Abstract
Herein we report a rare case of an intracortical chondroma with the histologic appearance of an enchondroma but located within the cortical bone.
Intracortical chondroma is a very rare benign cartilaginous tumor characteristically located in the cortex of long bones. Comprised of mature cartilage, it is rarely reported in literatures (1, 2, 3). Herein we report a rare case of intracortical chondroma in a 49-year-old woman with histologic appearance of enchondroma but located within the cortical bone. We performed literature review with emphasis on imaging findings.
A 49-year-old woman presented a focal hot uptake lesion in the right distal femur on whole body radioisotope (RI) bone scan taken at postoperative follow-up due to breast cancer (Fig. 1). There was no uptake in the same area of the right distal femur on whole body RI bone scan performed one year ago. Plain radiographs of the right knee showed a 1 cm sized well-circumscribed focal round osteolytic lesion located eccentrically in the marrow space of the distal femur with a sclerotic rim and intralesional calcification (Fig. 2). Magnetic resonance imaging (MRI) showed an intracortical tumor with a strong hyperintense signal on short tau inversion recovery pulse sequence and a hyperintense signal on T2-weighted image as well as rim contrast enhancement and internal focus on contrast enhanced T1-weighted image. The lesion was confined to the cortical bone. There was no extension into medullary canal. These findings were suggestive of a nonaggressive cartilaginous lesion (Fig. 3). Differential diagnosis of the lesion was osteoid osteoma, intracortical osteosarcoma, low-grade chondrosarcoma, or intracortical chondroma. The mass was excised en bloc and pathologically diagnosed as chondroma (Fig. 4). After the surgery, she was discharged without further complications.
According to reported cases in English journals, intracortical chondroma is extremely rare. Abdelwahab et al. (1) first described intracortical chondroma of the left femur in 1990. To the best of our knowledge; only 8 cases have been published in the literature (1, 2, 3, 4, 5, 6). The age of patients ranged from 2 to 58 years. In most cases, long bones of the lower extremities located in the diaphysis were affected. Most patients presented asymptomatic lesion. In contrast, periosteal chondromas presented with symptomatic lesion such as painful lesions. It was reported that the stretching of pain receptors in the periostium could cause the pain symptom (4).
Plain radiography of intracortical chondromas revealed geographic lysis. Additionally, radiographs showed intralesional calcification (5). On bone scintigraphy, the lesions showed mild hot uptakes in all cases. Computed tomography (CT) showed intact periosteal/cortical margins in all cases. The attenuation value of non-mineralized regions was analogous to a muscle. On MR imaging, the lesions revealed lobular contours, isointense signals to a muscle on T1-weighted images and hyperintense signals on T2-weighted images (1, 5). Gadolinium-enhanced MR imaging showed mild septal and peripheral enhancement appearances (7). The prognosis of all cases was great without associated mortality compared to those of other chondromas.
Enormous disease entities include tumorous or tumor-like lesions involving bony cortex. Differential diagnosis for intracortical lesions includes osteoid osteoma, non-ossifying fibroma, intracortical fibrous dysplasia, intracortical abscess, osteofibrous dysplasia, intracortical angioma, intracortical chondroblastoma (8), intracortical osteosarcoma (9), intracortical chondromyxoid fibroma (10), and intracortical chondroma (1, 2). Osteoid osteoma can occur as intracortical lesion, with 2 in 3 changes involving extremity bones, especially proximal and distal femur and proximal tibia. CT, MRI, and RI bone scan may be needed to prove the diagnosis and show the nidus. It is important to identify the central calcifications encircled by oval translucency for radiological diagnosis of osteoid osteoma. Intracortical osteoid osteoma shows hyperdense sclerosis around the nidus. Subperiosteal type osteoid osteoma produces periosteal reaction. On RI bone scan, osteoid osteoma may demonstrate focal hot uptake. In our case, there was an intralesional calcification mimicking the nidus. However, there was no dense sclerosis around the calcification or periosteal reaction. There was no hot uptake on RI bone scan either.
Although only a few cases of intracortical osteosarcoma were reported, most of these reported cases had benign-looking intracortical osteolytic lesion with no or subtle periosteal reaction (9). It may be necessary to distinguish intracortical osteosarcoma from osteoid osteoma or osteoblastoma depending on its size. It is possible to distinguish it from those disease entities depending on its local aggressiveness and cellular atypia. Histopathologically,
there is usually rich bone or osteoid formation in intracortical osteosarcoma. Creation of cartilage is not usual, but it may help distinguish the intracortical osteosarcoma from osteoid osteoma or osteoblastoma. On MRI, adjacent bone marrow and soft tissue edema has rarely been reported (9).
Other fibrous cortical bone diseases such as intracortical fibrous dysplasia and nonossifying fibroma were not considered as differential diagnosis because they may be often hypointense signal on conventional T1-, T2-weighted MR images. The main histologic differential diagnosis of intracortical chondroma is chondrosarcoma. Low-grade chondrosarcoma may show similar cytological features with those of enchondroma. The most important histologic feature for discriminating between them is a growth pattern. Chondrosarcomas typically infiltrate bone marrow and Haversian canals. However, such features do not exist in chondromas (2). It is difficult to clearly find an invasive growth pattern using small amounts of biopsy specimen. Therefore, the clinical and radiologic correlation is very important for their accurate diagnosis (2).
In conclusion, intracortical chondroma is a very rare benign cartilagenous neoplasm. Imaging findings strongly suggest that intracortical chondroma have intracortical location, lobular contours, elongated shape, and chondroid matrix. Plain radiographs and pathology may mimic a more aggressive lesion due to obvious destruction to bony cortex. However, CT and MR showing intact bony cortex would indicate benign entity of the lesion.
Figures and Tables
Fig. 1
The whole body radioisotope bone scan shows a small focal hot uptake in the right distal femur (arrow).

Fig. 2
Anterior-posterior (A) and lateral (B) radiographs of the right knee show a focal lytic lesion with sclerotic rim and intralesional calcification in the right distal femur (arrows).
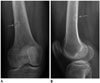
Fig. 3
The MRI shows an intracortical lesion with bright signal intensity on short tau inversion recovery (A) and high signal intensity and contrast enhancement of rim and internal focus on T2- (B) and contrast enhanced fat saturated T1-weighted (C) images in the right distal femur (arrows), suggestive of a cartilaginous lesion.

Fig. 4
The histopathology of the excised lesion from the right distal femur.
A. Low magnification hematoxylin and eosin (H&E, × 40) staining demonstrates bland hyaline cartilage matrix and a benign interface with surrounding cortical bone.
B. Higher magnification H&E staining (× 200) highlights the lone chondrocytes in the lacunae and the lack of nuclear atypia.

References
1. Abdelwahab IF, Hermann G, Lewis MM, Klein MJ. Case report 588: Intracortical chondroma of the left femur. Skeletal Radiol. 1990; 19:59–61.
2. Rudman DP, Damron TA, Vermont A, Mathur S. Intracortical chondroma. Skeletal Radiol. 1998; 27:581–583.
3. Ramnath RR, Rosenthal DI, Cates J, Gebhardt M, Quinn RH. Intracortical chondroma simulating osteoid osteoma treated by radiofrequency. Skeletal Radiol. 2002; 31:597–602.
4. Jones KB, Buckwalter JA, Frassica FJ, McCarthy EF. Intracortical chondroma: a report of two cases. Skeletal Radiol. 2006; 35:298–301.
5. Lui PC, Lau PP, Fan YS, Choi ST, Mak KH, Tam KF, et al. Intracortical chondroma in a 7-year-old boy and literature review. Pathology. 2006; 38:186–189.
6. Choi E, Wert M, Guerrieri C, Tucci J. A pathologic fracture of an intracortical chondroma masking as an osteoid osteoma. Orthopedics. 2010; 33:845.
7. Ruble C, Murphey MD, Fanburg-Smith J, Tyszko S, Zbojniewicz A, Franklin J. Imaging of intracortical chondroma. Special scientific paper session ISS 2009 Program Tuesday, September 1, 2009. Skeletal Radiol. 2009; 38:937–945.
8. Ishida T, Goto T, Motoi N, Mukai K. Intracortical chondroblastoma mimicking intra-articular osteoid osteoma. Skeletal Radiol. 2002; 31:603–607.
9. Hermann G, Klein MJ, Springfield D, Abdelwahab IF, Dan SJ. Intracortical osteosarcoma; two-year delay in diagnosis. Skeletal Radiol. 2002; 31:592–596.
10. Fujiwara S, Nakamura I, Goto T, Motoi T, Yokokura S, Nakamura K. Intracortical chondromyxoid fibroma of humerus. Skeletal Radiol. 2003; 32:156–160.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download