Abstract
Purpose
Materials and Methods
Results
Figures and Tables
 | Fig. 1Patient flow diagram. Data are numbers of patients having right or left colonic diverticulitis. Data in brackets are numbers of patients having right colonic diverticulitis. The disease severity (Ia-IV) was categorized according to the modified Hinchey classification by two radiologist's consensus review of CT images. *Eligible patients were those who underwent abdominopelvic CT and then were documented as having colonic diverticulitis as the final or working diagnosis in the medical record. †At least one of the two radiologists refuted the diagnosis of colonic diverticulitis in their retrospective CT image review. |
 | Fig. 237-year-old man with acute diverticulitis at the ascending colon. Contrast-enhanced transverse CT image shows an inflamed diverticulum (arrow). The modified Hinchey stage was determined as Ia. He did not undergo surgery and had no recurrence. |
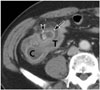 | Fig. 358-year-old man with diverticulitis at the cecum. Contrast-enhanced transverse CT image shows small pericolic abscess (arrow) containing a fecalith (arrowhead). The modified Hinchey stage was determined as Ib. He did not undergo surgery and had no recurrence. C and T indicate cecum and terminal ileum, respectively. |
 | Fig. 455-year-old man with perforated diverticulitis at the cecum with fecal peritonitis. Contrast-enhanced coronal CT image shows spillage of feces (arrows), diverticulosis (arrowheads), and wall thickening of the ascending colon (A). Although inflamed diverticulum was not identified at CT, the two radiologists concordantly reported as right diverticulitis. The modified Hinchey stage was determined as IV. He underwent right hemicolectomy and was pathologically confirmed to have diverticulitis. Fecal spillage was found during surgery. |
Table 1
CT Findings Based on Modified Hinchey Classification

| Stage | Modified Hinchey Classification (9) | CT Findings |
|---|---|---|
| Ia | Confined pericolic inflammation | Confined peridiverticular or pericolic fat stranding with colonic wall thickening |
| Ib | Pericolic or mesocolic abscess | Ia changes and small confined pericolic abscess |
| II | Pelvic, distant intraabdominal or retroperitoneal abscess | Ia changes and larger abscess* at pericolic or distant area |
| III | Generalized purulent peritonitis | Perforated diverticulitis with ruptured abscess and peritonitis† |
| IV | Generalized fecal peritonitis | Diverticular perforation with fecal‡ spillage in the peritoneal cavity |
When CT findings of different stages coexisted in a patient, the highest stage was chosen.
*Greater than 4 cm in axial or coronal diameter, which may need a drainage procedure.
†Localized or generalized ascites and diffuse peritoneal thickening with or without free air.
‡Amorphous mass mottled with gas bubbles, resembling the appearance of stool in the colon.
Table 2
CT Stages Determined by Two Radiologists Based on Modified Hinchey Classification

Table 3
Patient Characteristics

Table 4
Surgery Rate and Recurrence Rate

Data are numbers of patients (and the percentages).
*According to the consensus reading by two radiologists.
†Not including 32 patients lost to follow-up.
‡Not including 32 patients lost to follow-up and 15 patients who already underwent surgery during index admission or within 1 month after index admission.
NA = not applicable




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download