPD. The pulmonary function test is frequently abnormal and the CT scan is almost always abnormal in BPD survivors (410).
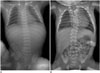
Radiographically, an initial finding is mainly interstitial edema, followed by mixed patterns of edema, atelectasis and hyperaeration (Fig. 11). Irregular opacities, fibrotic scar, air trapping, hyperaeration and atelectasis occur in the late stage. In some cases, the lungs appear "bubbly". Chest CT is very sensitive to demonstrate the late findings in older children (Fig. 12).
Pleural Effusion
Neonatal pleural effusion is rare and many disorders account for pleural fluid formation, including parapneumonic effusion, hydrothorax, chylothorax, or hemothorax (11). Depending on the amount, it may cause respiratory symptoms. Chylothorax is the most common cause in neonatal pleural effusion and congenital chylothorax is closely related to hydrops fetalis (Fig. 13). Chest radiography can suspect the presence of pleural effusion when large enough, but ultrasound is the best modality to detect even a very small amount of pleural fluid.
Surgical Causes of Respiratory Distress
Congenital diaphragmatic hernia is more common on the left side in the form of Bochdalek hernia and commonly associated with other congenital anomalies including cardiac defects. Air-filled bowel loops are seen in the hemithorax and the heart and mediastinum are shifted to the opposite side (Fig. 14). The degree of pulmonary hypoplasia is most important for postsurgical prognosis of the patients (12). It is noteworthy that extralobar pulmonary sequestration can be associated with the diaph-ragmatic defect. The stomach gas can be seen either in the thorax or in the abdomen. The differential diagnosis may include severe diaphragmatic eventration and congenital cystic adenomatoid malformation.
A newborn infant with esophageal atresia may present with respiratory distress. Esophageal atresia can occur with or without trachoesophageal fistula. The esophagus ends blindly regardless of the type, and is detected as air-distended with coiling of the nasogastric tube on plain radiography (Fig. 15). Since the esophageal atresia with distal tracheoesophageal fistula is the most common type, there would be normal appearing bowel gas in the abdominal cavity (Fig. 15B). Vertebral anomalies are not uncommon as a part of VATERL (Vertebral, Anorectal, TracheoEsophageal fistula, Renal, and Limb Anomalies) association.
BONY STRUCTURES
The chest wall and bony thorax should be assessed whenever interpreting chest films. The bell-shaped thorax can be seen in patients with neuromuscular hypotonia. Skeletal dysplasia with a narrow thorax can be associated with pulmonary hypoplasia and neonatal distress. The short ribs and narrow thorax are one of characteristic findings of asphyxiating thoracic dystrophy (non-lethal) (Fig. 16) and thanatophoric dysplasia (usually lethal). The clavicle fracture is common in babies born with difficult delivery (Fig. 17). Vertebral segmentation anomalies are possible with or without rib anomaly in cases of VATERL association (Fig. 15B). Decreased bone mineralization with multiple fractures are seen in osteogenesis imperfecta (Fig. 18).
SUMMARY
RDS is characterized by small hazy lungs with a spectrum ranging from granular lung to total white-out depending on the severity. Wet lung can be differentiated from RDS in relatively large lung volume, cardiomegaly, and pleural effusion with fissure accentuation. In meconium aspiration syndrome, coarse and patchy opacities are typical with or without associated air leak or effusion. Findings of neonatal pneumonia are nonspecific. Surgical disorders and abnormalities of the bony thorax can also be detected on the plain radiographs of newborn infants.




 PDF
PDF ePub
ePub Citation
Citation Print
Print














 XML Download
XML Download