Abstract
Adventitial cystic disease (ACD) is a rare, but well-characterized vascular disease. It is most commonly seen in the popliteal artery, but it has also been reported in the venous system. The most commonly involved segment has been the common femoral vein; the disease resulted in luminal compromise and extremity swelling. We report here on a case of percutaneous aspiration and ethanol sclerotherapy for recurrent ACD after surgery of the external iliac vein in a 70-year-old man who presented with a painless swelling of his left leg.
Adventitial cystic disease (ACD) is an uncommon condition that accounts for only 0.1% of all vascular disease (1), and it mainly affects young men with intermittent claudication. It is most commonly seen in the popliteal artery, but it has also been reported in the external iliac, femoral, ulnar and radial arteries. Very few reports of this disease have been described in the venous system such as the common femoral vein, the popliteal vein, the wrist area veins, the lesser saphenous vein and the external iliac vein (2). Surgery has been known to be a standard therapy for this disease. Also there have been reports about less invasive technique such as percutaneous aspiration and angioplasty. However, several recurrences have been reported in these less invasive therapies (3). To the best of our knowledge, there is no report about management of recurrent ACD after surgery with percutaneous drainage and use of absolute ethanol as sclerosis agent. Here we report a case of successful treatment by percutaneous drainage and ethanol sclerotherapy for recurrent ACD of left external iliac vein that was previously treated by cyst excision and patch angioplasty.
A 70-year-old man had 15 days history of swelling in his left leg. Deep vein thrombosis (DVT) was suspected based only on physical examination. Left lower extremity vein Doppler ultrasonography (US) was requested to rule out DVT. There was no definite evidence of DVT on left lower extremity, instead revealed approximately 2.3-cm elongated solid and cystic lesion in left external iliac vessel area with suggestion of lymphadenopathy, and then recommended computed tomography angiography (CTA) for further evaluation. We found cystic lesion in left common femoral vein and contrast filling defects in left deep femoral vein on CTA. Based on US and CTA finding, we concluded that the cystic lesion might be ACD. With a diagnosis of extrinsic compression of the left external iliac vein due to a cystic mass, the patient was scheduled for surgery to remove the cyst and decompress the venous system. On operation, an intraluminal cyst in external iliac vein was found and cyst excision and patch angioplasty was performed. The patient's postoperative course was uneventful and his swelling subsided.
Five months later the patient returned with swelling of his left calf and thigh. Low extremity Doppler ultrasound and CTA examinations revealed a newly developed cystic lesion outside the patch graft in left external iliac vein and patch graft was compressed and the external iliac vein lumen showed near total occlusion (Figs. 1, 2). Also there was newly developed filling defect in left common femoral vein from just distal to patch graft. We concluded this as a recurrent cystic adventitial disease and DVT.
Using a combination of fluoroscopic and ultrasound guidance, an 18-gauge needle was placed percutaneously into the cystic lesion adherent to the left external iliac vein wall. The needle was exchanged for a 4-Fr catheter (Cook, Bloomington, IN, USA) (Fig. 3). Next, gelatinous mucoid substance was aspirated out of the cystic lesion. On cystogram, contrast media leakage was not noted. Mixture of 3 cc of 99.9% ethanol with small amount of contrast media, iodixanol (Visipaque®, GE Healthcare, Princeton, UK), was injected in the cyst. We waited for 20 minutes and then totally aspirated the mixed material out of the lesion without complication.
On prone position, using fluoroscopic guidance, left popliteal vein was punctured and 10 Fr Desilets Hoffman sheath (Cook Incorporated, Bloomington, IN, USA) was inserted. On venogram by 5 Fr catheter (Cook, Bloomington, IN, USA), occlusion in left common femoral vein was noted and also contrast filling defect in proximal portion of femoral vein was noted suggesting venous thrombosis (Fig. 4). We passed through the occluded segment of left common femoral vein using 5-Fr catheter (Cook, Bloomington, IN, USA) and guide wire, then performed left iliac venogram. On left iliac venogram, there was no evidence of stenosis nor occlusion in left proximal external iliac vein and common iliac vein. Venous thrombosis in left proximal proximal portion of femoral vein was aspirated by using 8-Fr catheter (Cook, Bloomington, IN, USA). For the stenosis of left common iliac vein, balloon angioplasty was performed by 10 mm-4 cm balloon catheter (BLUE MAX, Boston Scientific, Maple Grove, MN, USA) (Fig. 5). Residual focal irregular contrast filling defect was noted in left common iliac vein (Fig. 6). But we finished the procedure because of good patency of blood flow without collateral vessels.
The patient revealed no clinical signs or symptoms of recurrence during follow-up of 3 years.
According to report about review of 18 cases of ACD, affected veins were the femoral vein (nine cases), popliteal vein (three cases), lesser saphenous vein (two cases), iliac vein (two cases), greater saphenous vein (one case), and wrist vein (one case) (4). ACD can be difficult to recognize on physical examination. The presenting symptom in most cases of ACD of the vein is extremity edema, as in our patient, although cases of ACD with DVT have been reported (5). Conventional angiography has traditionally been the study of choice for making the diagnosis. Yet this study is invasive and expensive for the evaluation of a peripheral artery, and there are frequently complications. Both enhanced and unenhanced CT scans and CTA have been used successfully in imaging ACD of the vein. If the cyst has concentric appearance, the influenced vein will have an "hourglass" appearance or if it is eccentric, the stenosis shows "scimitar sign". On US, the cyst can have anechoic or hypoechoic mass in the wall of affected vessel (678). Several treatment options have been proposed for cystic adventitial disease. Cystic aspiration has been described, but the cysts may re-occur after this treatment (8). Conventional therapy is surgery, although no established surgical technique has been identified due to the limited numbers of cases reported in the literature. Surgical treatments for lesions on the vein include transluminal fenestration, transadventitial evacuation and segmental resection (9). To provide less invasive treatment, percutaneous aspiration and angioplasty have been investigated and reported. However, several recurrences have also been reported in these therapies. The reasons for recurrence are thought due to incomplete aspiration due to the viscous nature of cyst content (mucin), or recollection of secretions (4). We agree that the first choice of modality for treatment of ACD is surgery. But in case of recurrent ACD, percutaneous aspiration can be considered as a treatment method, because the content of cyst would not as thick as the initial presentation of disease and much easier to completely aspirate.
There is a report about successful percutaneous aspiration and ethanol sclerotherapy for recurrent ACD as in our case (4). This report was based on other reports about ethanol sclerotherapy for cyst wall sclerosis after simple aspiration allowed for benefits for the treatment of hepatic and renal cysts, where safe and long-term resolution has been shown in multiples series.
We also used absolute ethanol for sclerotic agent for the prevention of recurrence, as it damages endothelium of vessel wall and promote sclerosis (4). Also, we chose the absolute ethanol as sclerotic agent, as it is most widely used sclerotic material in out institution. We think that use of absolute ethanol as sclerosis agent will lower the chance of recurrence.
In conclusion, percutaneous aspiration can be considered as a treatment of choice in case of recurrent ACD with use of absolute ethanol as sclerosis agent.
Figures and Tables
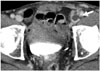 | Fig. 1Axial CT angiography image at inguinal area. Newly developed state of cystic lesion (arrow) outside the patch graft in left external iliac vein. Patch graft is compressed and the external iliac vein lumen shows near total occlusion. |
 | Fig. 2Duplex ultrasound image of left external iliac vein. Anechoic cystic lesion (arrow) outside the patch graft in left external iliac vein. Patch graft is compressed and the left external iliac vein lumen shows near total occlusion. |
 | Fig. 3Cystogram by ultrasonography guided puncture of the cystic lesion at the left external iliac vein. Ethanol sclerotherapy is performed at recurrent adventitial cystic disease (arrow). |
 | Fig. 4Venogram after puncture of left popliteal vein. Contrast filling defect is found at left proximal portion of femoral vein (arrow) with collateral vessels. Also, contrast filling defect at left common femoral vein (double arrows). These findings are compatible with deep vein thrombosis. |
References
1. Wright LB, Matchett WJ, Cruz CP, James CA, Culp WC, Eidt JF, et al. Popliteal artery disease: diagnosis and treatment. Radiographics. 2004; 24:467–479.
2. Lie JT, Jensen PL, Smith RE. Adventitial cystic disease of the lesser saphenous vein. Arch Pathol Lab Med. 1991; 115:946–948.
3. Sieunarine K, Lawrence-Brown MM, Kelsey P. Adventitial cystic disease of the popliteal artery: early recurrence after CT guided percutaneous aspiration. J Cardiovasc Surg (Torino). 1991; 32:702–704.
4. Johnson JM, Kiankhooy A, Bertges DJ, Morris CS. Percutaneous image-guided aspiration and sclerosis of adventitial cystic disease of the femoral vein. Cardiovasc Intervent Radiol. 2009; 32:812–816.
5. Gasparis AP, Wall P, Ricotta JJ. Adventitial cystic disease of the external iliac vein presenting with deep venous thrombosis. A case report. Vasc Endovascular Surg. 2004; 38:273–276.
6. Beregi JP, Djabbari M, Desmoucelle F, Willoteaux S, Wattinne L, Louvegny S. Popliteal vascular disease: evaluation with spiral CT angiography. Radiology. 1997; 203:477–483.
7. Deutsch AL, Hyde J, Miller SM, Diamond CG, Schanche AF. Cystic adventitial degeneration of the popliteal artery: CT demonstration and directed percutaneous therapy. AJR Am J Roentgenol. 1985; 145:117–118.
8. Keo HH, Baumgartner I, Schmidli J, Do DD. Sustained remission 11 years after percutaneous ultrasound-guided aspiration for cystic adventitial degeneration in the popliteal artery. J Endovasc Ther. 2007; 14:264–265.
9. di Marzo L, Peetz DJ Jr, Bewtra C, Schultz RD, Feldhaus RJ, Anthone G. Cystic adventitial degeneration of the femoral artery: is evacuation and cyst excision worthwhile as a definitive therapy. Surgery. 1987; 101:587–593.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download