Abstract
Cavernous sinus thrombophlebitis (CST) is a rare and life-threatening disease without prompt diagnosis and treatment. Two cases of fulminant superior ophthalmic vein (SOV) and CST caused by maxillary periodontitis and sphenoid sinusitis are described. A 65-year-old woman presented with right proptosis, headache, and fever. A 74-year-old woman presented with left periorbital swelling. In both patients, MRI with gadolinium showed expansion of the bilateral cavernous sinus and diffuse dilatation of the SOV with non-enhancement of central thrombus, which indicated CST. The condition was complicated by brain abscess, meningitis, and ischemic stroke. These conditions were improved by antibiotic treatment, but one patient underwent exenteration of the orbit due to orbital rupture during hospitalization.
Cavernous sinus thrombophlebitis (CST) is a rare but potentially lethal condition associated with significant morbidity and mortality. The mortality and morbidity associated with CST has remarkably decreased after improvement in antibiotic treatment, but it is still a lethal disease without prompt assessment and treatment. The presence of extensive valveless communication among veins of the orbit, face, and neck, render the cavernous sinuses (CSs) vulnerable to infection. The most common primary trigger of CST is paranasal sinusitis, whereas odontogenic or otogenic infections are the less common causes (1). Bidirectional and bilateral spread of a CS infection is usual (2), and this may extend into nearby structures. We report two cases of fulminant superior ophthalmic vein (SOV) and CS infections showing intracranial extension.
A 65-year-old female was hospitalized after a 2-week history of right-sided proptosis, headache, and fever. The patient was suffering from toothache since several weeks. Physical examination revealed right-eye proptosis with limitation of eyeball movement. The leukocyte count was 15600/mm3 and the C-reactive protein level was 21.3 mg/dL. Orthopantomography revealed a periapical abscess of the left secondary maxillary molar.
MR imaging was performed. The contrast-enhanced three-dimensional fast spoiled gradient-echo images showed multifocal, irregular filling defects within an expanded, enhanced CS (Fig. 1A). The left SOV was dilated in the absence of enhancement (Fig. 1B). Both the CS and the left SOV exhibited restricted diffusion (Fig. 1C). We suspected that the periapical abscess was the primary source of infection of the SOV and CST, and commenced parenteral broad-spectrum antibiotics after tooth extraction. Parvimonas micra was identified on blood culture. Follow-up contrast-enhanced T1-weighted spin echo images [repetition time (TR)/echo time (TE), 600/9.3] showed that the CST was controlled but brain abscesses developed on the left anterior temporal convexity at 7 days after admission (Fig. 1D). The patient continued to take antibiotics for 1 month and was then discharged.
A 74-year-old female presented with periorbital swelling and purulent discharge from the left eye. She was suffering from diabetes mellitus since 20 years. Her body temperature was 37.2℃ and periorbital edema was evident. The leukocyte count was 18880/mm3 and the C-reactive protein level was 16.6 mg/dL.
A post-contrast enhanced CT scan revealed left-sided proptosis, a gas-containing abscess in the preseptal region, and left sphenoid sinusitis (Fig. 2A). MR imaging was performed. The contrast-enhanced T1-weighted fat-suppressed spin-echo image (TR/TE, 816.6/9) showed diffuse dilatation of the left SOV and a non-enhanced central thrombus (Fig. 2B). Multiple abscesses were evident in the preseptal region and the intraconal space. CST was noted, along with thick enhancement of the dura along the left frontotemporal cerebral convexity.
Antibiotic therapy was commenced and patient underwent exenteration of the left orbit due to orbital rupture on the third hospital day. Corneal culture yielded Actinomyces. Aspergillus was cultured from a fungal ball from the left sphenoid sinus, and from the specimen obtained after exenteration. Therefore, antifungal agents were added. However, patient experienced a sudden episode of dysarthria and right-sided weakness at 15 days after admission. Multifocal acute infarctions in the left basal ganglia and periventricular white matter were identified on diffusion-weighted image (Fig. 2C). Combination treatment with antiplatelet and antimicrobial agents was continued for 6 weeks, and the patient recovered and was discharged.
The CSs are heavily trabeculated venous sinuses located along the sides of the sella turcica, extending from the anterior superior orbital fissure posteriorly to the petrous portion of the temporal bone. The CSs have extensive vascular connections that are valveless, rendering the CSs prone to septic thrombosis after infection (2). Paranasal sinusitis has become the most frequent cause because complicated facial infections have been effectively reduced by antibiotic treatment (3, 4). Two-thirds of cases in the antibiotic-era develop chronic residual neurological deficits including ocular palsy, blindness, hemiparesis, or pituitary insufficiency (4). Because of the risk of such poor outcomes, if CST is clinically suspected, it is imperative that prompt treatment should be given and careful evaluation including radiographic studies should be considered.
When paranasal sinusitis causes CST, as in one of our patients, sphenoethmoid sinusitis is the common cause. This occurs, first, via direct spread of an infection through communicating veins, facilitated by osteomyelitis of the intervening diploic bone or by mucosal breach caused by bony defects (5). Second, indirect spread occurs via the ophthalmic veins after penetration of the lamina papyracea, as in our cases. The latter route of infection is more common (6). Recently, oral and dental infections have been described as uncommon causes of CST. Infections can extend from the maxillary molar to enter the orbit through the inferior orbital fissure, eventually spreading to the CSs (1).
The organism most commonly isolated from CST patients is Staphylococcus aureus (69%) (1). Also, Rhinocerebral mucormycosis and Aspergillus can cause CST in immunocompromised and diabetic patients (7). Mixed infections involving beta-hemolytic streptococci, other streptococci, and anaerobes, are common in patients with oral and dental infections (1). Actinomycosis rarely extends to the CSs, either direct extension from the ear or sinuses or hematogenous spread may play a role (8).
The most common presentations of CST patients include fever, proptosis, and external ophthalmoplegia triggered by secondary dysfunction of cranial nerves III, IV, and VI (4). Moreover, intracranial extension of infections can develop, triggering pituitary insufficiency, meningitis, cortical vein thrombophlebitis with subsequent hemorrhagic infarction, subdural empyema, or development of brain abscesses (3).
CT and MRI are the primary imaging modalities to confirm the suspected origin of the infectious process and to promptly detect fatal intracranial complications of CST. Multiple filling defects within the expansive contours of enhanced CSs, caused by a thrombus, are direct signs. Filling defects in CST tend to be larger in size and show non-fat density compared with intracavernous fat deposits. Also, the thrombus is irregular in shape, whereas neural structures in CSs are either longitudinal or round to oval and confined to the lateral wall (9).
Indirect signs are related to concomitant venous obstruction, including dilatation of the SOVs, exophthalmos, and abnormal enhancement of the dura along the lateral margins of the CSs (7, 8). SOV thrombophlebitis is one of the well-known imaging findings of CST, which was present in all of our cases. Brain abscesses developed on the left anterior temporal convexity in the first case. According to Mahapatra (10), if CST is complicated by cerebral abscesses, the common locations of such abscesses are the frontal and temporal lobes.
Management of CST patients includes prompt and aggressive administration of parenteral antibiotics targeting the most common pathogens associated with primary infection, and such a therapy should be maintained for at least 2 weeks after clinical resolution (1). Surgical treatment is reserved for patients with primary sinusitis, dental infection, or complicating brain or orbital abscesses. The use of corticosteroids to treat cranial nerve dysfunction has been reported (4), and adjuvant anticoagulation to prevent thrombus propagation can be helpful (1).
In conclusion, although CST has become a rare disease, it remains potentially lethal, triggering life-threatening complications, long-term sequelae, and significant morbidity. Rapid establishment of the diagnosis of CST using contrast-enhanced CT scans and MR studies with commencement of prompt medical and surgical treatment are crucial.
Figures and Tables
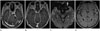 | Fig. 1A 65-year-old female presented with 2-week history of right-sided proptosis, headache, and fever.
A. Axial contrast-enhanced three-dimensional fast spoiled gradient-echo (3D FSPGR) image reveals multifocal, irregular filling defects within an expanded, enhanced cavernous sinus.
B. Axial contrast-enhanced 3D FSPGR image shows linear filling defect in dilated left superior ophthalmic vein (SOV).
C. The thrombosed left SOV exhibits a high signal intensity on diffusion-weighted imaging.
D. Axial contrast-enhanced T1-weighted spin echo images (repetition time/echo time, 600/9.3 msec) shows brain abscesses on the left anterior temporal convexity.
|
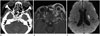 | Fig. 2A 74-year-old female presented with periorbital swelling and purulent discharge from left eye.
A. Axial contrast-enhanced computed tomographic scan reveals left-sided proptosis, a gas-containing abscess in the left preseptal region. The left sphenoid sinus exhibits mucosal thickening.
B. Axial contrast-enhanced T1-weighted fat-suppressed spin-echo image (repetition time/echo time, 816.6/9 msec) reveals a dilated, non-enhanced, left superior ophthalmic vein and rim-enhanced abscesses in the preseptal region and intraconal space. Thick enhancement of the dura along the left frontotemporal cerebral convexity is seen.
C. Follow-up diffusion-weighted imaging after orbital exenteration reveals ischemic infarctions in the left basal ganglia and periventricular white matter.
|
References
1. Bhatia K, Jones NS. Septic cavernous sinus thrombosis secondary to sinusitis: are anticoagulants indicated? A review of the literature. J Laryngol Otol. 2002; 116:667–676.
2. Osborn AG. Osborn's brain: Imaging, Pathology, and Anatomy. Philadelphia: Lippincott Williams & Wilkins;2012. p. 217–218.
3. DiNubile MJ. Septic thrombosis of the cavernous sinuses. Arch Neurol. 1988; 45:567–572.
4. Southwick FS, Richardson EP Jr, Swartz MN. Septic thrombosis of the dural venous sinuses. Medicine (Baltimore). 1986; 65:82–106.
5. Dolan RW, Chowdhury K. Diagnosis and treatment of intracranial complications of paranasal sinus infections. J Oral Maxillofac Surg. 1995; 53:1080–1087.
6. Gallagher RM, Gross CW, Phillips CD. Suppurative intracranial complications of sinusitis. Laryngoscope. 1998; 108(11 Pt 1):1635–1642.
7. Lee JH, Lee HK, Park JK, Choi CG, Suh DC. Cavernous sinus syndrome: clinical features and differential diagnosis with MR imaging. AJR Am J Roentgenol. 2003; 181:583–590.
8. Razek AA, Castillo M. Imaging lesions of the cavernous sinus. AJNR Am J Neuroradiol. 2009; 30:444–452.
9. Schuknecht B, Simmen D, Yüksel C, Valavanis A. Tributary venosinus occlusion and septic cavernous sinus thrombosis: CT and MR findings. AJNR Am J Neuroradiol. 1998; 19:617–626.
10. Mahapatra AK. Brain abscess--an unusual complication of cavernous sinus thrombosis. A case report. Clin Neurol Neurosurg. 1988; 90:241–243.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download