Abstract
Polysplenia syndrome is a rare situs ambiguous anomaly associated with multiple spleens and anomalies of abdominal organs. Because most of the minor anomalies do not cause clinical symptoms, polysplenia syndrome is detected incidentally in the adults. Anomalies of abdominal organs may include multiple spleens of variable size or right-sided spleen, large midline or left-sided liver, midline gallbladder, biliary tract anomalies, short pancreas, right-sided stomach, intestinal malrotation, inferior vena cava interruption with azygos or hemiazygos continuation, and a preduodenal portal vein. As the multidetector computed tomography is increasingly used, situs anomalies will likely to be found with greater frequency in the adults. Therefore, radiologists should become familiar with these rare and peculiar anomalies of abdominal organs in polysplenia syndrome.
Polysplenia syndrome is a rare congenital anomaly of situs ambiguous associated with multiple spleens and midline location of abdominal organs. During embryogenesis, the spleen plays an important role in the normal development and lateralization of visceral organs. Therefore, anomalies of the spleen are associated with many congenital anomalies of other organs and show wide spectrum of abnormalities in the abdominal organs (12). Abdominal anomalies of polysplenia syndrome include multiple spleens, various visceral anomalies including impaired visceral lateralization, gastrointestinal abnormalities, and inferior vena cava (IVC) interruption (123).
The majority of patients with polysplenia syndrome die before five years of age because of severe cardiac defects and only 5–10% of the patients with a normal heart or minor cardiac defects can survive to adulthood. Therefore, polysplenia syndromes are often incidentally found by multidetector computed tomography (MDCT) or magnetic resonance imaging for the evaluation of other medical diseases in the adults (456). Although polysplenia syndrome has some characteristic radiologic features, these anomalies may not present clinical pathognomonic symptoms. To the patient undergoing an abdominal surgery, the anomaly itself may make the surgery difficult and increase the risk of complications (7).
In this article, we illustrate various anomalies of polysplenia syndrome and focus on abdominal organs by MDCT with three-dimensional reconstruction images. It is important for radiologists to understand these unfamiliar features of polysplenia syndrome and not interpret them as other pathologic disease pro-cesses.
The spleen develops from within the dorsal mesogastrium and then incisures on the left side of the dorsal mesogastrium to become the initial splenic primordium during the fifth week of embryogenesis. Therefore, it is regarded that failure of fusion of these incisures can lead to multiple spleens (18).
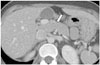
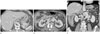
Most patients with polysplenia syndrome have multiple splenic masses of variable size in either left or right side of subphrenic space (Figs. 1, 2) (5). A single lobulated (Fig. 3) and even normal spleens have also been reported (4). The spleens are always located adjacent to the stomach because both the spleen and stomach develop together within the dorsal mesogastrium (18).
The pancreas may be normal, short in size, or have a cleft created by traversing vessels (2411). An annular pancreas and semiannular pancreas also have been reported (12). A short pancreas may be caused by disease processes such as chronic pancreatitis, ischemic atrophy of the pancreatic tail, Kwashiorkor, and viral infection. In contrast, congenital short pancreas is cau-sed by complete or incomplete agenesis of dorsal pancreas so that only the pancreatic head or pancreatic head with small portion of the pancreas body remains (Fig. 7) (1113). The pancre as head may be located in the midline or right side of midline (Figs. 8, 9). Because both the dorsal pancreas and spleen develop from dorsal mesogastrium, their anomalies tend to occur together (18). Endoscopic retrograde cholangiopancreatography must be performed carefully because the short pancreas may be misdiagnosed as pancreas divisum or mass, which can cause pancreatic duct obstruction. Rarely, a short pancreas can induce pancreatitis due to complete agenesis of the dorsal pancreas may lead to sphincter of Oddi dysfunction or ventral pancreas hyperplasia can give rise to increased pancreatic ductal pressure (14151617).
Malrotation or nonrotation of the gastrointestinal tract is commonly observed in polysplenia syndrome (2318). The stomach may be right-sided, the small bowel may be primarily right-sided and the colon left-sided (Figs. 10, 11), and the cecum may be incompletely fixed (2). Although gastrointestinal tract rotational anomalies may be a rare cause of abdominal pain in adults and may cause bowel obstruction, such as midgut volvulus (318).
Around the 25th day of embryogenesis, the blood flow of an embryo makes a transition from symmetric to asymmetric. This determines the visceral sidedness. Anomalies of conotruncus and the atrioventricular canal occur at this time (19).
In polysplenia syndrome, some portions of the IVC may be absent because it is primarily a right-sided structure (1). The intrahepatic IVC may be right-sided, left-sided, or duplicated. In the duplicated or right-sided IVC, the IVC is interrupted and connected to the azygos or hemiazygos vein (Fig. 12), whereas, the left-sided IVC is connected to suprahepatic IVC (4). This is the most frequently encountered anatomical anomaly in polysplenia syndrome, albeit not pathognomonic (1245).
A preduodenal portal vein (PDPV) is a rare anomaly resulting from maldevelopment of portal venous system or malposition of the abdominal viscera. Although PDPV is associated with duodenal atresia, stenosis, web, and annular pancreas; the possibility of duodenal obstruction is low due to its thin wall and low pressure vessel (1111220). PDPV also has been known to cause atrophy of left lateral segment of the liver, selective portal vein obstruction, biliary duct obstruction, long standing malnutrition and cachexia, or toxic and vascular influences (21). PDPV can also give rise to cholelithiasis.
Polysplenia syndrome is a rare complex of congenital anomalies characterized by multiple spleens and various visceral anomalies (23). Visceral anomalies of polysplenia syndrome include right-sided stomach, midline or left-sided liver, short pancreas, IVC anomalies, intestinal malrotation, and a PDPV.
MDCT with contrast enhancement and three-dimensional reconstruction is excellent in visualizing these anomalies by providing clear anatomic detail. Because the wide spectrum of anomalies in polysplenia syndrome do not have pathognomonic radiologic features, the knowledge of various radiologic features plays an important role in the diagnosis of this rare syndrome. In addition, correct diagnosis may decrease both the mortality and morbidity under surgical conditions.
Figures and Tables
 | Fig. 1Polysplenia. Contrast-enhanced axial CT scan shows multiple small discrete splenic tissues (arrows) from the left subphrenic space adjacent to the stomach. |
 | Fig. 2Polysplenia. Contrast-enhanced axial (A) and coronal reformatted (B) images show several large splenic tissues of lobulating contour (arrows). |
 | Fig. 3Single spleen. Contrast-enhanced axial (A) and coronal reformatted (B) images show a single small ovoid spleen on the left side (arrows). |
 | Fig. 4Location and shape of the liver and gallbladder. Contrast-enhanced axial (A) and coronal reformatted (B) images show a normal location and shape of liver and right-sided gallbladder in a polysplenia patient. |
 | Fig. 5Midline gallbladder. Contrast-enhanced axial (A) and coronal reformatted (B) images show the midline location of gallbladder (arrows). Although the liver is located on the right side, the left lateral segment is large and located in the left subphrenic space. |
 | Fig. 6Midline gallbladder and large left lobe of the liver. Contrast-enhanced axial (A, B) and coronal reformatted (C) images show midline location of gallbladder (white arrows). The left lateral segment of the liver is very large (black arrows). Dextrocardia is displayed (black arrowhead) (C). |
 | Fig. 7Short pancreas with agenesis of a dorsal pancreas. Contrast-enhanced axial (A) and coronal reformatted (B) images at the pancreas head level show normal pancreas head (white arrows) developed from the ventral pancreas. Axial CT image at the splenic vein level (C), body and tail of the pancreas is not seen ventral to the splenic vein (black arrow) due to agenesis of the dorsal pancreas. |
 | Fig. 8Right-sided short pancreas. Contrast-enhanced axial CT image shows right-side location of short pancreas head (white arrows).D = duodenum
|
 | Fig. 9Midline short pancreas. Contrast-enhanced axial CT image shows midline location of short pancreas head and body (arrow). |
 | Fig. 10Intestinal malrotation.
A. A contrast-enhanced coronal reformatted CT image. Stomach (S) is located in the left side. Duodenum turns to right side and the duodenojejunal junction (white arrow) is abnormally situated at the right of the midline.
B. In the axial image, the ascending colon is found in the left side of abdomen (black arrow).
C. In coronal reformatted image, most of the small bowel loops are situated in the right side and the ascending colon is located in the left side of abdomen (black arrows).
D. Fluoroscopy during the colonoscopy shows a left-sided colon.
|
 | Fig. 11Intestinal malrotation.
A, B. Contrast-enhanced axial images show left side location of the stomach (black arrows). However, the duodenum is directed from left to right side (white arrows).
C. A coronal reformatted image shows the left-sided appendix (black arrowhead) and terminal ileum (white arrowhead).
|
 | Fig. 12IVC interruption with azygos continuation.
A. Contrast-enhanced axial image shows absence of hepatic segment of the IVC and a dilated azygos vein (arrow) in the retrocrural area adjacent to the descending aorta (Ao).
B, C. Axial (B) and coronal reformatted (C) images show interruption of the IVC (white arrows), a dilated azygos vein (black arrows) and the continuation point (arrowheads).
IVC = inferior vena cava
|
References
1. Muneta S, Sakai S, Fukuda H, Imamura Y, Matsumoto I. Polysplenia syndrome with various visceral anomalies in an adult: embryological and clinical considerations. Intern Med. 1992; 31:1026–1031.
2. Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002; 22:1439–1456.
3. Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: imaging of the heterotaxy syndrome. Radiographics. 1999; 19:837–852. discussion 853-854
4. Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999; 24:178–184.
5. Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983; 4:129–137.
6. Winer-Muram HT, Tonkin IL. The spectrum of heterotaxic syndromes. Radiol Clin North Am. 1989; 27:1147–1170.
7. Esscher T. Preduodenal portal vein--a cause of intestinal obstruction? J Pediatr Surg. 1980; 15:609–612.
8. Gayer G, Zissin R, Apter S, Atar E, Portnoy O, Itzchak Y. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001; 74:767–772.
9. Chandra RS. Biliary atresia and other structural anomalies in the congenital polysplenia syndrome. J Pediatr. 1974; 85:649–655.
10. Gagner M, Munson JL, Scholz FJ. Hepatobiliary anomalies associated with polysplenia syndrome. Gastrointest Radiol. 1991; 16:167–171.
11. Kobayashi H, Kawamoto S, Tamaki T, Konishi J, Togashi K. Polysplenia associated with semiannular pancreas. Eur Radiol. 2001; 11:1639–1641.
12. Maier M, Wiesner W, Mengiardi B. Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. AJR Am J Roentgenol. 2007; 188:W150–W153.
13. Kapa S, Gleeson FC, Vege SS. Dorsal pancreas agenesis and polysplenia/heterotaxy syndrome: a novel association with aortic coarctation and a review of the literature. JOP. 2007; 8:433–437.
14. Jeong JH, Kim GH, Song GA, Lee DG, Moon JY, Cheong JH, et al. Polysplenia syndrome with congenital agenesis of dorsal pancreas presenting as acute pancreatitis and the role of endoscopic ultrasonography in its diagnosis. Korean J Gastroenterol. 2012; 60:47–51.
15. Rakesh K, Choung OW, Reddy DN. Agenesis of the dorsal pancreas (ADP) and pancreatitis - is there an association? Indian J Gastroenterol. 2006; 25:35–36.
16. Nishimori I, Okazaki K, Morita M, Miyao M, Sakamoto Y, Kagiyama S, et al. Congenital hypoplasia of the dorsal pancreas: with special reference to duodenal papillary dysfunction. Am J Gastroenterol. 1990; 85:1029–1033.
17. Gold RP. Agenesis and pseudo-agenesis of the dorsal pancreas. Abdom Imaging. 1993; 18:141–144.
18. Ditchfield MR, Hutson JM. Intestinal rotational abnormalities in polysplenia and asplenia syndromes. Pediatr Radiol. 1998; 28:303–306.
19. Miyabara S, Sugihara H, Kamio A, Oota K, Abe H, Kato S. Atypical polysplenia only with absence of the hepatic segment of inferior vena cava in a middle-aged. Acta Pathol Jpn. 1984; 34:111–116.
20. Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol. 2008; 14:6418–6420.
21. Ishizaki Y, Tanaka M, Okuyama T. Surgical implications of preduodenal portal vein in the adult. Case report and review of the literature. Arch Surg. 1994; 129:773–777.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download