Abstract
Pleomorphic adenoma is the most common neoplasm of the salivary gland. It is usually a well-circumscribed and slow-growing benign tumor. In rare instances, benign pleomorphic adenomas may metastasize and spread to distant sites in which case they are described as metastasizing pleomorphic adenomas. So far, there has been no case report of metastasizing pleomorphic adenoma focusing on radiologic features of the tumor using several different imaging tools. Furthermore, only a few cases of pleomorphic adenoma with metastasis to pulmonary sites have been reported, which usually present as multiple lung nodules. We report a rare case of metastasizing pleomorphic adenoma presenting as a solitary pulmonary nodule without prior history of local tumor recurrence with a particular focus on multimodality imaging of the tumor.
Malignant mixed tumors of the salivary glands are classified into three distinct histologic types: carcinoma ex pleomorphic adenoma, carcinosarcoma (malignant mixed tumor), and metastasizing pleomorphic adenoma. Metastasizing pleomorphic adenoma, a subset of pleomorphic adenoma that spreads to distant sites, is rare; very few cases have been recorded. So far, there has been no case report of metastasizing pleomorphic adenoma focusing on radiologic features of the tumor using multiple imaging tools. Previous reported cases of metastasizing pleomorphic adenoma presenting as pulmonary metastasis involved multiple pulmonary metastases. Also, most patients with metastasizing pleomorphic adenoma have a history of at least one local recurrence of pleomorphic adenoma prior to the detection of distant metastasis (1234567). Therefore, metastasizing pleomorphic adenoma presenting as a solitary pulmonary nodule without a history of local tumor recurrence is a rare manifestation of the disease. This article presents a case of this very rare condition with a discussion of the clinical presentation and a review of the literature; we focus on the radiologic features of the adenoma visualized with multiple imaging modalities.
A 46-year-old female patient visited our hospital for evaluation and treatment of an incidentally discovered solitary pulmonary nodule. She had a medical history of asthma and surgically excised pleomorphic adenoma of the left submandibular gland 9 years prior. An earlier computed tomography (CT) scan of the neck showed a 4.1 × 5.1 cm well-defined non-homogenous enhancing mass in the left submandibular gland with internal calcifications (Fig. 1). She was asymptomatic at the time of the initial visit. All initial laboratory values were within normal ranges.
A chest radiograph showed a 2.4 cm, oval, well-defined solitary pulmonary nodule in the right upper lobe (Fig. 2). We reviewed the chest CT scan and found a 2.2 × 2.0 × 2.2 cm well-defined nodule with lobulated margin and relatively homogenous enhancement (12 to 44 Hounsfield units) in the anterior segment of the right upper lobe. The pulmonary nodule showed no sign of cavitation, necrosis, or calcification (Fig. 3). The initial list of differential diagnoses included sclerosing hemangioma, carcinoid, and, less likely, lung cancer. Magnetic resonance imaging (MRI) was performed in order to further characterize the structure of the affected tissues. MRI revealed intermediate to high signal intensity on T1-weighted images and heterogenous high signal intensity on T2-weighted images with strong enhancement on gadolinum-enhanced T1-weighted images (Fig. 4). A positron emission tomography-computed tomography (PET-CT) scan revealed increased fluorodeoxyglucose (FDG) uptake in the right upper lobe nodule with a maximum standardized uptake value of 4.98 (Fig. 5). There was no other uptake in the maximum intensity projection image of the torso. Because of the notable FDG uptake, which is not usually found in sclerosing hemangioma or carcinoid, we considered lung cancer to be a likely diagnosis after performing PET-CT.
CT-guided core-needle biopsy was performed for pathologic diagnosis. Given the presence of a previous submandibular gland tumor, the pathologic findings were consistent with metastasizing pleomorphic adenoma with the standard features of predominant proliferation of epithelial and mucoepithelial cells, immersed in a chondromyxoid stroma. Immunohistochemistry of the biopsy specimen showed diffuse strong positive reaction for S-100 protein, multifocal weakly positive reaction for smooth muscle actin, and negative reaction for thyroid transcription factor-1 (Fig. 6). Because there was a single metastasizing pulmonary pleomorphic adenoma, a decision to surgically remove the mass was made. Thus, the patient underwent right upper lobe lobectomy with video assisted thoracoscopic surgery. She has exhibited no remarkable postoperative complications during the 15 months since the procedure.
Pleomorphic adenoma is the most common neoplasm of the salivary gland. It is usually a benign, slow-growing, and well-circumscribed tumor. Rarely, pleomorphic adenoma metastasizes to distant sites (1234567). The World Health Organization defines metastasizing pleomorphic adenoma as a "histologically benign pleomorphic adenoma that inexplicably manifests local or distant metastasis" (567). The mechanism underlying the metastatic behavior of salivary pleomorphic adenoma is not clear. The seeming paradox that benign entities occasionally exhibit aggressive behavior and also manifest as multiple metastases is also true for other neoplasms of different organs such as metastatic giant cell tumor of bone, metastasizing leiomyomatosis of the uterus, benign pheochromocytomas of the adrenal gland, lymphangiomatosis of the lymphatic system, and intracranial benign meningioma.
Most patients (72.8%) with metastasizing pleomorphic adenoma have a history of at least a single incidence of local recurrence of pleomorphic adenoma prior to the detection of distant metastasis. A meta-analysis of 81 case reports published from 1942 through 2014 uncovered no reports of metastasizing pleomorphic adenoma as a solitary lung lesion without local tumor recurrence (5). There were two case reports of metastasizing pulmonary pleomorphic adenoma with no history local tumor recurrence that did not cite the number of lung lesions (89). We found incorrect classification in one of the two case reports: it was in fact a case of hepatic metastasizing pleomorphic adenoma. The other case was metastasizing pulmonary pleomorphic adenoma with two lung lesions. Therefore, our case is the first report of solitary pulmonary metastasizing pleomophic adenoma without a history of local tumor recurrence.
CT findings of metastasizing pulmonary pleomorphic adenoma have been reported as multiple, well-defined, variable-sized, ovular or round lung nodules (1234). To our knowledge, MRI findings of metastasizing pulmonary pleomorphic adenoma have not been reported. Our case showed heterogenous high signal intensity on T2-weighted MRI images (Fig. 4). These findings are corroborated by histological findings of a mixture of epithelial tissue intermingled with chondromyxoid stroma. The chondroid area with myxoid interstitium showed high signal intensity, whereas epithelial tissue showed relatively low signal intensity, on T2-weighted images (10). Our case also points out that MRI is better than CT in tissue characterization as it more clearly shows heterogenous components of the lesion. Indeed, CT findings in our case suggested a relatively homogenous appearance. PET-CT scan findings of metastasizing pleomorphic adenoma have been described as FDG-accumulated masses; our case is similar (7).
The treatment of choice for metastasizing pleomorphic adenoma is total surgical resection. The effectiveness of adjuvant primary radiotherapy is a controversial issue. Recurrence after complete surgical removal is rare, and the prognosis is excellent. However, multiple metastases are deemed invariably fatal (12567).
In conclusion, we described multimodality imaging features of a rare case of metastasizing pleomorphic adenoma presenting as a solitary pulmonary nodule without local tumor recurrence based on the findings of CT, MRI, and PET-CT. Hence, radiologists should be aware that metastasizing pleomorphic adenoma may be a differential diagnosis of solitary pulmonary nodule in cases with a prior history of pleomorphic adenoma.
Figures and Tables
Fig. 1
CT scan of the neck of a 46-year-old female with a history of left submandibular pleomorphic adenoma 9 years prior. Axial post-contrast image reveals a 4.1 × 5.1 cm well-defined non-homogenous enhancing mass in the left submandibular gland with internal calcifications (arrow).
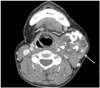
Fig. 2
Chest radiograph of a 46-year-old female with metastasizing pleomorphic adenoma.
A, B. Chest radiograph of posterior-anterior projection (A) and right lateral projection (B) show a 2.4 cm, oval, well-defined solitary pulmonary nodule in the right upper lobe (arrows).
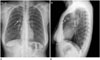
Fig. 3
CT images of metastasizing plemorphic adenoma.
A, B. Axial pre-contrast image (A) and post-contrast image (B) show a 2.2 × 2.0 × 2.2 cm well-defined nodule with lobulated margin and relatively homogenous enhancement (12 to 44 Hounsfield units) in the anterior segment of the right upper lobe without cavitation, necrosis, or calcification.
CT = computed tomography
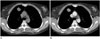
Fig. 4
MR images of metastasizing plemorphic adenoma.
A-C. Axial T1-weighted (A), T2-weighted (B), and post-contrast enhanced T1-weighted image (C) of the lung show a solitary pulmonary nodule in the anterior segment of the right upper lobe with intermediate to high signal intensity on T1-weighted images, heterogenous high signal intensity on T2-weighted images, and with strong enhancement on gadolinium-enhanced T1-weighted images.
MR = magnetic resonance

Fig. 5
FDG PET-CT image of metastasizing pleomorphic adenoma.
Axial fusion image shows increased FDG uptake (maximum standardized uptake value of 4.98) in the right upper lobe.
FDG = fluorodeoxyglucose, PET-CT = positron emission tomography-computed tomography
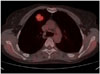
Fig. 6
Microscopic findings of pathologically confirmed metastasizing pleomorphic adenoma.
A, B. Low power micrograph (A) of the metastasizing pleomorphic adenoma shows an intrapulmonary well-demarcated cellular nodule (hematoxylin and eosin, × 20). High power micrograph (B) of another field of the metastasizing pleomorphic adenoma shows proliferation of epithelial and myoepithelial cells immersed in a chondromyxoid stroma (arrow) (hematoxylin and eosin, × 100).

References
1. Rodríguez-Fernández J, Mateos-Micas M, Martínez-Tello FJ, Berjón J, Montalvo JJ, Forteza-González G, et al. Metastatic benign pleomorphic adenoma. Report of a case and review of the literature. Med Oral Patol Oral Cir Bucal. 2008; 13:E193–EE19.
2. Sit KY, Chui WH, Wang E, Chiu SW. Multiple pulmonary metastases from benign pleomorphic adenoma. Asian Cardiovasc Thorac Ann. 2008; 16:62–64.
3. Zhang Y, Gomez-Fernandez CR, Jorda M, Ganjei-Azar P. Fine-needle aspiration (FNA) and pleural fluid cytology diagnosis of benign metastasizing pleomorphic adenoma of the parotid gland in the lung: a case report and review of literature. Diagn Cytopathol. 2009; 37:828–831.
4. Raja V, China C, Masaki KH, Nakano G. Unusual presentations of uncommon tumors: case 1. Benign metastasizing pleomorphic adenoma. J Clin Oncol. 2002; 20:2400–2240.
5. Knight J, Ratnasingham K. Metastasising pleomorphic adenoma: systematic review. Int J Surg. 2015; 19:137–145.
6. Santaliz-Ruiz LE, Morales G, Santini H, Sánchez-Santiago M, Arroyo A. Metastasizing pleomorphic adenoma: a fascinating enigma. Case Rep Med. 2012; 2012:148103.
7. Nouraei SA, Ferguson MS, Clarke PM, Sandison A, Sandhu GS, Michaels L, et al. Metastasizing pleomorphic salivary adenoma. Arch Otolaryngol Head Neck Surg. 2006; 132:788–793.
8. Youngs GR, Scheuer PJ. Histologically benign mixed parotid tumour with hepatic metastasis. J Pathol. 1973; 109:171–172.
9. Landolt U, Zöbeli L, Pedio G. Pleomorphic adenoma of the salivary glands metastatic to the lung: diagnosis by fine needle aspiration cytology. Acta Cytol. 1990; 34:101–102.
10. Kinoshita T, Ishii K, Naganuma H, Okitsu T. MR imaging findings of parotid tumors with pathologic diagnostic clues: a pictorial essay. Clin Imaging. 2004; 28:93–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download