Abstract
We describe a case of an epiphyseal hemangioma in the humeral head of a 20-year-old man. On plain radiographs, the lesion showed no gross abnormality. The computed tomography images demonstrated the presence of an irregular and lobulating osteolytic lesion with a peripheral sclerotic rim and focal cortical defects. The magnetic resonance images showed an ill-defined low signal intensity on T1-weighted images and mixed low and high signal intensities on T2-weighted images. Additionally, ill-defined marrow enhancement with inner low signal lines was noted in this lesion. The patient was treated with curettage and a bone chip graft. The present case is instructive in the differential diagnosis of epiphyseal bone tumors; furthermore, the possibility of an intraosseous hemangioma should also be considered.
A hemangioma of the bone is a benign tumor that may affect any bone and can occur at any age; however, this tumor commonly affects the vertebral bodies and the skull. Involvement of a long bone is infrequent and most hemangiomas that occur in a long tubular bone are located in the metadiaphysis or diaphysis (12). An intraosseous hemangioma rarely involves in the epiphysis of the long bone and only a few cases of an epiphyseal hemangioma have been previously reported (3456).
We present a case of a symptomatic hemangioma that affected the epiphysis of the humeral head and describe the associated radiographic, computed tomography (CT), and magnetic resonance imaging (MRI) findings. As the imaging findings were similar to findings for the vertebral body hemangiomas on CT and MRI, the diagnosis was considered preoperatively.
A 20-year-old man presented with dull pain for three months in the right shoulder. The patient had no traumatic history or shoulder dislocation, and he had not been suffering from known arthritis. Radiographs of the right shoulder joint (Fig. 1) showed no gross abnormality in the humeral head. On CT images (Fig. 2), an irregular and lobulating osteolytic lesion was visible with a peripheral sclerotic rim and focal cortical defects. Magnetic resonance images (Fig. 3) showed irregular low signal intensity on T1-weighted images, mixed low and high signal intensities on T2-weighted images, and inhomogeneous enhancement. In addition, inner and peripheral low signal lines in this lesion were observed on all MR sequences. We thought that these low signal intensity lines were probably due to thickened bony trabeculae. Based on the above multi-modality imaging findings, we diagnosed the intraosseous lesion of the humeral head as an intraosseous hemangioma.
The patient underwent open surgery, including a careful curettage and a bone chip graft. During surgery, multiple dark brownish fragments were obtained and a histopathological examination of these fragments showed the presence of multiple dilated vascular channels and the irregular architecture of the thickened bony trabeculae (Fig. 4A). Immunostaining for the expression of factor VIII revealed a variety of different sizes and shapes of vascular channels, lined by endothelial cells (Fig. 4B). Based on these findings, an intraosseous hemangioma was diagnosed.
A hemangioma may affect any bone, but commonly affects the vertebral bodies and the skull. Intraosseous hemangiomas can be easily diagnosed when lesions are located at these typical sites (7). When a lesion is located in the vertebral body, it has a coarse, vertical trabecular pattern as seen on radiographs and CT. Typically, a CT scan demonstrates a characteristic appearance-the so-called polka-dot pattern or a honeycomb pattern (12). Generally, a vertebral hemangioma shows high signal intensity on both T1- and T2-weighted images (8). The loss of hematopoietic cells in the gaps of hemangiomas and apparent increase in the fat component can produce an increased signal intensity on T1-weighted images in hemangiomas of the vertebral bodies (7). However, vertebral hemangiomas can demonstrate variable signal intensity on T1-weighted images, based on the degree of adipose tissue present (9).
Intraosseous hemangiomas rarely affect the long tubular bones and hemangiomas of the long tubular bones usually occur in the metadiaphyseal or diaphyseal portion of the bones of the lower extremities and ribs (127). Radiographically, the intraosseous hemangioma is seen as an osteolytic area with trabeculation, creating a soap bubble or honeycomb appearance as a result of the expanding, proliferating, engorging vessels and thickened, remodeled bone trabeculae (7). MR findings of an intraosseous hemangioma have not been well documented, except for vertebral body or skull hemangiomas (10). Generally, medullary hemangiomas of long bones show a low signal on T1-weighted images and a high signal on T2-weighted images. The high signal on T2-weighted images can be explained by the fluid content of the tumor vessels (7). In addition, Resnick (2) described the multiple channel-like appearance of the high signal intensity on T2-weighted images. The appearance was similar to that of hemangiomas in the soft tissues in a case of tibial hemangioma. The enhancement pattern of intraosseous hemangiomas was reported to be variable, with whole enhancement, peripheral enhancement, or lattice-like enhancement observed (4910).
In reviewing the literature, several hemangiomas involving the epiphyses of the long tubular bones have been reported (Table 1) (3456). Among these cases, three hemangiomas were seen as well-defined osteolytic lesions on radiographs. In the present case, there was no gross bony abnormality in the humeral head. Two of the three cases where the CT findings were reported sh-owed partial cortical breakthrough on CT images. In the present case, CT imaging showed a focal cortical defect, similar to the findings of the above two cases. On MRI, one case showed a multilocular and hemorrhagic lesion with fluid-fluid level, and the other cases showed hypointensity on T1-weighted images, hyperintensity with internal hypointense septa on T2-weighted images, and lattice-like enhancement. In the present case, the lesion showed inhomogeneous enhancement and intervening low signal lines on MRI. In agreement with the histopathological findings, the portion of inhomogeneous enhancement might be related to the multiple dilated vascular channels while the portion of intervening low signal lines might be related to the thickened trabeculae.
In conclusion, we report an unusual case of a hemangioma involving the epiphysis of the humeral head that was seen with inhomogeneous enhancement and intervening low signal lines. These findings were similar to findings of hemangiomas in the vertebral bodies.
Figures and Tables
 | Fig. 1An anteroposterior radiograph of the right shoulder shows no gross abnormalities in the humeral head. |
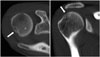 | Fig. 2CT scans show an irregular and lobulating osteolytic lesion with a peripheral sclerotic rim and thickened internal trabeculae (arrow). On coronal reformatted images, a focal cortical defect (arrow) is suggested. |
 | Fig. 3Magnetic resonance images show irregular low signal intensity on T1-weighted images (A, arrow; T1WI; axial plane; TR/TE, 600/20 ms), mixed low and high signal intensities on T2-weighted images (B, arrow; T2WI; coronal plane; TR/TE, 4400/80 ms) and inhomogeneous enhancement on gadolinium-enhanced fat-suppressed T1WI (C, arrow; CE-FS T1WI; axial plane; TR/TE, 670/20 ms). In addition, inner and peripheral low signal lines in this lesion are demonstrated on all MR sequences.CE-FS = contrast-enhanced fat-suppressed, TE = echo time, TR = repetition time
|
 | Fig. 4A photomicrograph (A) of an intraosseous hemangioma reveals numerous vascular channels (arrows) of various sizes and shapes. The irregular architecture of the thickened bony trabeculae (T) is noted (hematoxylin and eosin staining, original magnification, × 40). Immunostaining for factor VIII (B) shows vascular channels of a variety of shapes and sizes (arrows), lined by endothelial cells (polymer method; original magnification, × 200). |
Table 1
Cases of Intraosseous Hemangiomas Involving in the Epiphysis of the Long Tubular Bones

| Authors | Sex/Age | Location | CR | CT | MR | Others |
|---|---|---|---|---|---|---|
| Boumdin et al. (3) | M/22 | Humeral head | A well-defined osteolytic lesion with marginal sclerosis | An osteolytic lesion with coarse trabecular pattern & partial cortical breakthrough | A multilocular and hemorrhagic lesion with fluid-fluid level | Cavernous hemangioma |
| Yamamoto et al. (4) | M/70 | Proximal tibia | A well-defined osteolytic lesion with marginal sclerosis | A well-defined osteolytic lesion with partial cortical breakthrough |
Hypointense lesion on T1WI Hyperintense areas with internal, hypointense septa on T2WI Lattice-like enhancement |
Cavernous hemangioma |
| Mirra (5) | (-) | Tibial epiphysis | (-) | (-) | (-) | Associated with soft tissue hemangioma |
| Pandey and Pandey (6) | F/7 | Greater tuberosity of the humerus | A localized osteolytic lesion | (-) | (-) | (-) |
References
1. Unni KK. Benign vascular tumors. In : Unni KK, Inwards CY, editors. Dahlin's Bone Tumors: General Aspects and Data on 10,165 Cases. Philadelphia: Lippincott Williams & Wilkins;2010. p. 262–271.
2. Resnick D. Tumors of vascular differentiation. In : Resnick D, editor. Diagnosis of Bone and Joint Disorders. Philadelphia: Saunders;1995. p. 3821–3846.
3. Boumdin H, Rachid K, Mahi M, Chaouir S, Benameur M. [Hemangioma of the humerus: value of imaging]. J Radiol. 2002; 83(9 Pt 1):1088–1089.
4. Yamamoto T, Kurosaka M, Mizuno K. Juxta-articular hemangioma of long bone. Skeletal Radiol. 2000; 29:535–537.
5. Mirra JM. Vascular tumors. In : Mirra JM, Picci P, Gold RH, editors. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia: Lea & Febiger;1989. p. 1338–1478.
6. Pandey S, Pandey AK. Osseous haemangiomas. Arch Orthop Trauma Surg. 1981; 99:23–28.
7. Dorfman HD, Czerniak B. Vascular lesions. In : Dorfman HD, Czerniak B, editors. Bone Tumors. St. Louis: Mosby;1998. p. 729–814.
8. Ross JS, Masaryk TJ, Modic MT, Carter JR, Mapstone T, Dengel FH. Vertebral hemangiomas: MR imaging. Radiology. 1987; 165:165–169.
9. Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. Radiographics. 1995; 15:893–917.
10. Matsumoto K, Ishizawa M, Okabe H, Taniguchi I. Hemangioma of bone arising in the ulna: imaging findings with emphasis on MR. Skeletal Radiol. 2000; 29:231–234.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download