Abstract
Differential diagnosis between spinal metastasis and infectious spondylodiscitis is one of the occasional challenges in daily clinical practice. We encountered an unusual case of spinal metastasis in a 75-year-old female breast cancer patient that mimicked infectious spondylodiscitis. Magnetic resonance imaging (MRI) showed diffuse bone marrow infiltrations with paraspinal soft tissue infiltrative changes in 5 contiguous cervical vertebrae without significant compression fracture or cortical destruction. These MRI findings made it difficult to differentiate between spinal metastasis and infectious spondylodiscitis. Infectious spondylodiscitis such as tuberculous spondylodiscitis was regarded as the more appropriate diagnosis due to the continuous involvement of > 5 cervical vertebrae. The patient's clinical presentation also supported the presumptive diagnosis of infectious spondylodiscitis rather than spinal metastasis. Intravenous antibiotics were administered, but clinical symptoms worsened despite treatment. After pathologic confirmation by computed tomography-guided biopsy, we were able to confirm a final diagnosis of spinal metastasis.
The spine represents the most frequent site of skeletal metastasis. Of the malignant tumors that secondarily involve the spine, carcinomas of the lung, breast, and prostate are most frequently encountered (1).
Magnetic resonance imaging (MRI) is a powerful diagnostic tool that can be used to distinguish spinal metastasis from infectious spondylodiscitis (2). Typical spinal metastasis shows complete replacement of normal bone marrow in the involved non-contiguous vertebrae. Destruction of vertebral bodies with com-pression fracture is occasionally visible. Paraspinal or epidural soft tissue infiltration also implies spinal metastasis, and pedicle involvement can be seen (1). However, it is challenging to differentiate spinal metastasis from infectious spondylodiscitis in the presence of only diffuse bone marrow infiltration with paraspinal soft tissue infiltration in contiguous vertebrae without significant vertebral body collapse or destruction. Furthermore, if the patient has ambiguous laboratory findings and clinical symptoms, an accurate diagnosis can be more difficult to reach.
We experienced an unusual case of breast cancer spinal metastasis that mimicked findings of infectious spondylodiscitis on MRI.
A 75-year-old woman was admitted to our hospital with complaints of right upper extremity weakness and left shoulder pain for 2 months. She had a history of modified radical mastectomy and lymph node dissection for invasive ductal carcinoma of the left breast 3 months prior. There was no evidence of local recurrence in her breast. The patients' vital signs were stable and she had no fever. In laboratory studies, complete blood cell count showed mild leukocytosis (10100/mm3 with 7480/mm3 neutrophils), hemoglobin level of 13.8 g/dL, and platelet count of 227000/mm3. C-reactive protein (CRP) was mildly elevated (4.3 mg/dL). Blood urea nitrogen level was 32.0 mg/dL, and creatinine level was within normal range. The blood culture was negative.
Plain radiography showed only mild disc space narrowing and endplate irregularity in the lower cervical spine without significant destruction or collapse of vertebral bodies (Fig. 1). The initial cervical spine MRI showed diffuse bone marrow infiltrations at contiguous C4 to T1 vertebrae without cortical destruction or vertebral body collapse. The intervertebral disc and disc space were relatively spared. Additionally, paraspinal soft tissue infiltrative change was also visible (Fig. 2). These MRI findings were not compatible with either spinal metastasis or infectious spondylodiscitis. However, the contiguous involvement of > 5 vertebrae without significant cortical destruction favored the diagnosis of infectious spondylodiscitis, such as tuberculous spondylodiscitis, than spinal metastasis. After cervical spine MRI, intravenous vancomycin treatment was started. However, there was no improvement of clinical symptoms after 10 days of vancomycin treatment. Thus, computed tomography (CT)-guided biopsy was performed at C6 and C7 vertebral bodies for an accurate diagnosis. The histologic specimen showed the presence of cells with hyperchromatic nuclei and large eosinophilic cytoplasm. The cells were arranged in nests and glandular-like structures and located between segments of bone and within bone marrow spaces (Fig. 3). These histological results provided evidence for metastatic breast invasive ductal carcinoma.
On the follow-up MRI after 2 weeks, diffuse bone marrow infiltrations were more prominent, and the paraspinal soft tissue infiltrative change also extended to the epidural space. Nevertheless, the vertebral body heights and endplates were still preserved without collapse or compression fracture (Fig. 4).
Subsequently, the patient presented with a drowsy mentality, disorientation, and general weakness. However, the patient's family refused spinal surgery or intensive care unit treatment. Finally, the patient expired due to respiratory failure.
The spine is one of the most common sites of metastasis in many cancers such as breast, prostate, thyroid, and lung cancers. About 60-70% of patients with malignancies have spinal metastasis (34).
On MRI, spinal metastasis shows diffuse vertebral body destruction, low signal intensity on T1-weighted image, and iso- or high signal intensity on T2-weighted image of bone marrow in non-contiguous vertebrae (5). The heights of involved vertebral bodies are usually decreased. However, intervertebral disc and disc space are relatively preserved, and paraspinal soft tissue phlegmon or abscess is uncommon (6).
On the other hand, MRI of infectious spondylodiscitis shows bone marrow infiltrations in contiguous spinal segments with low signal intensity on T1-weighted image and high signal intensity on T2-weighted image of the vertebral body and endplate. Destruction of vertebral bodies and endplates is not as prominent as in spinal metastasis, and only the cortical discontinuity of endplates may be visible. In pyogenic spondylodiscitis, fluid-like signal intensity and enhancement are seen in the involved intervertebral disc, which is relatively spared in tuberculous spondylodiscitis until the late stage. Paraspinal abscess or intra-osseous abscess is another typical MRI finding of infectious spondylodiscitis, which is relatively larger in tuberculous spondylodiscitis than pyogenic spondylodiscitis. Subligamentous spread of inflammatory soft tissue and multi-level contiguous or non-contiguous involvements are also seen in tuberculous spondylodiscitis (27). Some known atypical patterns of infectious spondylodiscitis on MRI include involvement of only 1 vertebral body, involvement of 1 vertebral body and 1 disc, and involvement of 2 bodies without intervening disc involvement, which may be difficult to differentiate from a neoplastic condition (28). Gillams et al. (9) reported the appearance of the temporal evolution and resolution of infectious spondylodiscitis among the 25 patients who underwent MRI. Two of 25 patients (8%) showed atypical infectious spondylodiscitis characterized by abnormal signal changes in 2 adjacent vertebral bodies without abnormal findings in the intervening disc mimicking a neoplastic condition, which became abnormal on the follow-up MRI.
Our case was a very confusing case of spinal metastasis that mimicked findings of infectious spondylodiscitis. On MRI, diffuse bone marrow infiltrations in 5 contiguous cervical vertebrae with paraspinal soft tissue infiltrative changes were visible. To the best of our knowledge, there is no reported case of spinal metastasis in ≥ 5 contiguous vertebrae seen on MRI. Tuberculosis can involve ≥ 3 contiguous or non-contiguous vertebrae, which is not the typical finding in spinal metastasis or pyogenic spondylodiscitis. Intervertebral discs and disc spaces were relatively spared, which is a possible finding in both spinal metastasis and tuberculous spondylodiscitis. However, there was no significant destruction or collapse of vertebral bodies, and no significant abscess formation, which is more characteristic of tuberculosis than pyogenic infection. Epidural extension of the paraspinal soft tissue infiltration was observed on the follow-up MRI, but there was no significant paraspinal abscess formation. These MRI findings were not compatible with infectious spondylodiscitis (including both pyogenic and tuberculous) or spinal metastasis. Laboratory findings of mild leukocytosis and elevated CRP levels made the diagnosis more difficult. The many changes in cervical vertebrae were confirmed as metastasis, and not infection, only after histopathological studies using a CT-guided approach.
In retrospect, despite its likeness to infectious spondylodiscitis, more specifically tuberculous spondylodiscitis, the MRI findings of involvement of marrow in ≥ 5 contiguous vertebrae and paraspinal soft tissue infiltrative change with relatively preserved intervertebral discs and vertebral body cortex were more highly indicative of spinal metastasis than infectious spondylodiscitis. However, the differential diagnosis may still be difficult in similar cases in future. A patient's history of pre-existing malignancy should also be additionally considered in the differential diagnosis; and furthermore, histopathological confirmation by CT-guided biopsy should be performed.
Figures and Tables
Fig. 1
Plain radiography of the cervical spine shows mild disc space narrowing and endplate changes in the lower cervical spine. There is no significant destruction or collapse of vertebral bodies; and trabeculae of vertebral bodies are preserved.
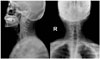
Fig. 2
Initial cervical spine MRI of the 75-year-old female patient. Sagittal (A) and axial (D) T1-weighted MR images show abnormal marrow infiltrations (arrows) in continuous cervical vertebrae without significant destruction or collapse of vertebral bodies. Sagittal (B) and axial (E) T2-weighted MR images show relatively preserved intervertebral disc space (arrowhead) and loss of definition in the endplates. The signal intensities of intervertebral discs are slightly decreased, as compared to the other uninvolved segments. Sagittal (C) and axial (F) contrast-enhanced fat-saturated T1-weighted MR images show enhancement of bone marrow infiltrations and paraspinal soft tissue infiltrative changes (blank arrows). There is no significant enhancement of the intervertebral disc.
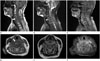
Fig. 3
The histologic specimen from C6 and C7 vertebrae shows the presence of cells with hyperchromatic nuclei and large eosinophilic cytoplasm (blank arrow). The cells are arranged in nests and glandular-like structures between segments of bone and within bone marrow spaces (arrows; A, B). The cells show strong immunoreactivity for cytokeratin, which is one of the representative immunohistochemical markers for breast cancer (C). These histological results provide evidence of metastatic invasive ductal carcinoma.

Fig. 4
Follow-up cervical spine MRI after 2 weeks. Sagittal (A) and axial (D) T1-weighted MR images show more prominent marrow infiltrations (arrows) extending to posterior columns. Vertebral body heights and disc spaces (arrowheads) are still preserved on sagittal (B) and axial (E) T2-weighted MR images. More prominent paraspinal soft tissue infiltrative changes (blank arrows) with epidural extension and posterior ligamentous complex involvement are also noted in the sagittal (C) and axial (F) contrast-enhanced fat-saturated T1-weighted MR images.

References
1. Resnick D, Kransdorf MJ. Bone and joint imaging. 3rd ed. Philadelphia: Elsevier Saunders;2005. p. 1251–1252.
2. Hong SH, Choi JY, Lee JW, Kim NR, Choi JA, Kang HS. MR imaging assessment of the spine: infection or an imitation? Radiographics. 2009; 29:599–612.
3. Alcalay M, Azais I, Brigeon B, Babin P, Vandermarcq P, Debiais F, et al. Strategy for identifying primary malignancies with inaugural bone metastases. Rev Rhum Engl Ed. 1995; 62:632–642.
4. Brage ME, Simon MA. Evaluation, prognosis, and medical treatment considerations of metastatic bone tumors. Orthopedics. 1992; 15:589–596.
5. Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 2011; 2011:769753.
6. Khattry N, Thulkar S, Das A, Khan SA, Bakhshi S. Spinal tuberculosis mimicking malignancy: atypical imaging features. Indian J Pediatr. 2007; 74:297–298.
7. Sans N, Faruch M, Lapègue F, Ponsot A, Chiavassa H, Railhac JJ. Infections of the spinal column--spondylodiscitis. Diagn Interv Imaging. 2012; 93:520–529.
8. James SL, Davies AM. Imaging of infectious spinal disorders in children and adults. Eur J Radiol. 2006; 58:27–40.
9. Gillams AR, Chaddha B, Carter AP. MR appearances of the temporal evolution and resolution of infectious spondylitis. AJR Am J Roentgenol. 1996; 166:903–907.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download