Abstract
Encephaloceles are generally regarded as midline abnormalities. A 50-year-old man presented with a parietal intradiploic encephalocele manifesting as intermittent headache for the past 6 months. Computed tomography (CT) showed bone destruction associated with a left parietal lesion. Magnetic resonance imaging (MRI) demonstrated brain herniation within the intradiploic space. Cerebral angiographic imaging showed a normal cerebral vessel pattern within the herniated brain lesion. In this case, surgical treatment may not be necessary in the absence of concurrent symptoms and neurologic deficit. We report the CT, MRI, and angiographic findings of an extremely rare case of parietal intradiploic encephalocele in adulthood.
Encephaloceles consist of herniated cerebral tissue through the skull or dural defect (1). Encephaloceles may develop spontaneously as congenital maldevelopments or may occur subsequent to acquired processes, such as infection, trauma, neopla-sms, and surgical procedures. The incidence of this malformat-ion has been estimated at one in every 3000 to 10000 live births (2). These lesions are a rare complication of skull fractures and rarely occur in adults. They can be difficult to distinguish from congenital encephaloceles in patients with no history of head trauma.
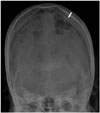
We report a rare case of parietal intradiploic encephalocele incidentally found on computed tomography (CT) and magnetic resonance imaging (MRI). Cerebral angiographic imaging was useful to define the abnormal vascular lesion, such as arteriovenous malformation, arteriovenous fistula, and hyper- or hypo-vascular tumor.
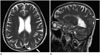
A previously healthy 50-year-old man presented with intermittent headache for the past 6 months. He had no history of head trauma and surgery. The patient was alert and had normal vital signs. The neurological and general physical examinations were normal. Results of routine laboratory blood tests including C-reactive protein and erythrocyte sedimentation rate were within their normal ranges. Tumor markers were negative. Skull radiography showed osteolytic changes involving the left parietal bone (Fig. 1). CT demonstrated a defect of the inner table, widened diploic space with outer table bony erosion, and thinning of the left parietal parasagittal bone (Fig. 2). MRI revealed a lesion in the parietal parasagittal intradiploic space continuous with the left parietal lobe appearing isointense to the normal br-ain on the axial T2-weighted image (Fig. 3A). Sagittal T2-wei-ghted MRI showed a defect in the left parietal bone, which contained cerebrospinal fluid and herniated cerebral tissue (Fig. 3B). We performed transfemoral cerebral angiography to identify vascular abnormalities. A baseline control angiogram of the left internal carotid artery showed a normal cerebral vessel pattern for the herniated brain in the left parietal bony defect area and no vascular abnormalities, such as arteriovenous malformation, arterioveous fistula, hemangioma, and hyper- or hypo-vascular tumor (Fig. 4). After the headache was resolved symptomatically with medical therapy, the patient was discharged.
A cephalocele is defined as a protrusion of intracranial contents through a defect in the skull or dura. The herniating neural tissue may include meninges, brain parenchyma, ventricles, and vascular structures. Encephaloceles consist of herniated cerebral tissue through the skull or dural defect, and are generally regarded as midline cerebral abnormalities (3).
During the 8th week of development, the two parietal bones undergo membranous ossification from two primary centers for each bone. At 4 months, the fusion between these centers is com-plete. At birth, the parietal bones are unilaminar and are separated by the sagittal suture. At the age of 4 years, differentiation between the inner and outer tables is evident, and the ossification of the sagittal suture begins at the same time for the two layers. A complete fusion takes place by the age of 20 years. Defects occurring as the sagittal suture closes allow the herniation of the brain, but they involve both tables (4). Therefore, these spontaneous lesions usually occur at the site of a cranial suture, and most of these lesions represent primary or secondary midline closure defects of the neural tube. Parietal cephaloceles are very rare (10% of cephaloceles), and if they are congenital, they are usually associated with anomalies, such as corpus callosum agenesis and Dandy-Walker malformation (5).
Intradiploic encephaloceles are also very rare, with only a few cases having been reported with diagnosis based on surgical biopsy (1, 3). Paters et al. (5) and Dobrin et al. (6) reported a global defect of both inner and outer tables in all cases of congenital parietal encephaloceles. This unusual lesion resembles the mechanism of a growing skull fracture (6). Although the majority of reported intradiploic encephaloceles are of traumatic origin, several reports found no certain cause for these lesions. In this lesion, increased intracranial pressure results in further herniation of the involved site, which can cause symptoms that include headache, seizure, motor weakness, and aphasia (7). The differential diagnosis includes head trauma, multiple myelomas, dermoids, epidermoids, metastatic bone tumor, arachnoid cyst, eosinophilic granuloma, and brain tumor (3, 8). CT, MRI, and cerebral angiography have been used in the evaluation of encephaloceles. Surgery is indicated for both diagnosis and treatment of symptomatic encephaloceles (3). However, the surgical treatment for asymptomatic incidental lesions remains controversial. In the present case, we considered that maybe the lesion was an acquired lesion following an insignificant head trauma in early childhood because congenital encephaloceles usually occur in the midline and extend through both the inner and outer tables, and there were no other malformations (5).
In conclusion, we report a rare case of intradiploic encephalocele in the left parietal lobe incidentally discovered on CT and MRI. Cerebral angiography was useful in the differential diagnosis of an abnormal vascular lesion.
Figures and Tables
Fig. 2
Coronal image of bone window CT shows a defect of the inner table, widened diploic space (black arrow). There is marked thinning and erosion of the outer table of the left parietal parasagittal bone (white arrow).
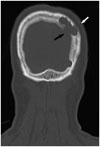
Fig. 3
MRI shows a lesion in the parietal parasagittal intradiploic space continuous with the left parietal lobe appearing isointense with the normal brain on axial T2-weighted (A) image. Sagittal T2-weighted MRI shows a defect in the left parietal bone, which contains cerebrospinal fluid and herniated cerebral tissue (white arrow) (B).
References
1. Kosnik EJ, Meagher JN, Quenemoen LR. Parietal intradiploic encephalocele. Case report. J Neurosurg. 1976; 44:617–661.
2. Mealey J Jr, Dzenitis AJ, Hockey AA. The prognosis of encephaloceles. J Neurosurg. 1970; 32:209–218.
3. Tsuboi Y, Hayashi N, Noguchi K, Kurimoto M, Nagai S, Endo S. Parietal intradiploic encephalocele--case report. Neurol Med Chir (Tokyo). 2007; 47:240–224.
4. Sadler TW. Langman's medical embryology. 10th ed. Baltimore: Lippincott Williams & Wilkins;2006. p. 126–143. p. 286–317.
5. Peters J, Raab P, Marquardt G, Zanella FE. Intradiploic meningoencephalocele. Eur Radiol. 2002; 12:Suppl 3. S25–S27.
6. Dobrin N, Bălinişteanu M, Costăchescu B, Tudorache C, Chiriac A, Poeată I. Acquired parietal intradiploic encephalocele. Case report and review of the literature. Rom S Neurosurg. 2011; 18.
7. Loumiotis I, Jones L, Diehn F, Lanzino G. Symptomatic left intradiploic encephalocele. Neurology. 2010; 75:1027.
8. Kumar R, Chandra SP, Sharma BS. Giant intradiploic pseudomeningocele of occipital bone. J Neurosurg Pediatr. 2012; 9:82–85.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download