INTRODUCTION
Scrub typhus causes systemic vasculitis characterized by the destruction of endothelial cells that line small blood vessels and inflammatory lesions caused by infiltrating leukocytes (1). It is a rickettsial disease caused by Orientia tsutsugamushi and is transmitted through chigger bites. Its prevalence is high in East Asia, Korea, and the western Pacific region (1). It involves multiple organs, and is characterized by a fever, headache, myalgia, rash, lymphadenopathy, eschar formation, pneumonia, and meningoencephalitis. Scrub typhus with central nervous system (CNS) involvement presents with various features from aseptic meningitis to meningoencephalitis (2). Cerebrospinal fluid (CSF) analysis generally shows pleocytosis, a normal level of glucose, and a mild increase in the protein level (1). The early diagnosis of scrub typhus with CNS involvement is important, as it can alter the patients' prognoses and reduce mortality rates. Scrub typhus with CNS involvement is not rare and has been reported in several cases. However, to the best of our knowledge, scrub typhus encephalitis with extensive white matter involvement and subependymal enhancement are rarely described findings in the previous literature.
CASE REPORT
Case 1
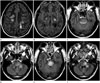
A 57-year-old man was admitted to our hospital for general weakness, gait disturbance, and mental change. He had visited a family member's grave 1 month previously. For 3 days before admission, the patient experienced a febrile sensation and skin rash. He had no previous history of medical diseases, such as diabetes mellitus, hypertension, or tuberculosis. Physical examination showed a temperature of 37.4℃, blood pressure of 120/70 mm Hg, and pulse rate of 70/min. Eschars were noted over the upper portion of his left arm and back. A neurologic examination indicated that his consciousness ranged from a stupor to a semicomatose state. He did not show motor responses and had a sluggish light reflex. He did not have cranial nerve palsy. Results of the routine hematology test were normal, except for elevated fibrin degradation product (5.0 µg/mL) and D-dimer levels (1.57 µg/mL fibrinogen equivalent units). The liver function test showed an albumin level of 3.4 g/dL (range: 3.8-5.3 g/dL), total bilirubin level of 0.6 mg/dL (range: 0.2-1.0 mg/dL), alkaline phosphatase level of 362 U/L (range: 104-338 U/L), aspartate aminotransferase (AST) level of 812 U/L (range: 10-33 U/L), and alanine aminotransferase (ALT) level of 1043 U/L (range: 4-50 U/L). The C-reactive protein (CRP) level was 3.76 mg/dL (-0.5 mg/dL), and the erythrocyte sedimentation rate was 24 mm/h (range: 0-20 mm/h). Serologic tests yielded negative results for the hepatitis B surface antigen, human immunodeficiency virus, Hantan virus, Epstein-Barr virus, and cytomegalovirus. Polymerase chain reaction test results for the Epstein-Barr virus, cytomegalovirus, and tuberculosis were negative. CSF analysis showed a white blood cell count of 220/mm3 (lymphocytes 30%, polymorphonucleocytes 70%), glucose level of 66 mg/dL (blood glucose, 133 mg/dL), and protein level of 138.5 mg/dL (range: 11-45 mg/dL). The CSF sample tested positive for the tsutsugamushi antibody [immunoglobulin (Ig)-G, 1:160] and serum sample (IgG, 1:10240). Chest computed tomography showed patchy consolidations in the lower lobes of both lungs. On admission magnetic resonance images (MRIs), T2-weighted images (T2WIs), and fluid-attenuated inversion recovery images (FLAIRs) demonstrated multifocal, hyperintense lesions involving the cerebral white matter of both the right and left sides, thalamus, brainstem, left middle cerebellar peduncle, and both cerebellar hemispheres (Fig. 1). These lesions did not show contrast enhancement on contrast-enhanced T1-weighted images. On a follow-up MRI, obtained 5 days after admission, the extent of multiple areas of T2 hyperintense cerebral white matter lesions on both the right and left sides were slightly increased, with no significant interval change in the other sites. After treatment with doxycycline for 2 weeks, his consciousness improved to an alert state. However, his motor functions were still impaired in the left upper (grade 2/5), left lower (grade 3/5), right upper (grade 1/5), and right lower (grade 1/5) extremities. A follow-up MRI, acquired 2 weeks after admission, previously noted that the number of multifocal T2 hyperintense lesions had slightly decreased in the cerebral white matter on both sides and increased in the brainstem (Fig. 1). However, no significant interval changes were seen in the other lesion sites. He was discharged to a local hospital for rehabilitative therapy.
Case 2
A 71-year-old woman was admitted to our hospital for general weakness. The patient had visited the countryside to pick persimmons 4 days previously. Three days before admission, she had visited a local hospital because of fever and general weakness. Her symptoms had not improved, and she presented with irritability on admission. She had a history of osteoporosis and hyperlipidemia, and was taking cholesterol-lowering medication. Physical examination showed a temperature of 36.5℃, blood pressure of 130/80 mm Hg, and pulse rate of 80/min. The patient did not have eschars, but she presented with ecchymosis and pain in both arms. Cranial nerve function was essentially normal. The patient did not present with abnormal motor function. Results of the routine hematology test were normal. The liver function test showed an albumin level of 4.0 g/dL (range: 3.8-5.3), total bilirubin level of 0.7 mg/dL (range: 0.2-1.0 mg/dL), alkaline phosphatase level of 240 U/L (range: 104-338 U/L), AST level of 254 U/L (range: 10-33 U/L), and ALT level of 52 U/L (range: 4-50 U/L). The creatine phosphokinase level was 11875 U/L (range: 38-176 U/L), and the CRP level was 0.23 mg/dL (-0.5 mg/dL). Serologic tests yielded negative results for the Hantan virus antibody, influenza A and B viral antigens, Cryptococcus antigen, varicella zoster virus, and human T-lymphotropic virus I/II. Polymerase chain reaction test results for the varicella zoster virus, herpes simplex virus, and tuberculosis were negative. The CSF and serum samples tested positive for the tsutsugamushi antibody (IgG, ≥ 1:160 and IgG, 1:640, respectively). Chest radiography showed no significant abnormality in both lungs. She was diagnosed with rhabdomyolysis and scrub typhus. After discontinuing the cholesterol-lowering medication, doxycycline was administered on the day following admission. Levels of the liver function enzymes and creatine phosphokinase improved, and the ecchymosis of both arms improved. However, her consciousness suddenly altered. CSF analysis showed a white blood cell count of 25 mm3 (lymphocytes 90%, polymorphonucleocytes 10%), glucose level of 46 mg/dL (blood glucose, 154 mg/dL), and protein level of 115.4 mg/dL (range: 11-45 mg/dL). Contrast-enhanced T1-weighted images showed focal parenchymal enhancement involving the right gyrus rectus and subtle subependymal enhancement along both lateral ventricles (Fig. 2). These lesions did not show a signal change on T2WIs and FLAIRs. We initiated treatment with a combination of doxycycline and rifampin. However, a follow-up MRI acquired 3 days later showed more prominent subependymal enhancement along both lateral ventricles. Another follow-up MRI, obtained 10 days later, after persistent medical therapy, showed that the subependymal enhancement along both the lateral ventricles had disappeared and new multifocal T2 hyperintense lesions appeared in both the basal ganglia and right frontal lobe (Fig. 2). The patient's mental status improved slightly (to a stupor) and she was transferred to another local hospital.
DISCUSSION
Scrub typhus is commonly acquired through agricultural and recreational activities in the woods or mountains in endemic areas (12). It frequently occurs during spring and summer in temperate areas and throughout the year in tropical regions (3). Typhus is derived from the Greek word tuphos, which means stupor (4). The severity of the clinical manifestations ranges from mild to severe or fatal (5).
Scrub typhus can involve both the central and peripheral nervous systems. Scrub typhus with CNS involvement has diverse manifestations, such as meningoencephalitis, infarction, cerebellitis, myelitis, intracranial hemorrhage, demyelination, subdural hematoma, and typhus nodules (46). A few previous studies have reported focal neurologic signs and abnormal neurologic findings in patients with scrub typhus, but the cases in this study showed mental deterioration and severe neurologic deficit (7). The mortality rate of scrub typhus with CNS involvement is higher than that for other CNS infections, and reaches up to 25% (1). Although scrub typhus can be associated with significant morbidity, it generally resolves after treatment with doxycycline for an appropriate duration (8).
Scrub typhus is usually limited to the gray matter because, pathologically, it involves small vessels throughout the body (79). Thus, scrub typhus rarely involves the white matter, and only a few reports have described cases of scrub typhus involving the white matter (37). According to a previous case report, the white matter can be destroyed because of a blood-brain barrier breakdown, microinfarction, and edema (7). The first patient in this study showed extensive white matter involvement, which mimicked radiologic findings of acute disseminated encephalomyelitis. The second patient presented with subependymal enhancement along both lateral ventricles. To the best of our knowledge, subependymal enhancement associated with scrub typhus has not been reported in previous case reports. Considering the CSF findings, we presumed that the subependymal enhancement is associated with ventriculitis.
Pathologic findings of scrub typhus with CNS involvement include diffuse or focal histiocytes, lymphocytes and plasma cell infiltration of the leptomeninges, typhus nodules (i.e., clusters of microglial cells), and brain hemorrhage (610). The diagnosis of scrub typhus is usually dependent on a history of exposure, clinical features including eschars, and serological test results. The patients in this study showed typical findings, such as CSF pleocytosis, and both patients had an elevated CSF protein level (> 60 mg). Liver enzyme levels are usually elevated in scrub typhus, and the patients showed elevated liver enzyme levels. However, a radiologic diagnosis based on MRI findings is not easy because scrub typhus does not present typical features. In the cases of this study, the diagnosis was apparent because the first patient presented with eschars, and both patients had a history of agricultural activity and positive serologic test results.
Scrub typhus responds well to antibiotics, and the treatment of scrub typhus should be started as soon as possible after diagnosis. The patients in this study did not show complete recovery, but their symptoms resolved with treatment. A previous study reported that CSF results of scrub typhus meningitis normalized within a shorter time than other types of meningitis (7). The patients' follow-up CSF results normalized after 5 and 9 days, respectively.
CNS involvement is not rare in scrub typhus; thus, clinicians should carefully consider a patient's complaints of neurologic symptoms, including headache, dizziness, and drowsiness. Recognizing atypical radiologic findings of scrub typhus may be helpful in the early diagnosis of scrub typhus with CNS involvement, which may alter the prognoses of patients.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download