Abstract
Purpose
To analyze hip morphometry of femoroacetabular impingement (FAI) pattern in patients with ankylosing spondylitis (AS) and correlate them with sacroiliitis grades.
Materials and Methods
384 patients with AS were analyzed regarding demographics, radiologic signs of FAI for hip involvement, and sacroiliitis grades. FAI was classified into 3 types according to alpha angle, lateral center-edge angle and pistol grip deformity. Sacroiliitis was graded according to the New York criteria. Prevalence of FAI morphometry types was determined and evaluated for association with sacroiliitis grades. Statistical analysis regarding numerical variables, including age, sacroiliitis score using t-test, sacroiliitis score in three groups using Kruskal-Wallis test and Mann-Whitney U-test, corrected by Bonferroni methods for post hoc analysis was done.
Results
Among 384 patients, 141 (36.7%) had FAI morphometry. Male predominance was found in group with FAI pattern involvement (87.2%) (p = 0.000). Pincer type (20.6%) was the most common. Hip involvement group also showed greater sacroiliitis score (2.49 vs. 1.75, p = 0.000). Combined-type had greater sacroiliitis score compared with others (p = 0.002, 0.003).
Ankylosing spondylitis (AS) is a chronic inflammatory disease of the axial skeleton with involvement of peripheral joints and non-articular structures (1). Indeed, it is best known for its symptom of lower back pain; however, patients often present with hip or groin pain misleading the clinician to think that the cause lies primarily in the hips. Hip involvement as a common problem in AS increases the burden and negative affects its prognosis of AS than any other axial joints (2).
Femoroacetabular impingement (FAI) has been recently identified as a major cause of early primary osteoarthritis (OA) of the hip (3). FAI refers to abnormal contact between the femoral head-neck junction or the acetabular rim (4). A number of predisposing conditions have been described with deformities of the femur and the acetabulum which result in FAI including Legg-Calvé-Perthes, slipped capital femoral epiphysis, coxa magna, hip dysplasia, and fractures of the femoral neck (5).
Though FAI has not been recognized as a common radiologic feature of AS, we noticed FAI like features in hips of AS patients and hypothesized that AS may be predisposed to FAI. To the best of our knowledge, there has been no study about FAI pattern of hip involvement in AS. In this study, we investigated the prevalence and radiographic patterns of FAI in hips of AS patients. In addition, we evaluated the possible association between sacroiliitis grade and FAI according to different types.
This retrospective observational study was approved by the Institutional Review Board and informed consent was waived. Electronic medical records search revealed 543 patients diagnosed as AS or seronegative spondyloarthropathy from January 2004 to April 2012; out of these, 384 patients were included based on the following inclusion criteria: 1) clinically diagnosed as AS based on the New York criteria, 2) pelvis radiography, and 3) no previous hip surgery. We excluded patients with obvious severe OA and ankylosis of the hip (n = 61) or unavailability of lateral radiographs (n = 98). The typical radiographic findings of severe OA include definite joint space narrowing and/or osteophyte formation. A total of 384 patients [288 (72.3%) men, 96 women; mean age, 35.9 years; range 15-80 years] were included, of whom 296 patients were HLA-B27 positive.
Images included anteroposterior (AP) and translateral views of the hip. All patients underwent pelvic radiography to assess routine evaluation of AS. All of the images were retrospectively reviewed by two radiologists. FAI-like features were evaluated regarding the following: alpha angle, lateral center-edge (CE) angle, presence of pistol grip deformity in AS patients. Then they were classified into 3 types: cam, pincer, and combined-types.
The alpha angle was measured in the translateral radiograph in accordance with the method described by Nötzli et al. (6). The first line defining the α angle was located between the center of the femoral head and the point where the distance from the center of the femoral head to the peripheral contour of the femoral head exceeded the radius of the femoral head. The second line defining the α angle was the axis of the femoral neck, which was defined as a line that passed through the center of the femoral head and the center of the femoral neck at its narrowest point (Fig. 1) (7).
The lateral CE angle and pistol grip deformity were measured on AP radiographs. Excessive acetabular coverage can be quantified with the lateral CE angle (8). The lateral CE angle is the angle formed by a vertical line and a line connecting the femoral head center with the lateral edge of the acetabulum (Fig. 2) (9). A normal lateral CE angle varies between 25° (which defines a dysplasia) (10) and 39° (which is an indicator for acetabular overcoverage) (11). Also flattening of the head-neck junction (so called pistol grip deformity) was evaluated on AP radiographs (Fig. 3).
Cam type FAI was considered to be present when there was flattening of the head-neck junction (pistol grip deformity) and/or α angle > 55°; pincer FAI was considered when the lateral CE angle > 39° was detected. Combined type was considered in cases with findings of both types.
The prevalence of FAI types was determined and evaluated for the association with grades of sacroiliitis. Sacroiliac joints were graded according to the New York criteria established in 1966 (9), which describe five grades of sacroiliitis from 0 to 4 (0 = no disease, 1 = suspicious for disease, 2 = minimal disease, 3 = moderate disease, and 4 = severe disease). Images of 384 patients were analyzed by the first observer and they were also re-analyzed independently; a second observer evaluated the images after consensus training session with the first observer.
The measurements were performed by two radiologists (one with three years, the other with five years of experience) and their interrater reliabililty was tested. For the quantitative assessments (lateral CE angle, α angle), intraclass correlation coefficient (ICC) was used to evaluate interrater reliability. ICC was interpreted as indicating poor (ICC, 0-0.2), fair (ICC, 0.3-0.4), moderate (ICC, 0.5-0.6), strong (ICC, 0.7-0.8), or almost perfect (ICC, > 0.8) agreement. For the qualitative assessments (pistol-grip deformity), kappa analysis was used to evaluate interrater validity. Level of agreement was interpreted as indicating less than chance (κ ≤ 0), slight (κ = 0.01-0.20), fair (κ = 0.21-0.40), moderate (κ = 0.41-0.60), substantial (κ = 0.61-0.80), almost perfect (κ = 0.81-0.99), or perfect (κ = 1).
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software version 18.0 (SPSS Inc., Chicago, IL, USA). p values less than 0.05 were considered to be statistically significant. We performed t-test for numerical variables including age, sacroiliitis score, Kruskal-Wallis test for sacroiliitis score in three groups, and Mann-Whitney U-test, corrected by Bonferroni methods for post hoc analysis.
Among 384 patients, 141 (36.7%) had FAI pattern of hip joint involvement. Male predominance was found in the group with FAI pattern involvement (M:F = 123:18, 87.2%) compared with the group without hip involvement (M:F = 165:78, 67.9%) (p = 0.000) (Table 1). The group with FAI pattern of hip involvement also showed greater sacroiliitis score as compared with those without hip involvement (2.49 ± 1.19, 1.75 ± 1.19, p = 0.000). HLA-B27 was not different between FAI (-) and FAI (+) groups (75.3% vs. 75.2%, respectively, p = 0.977).
Regarding type of FAI (n = 141), it was composed of pincer-type (n = 79/384, 20.6%), cam-type (n = 25/384, 6.5%), and combined-type (n = 37/384, 9.6%); pincer type was the most common among the FAI types (Figs. 4,5,6). Sacroiliitis grade was different according to FAI types (p = 0.002); combined-type FAI pattern (n = 37, 3.05 ± 0.97) had greater sacroiliitis score than pincer (n = 79, 2.33 ± 1.19, p = 0.002) and cam-types (n = 25, 2.16 ± 1.25, p = 0.003), respectively (Table 2).
ICC was used to evaluate agreement between the two observers for each quantitative measurement and ranged from strong to almost perfect (0.78, 0.86). For the qualitative parameters, kappa analysis showed moderate agreement (0.54).
The importance of hip involvement in patients with AS has been recognized for several years as a common and disabling problem, whereas involvement of other peripheral joints is less common. Hip involvement is an important prognostic factor associated with radiographic progression (1); approximately 8 to 15% of AS patients with long-term follow-up have to undergo total hip joint replacement arthroplasty (12, 13). Though radiographic and clinical signs of hip involvement showed positive correlation in many studies, there has been no definite consensus on how to assess hip involvement (1) and radiologic pattern of hip involvement in AS patients.
Especially in the very early phase of hip involvement, patients may not have classic radiographic signs of OA, such as joint space narrowing, bone erosion, osteophyte formation or subchondral sclerosis on hip radiograph. During hip radiograph interpretation in AS patients, we found radiologic pattern of hip involvement similar to FAI in AS patients. So we postulated that the deformities caused by hip involvement in AS patients can change the mechanical function of the hip joint and contribute to FAI-like features on radiographs. We expected that AS patients have higher prevalence of FAI-like features than the general population and have association with higher grades of sacroiliitis.
In this study, we found FAI pattern of hip involvement in 36.7% of patients with AS. FAI has been reported to be present in 10-15% of general population (14). And recent CT study has shown that two or more abnormal parameters of FAI were present in 29% of joints in asymptomatic young populations (15). Also, FAI-like pattern was found in 35.3% of primary OA caused mostly by developmental dysplasia of the hip (16). Slipped capital femoral epiphysis is known as a predisposing condition of FAI; Dodds et al. (17) reported that among patients with after slipped capital femoral epiphysis, 32% had clinical signs of FAI. Although AS has not been previously investigated as a predisposing factor of FAI, FAI pattern of hip involvement was frequent in AS and higher prevalence of FAI-type features were found than in asymptomatic general population in our study.
Regarding type of FAI, pincer type FAI was the most common pattern in our study of AS patients, followed by combined and cam types. Most FAI patients (86%) are reported to have a combination of both forms of impingement and only a minority (14%) to have the pure cam or pincer type of FAI in the general population (18). Although the mechanism is unclarified, we hypothesize that pincer type FAI pattern may be caused by pronounced periarticular ossification at the acetabulum as a result of hip involvement of AS. This enthesopathy of acetabular rim may result in further overcoverage of the femoral head, which would produce the characteristic features of pincer type FAI. In AS patients with advanced hip OA, coxa profunda or protrusio acetabuli is usually seen on AP hip radiographs. Protrusio acetabuli is very common, occurring in as many as 33% of those with AS in the hip (19). A coxa profunda is defined as the floor of the fossa acetabuli touching or overlapping the ilioischial line medially and protrusio acetabuli occurs when the femoral head is overlapping the ilioischial line medially. These two findings increase the relative depth of the acetabulum and generally a deep acetabulum is associated with excessive acetabular coverage, which would predispose to further pincer type FAI (3).
Our findings of the positive correlation between hip involvement and sacroiliitis grade are consistent with results of other studies, suggesting a strong association of hip disease with more severe axial involvement (20,21,22). Sacroiliitis is the most frequent and earliest radiographic manifestation of AS. Doran et al. (20) noted that radiologic hip involvement is significantly associated with higher scores of radiologic change in the spine. In our study, hip involvement group also showed greater sacroiliitis score than AS without hip involvement. Regarding FAI pattern types, combined-type FAI pattern had greater sacroiliitis score compared with pincer and cam-types, respectively (p = 0.002, 0.003). We postulated that combined type is combination of both impingement types and it may be seen in more advanced state of hip involvement than pure pincer and cam types.
Inflammatory low back pain is the most typical presenting symptom of AS, which most likely represents sacroiliac and spinal involvement (23); hip joint stiffness and groin pain have been suggested to indicate hip involvement. In our study, among patients with FAI pattern hip involvement, 66.7% patients presented with hip or inguinal pain rather than lower back pain. We expected that patients with FAI involvement often showed painful symptom before the onset of classical radiographic degenerative change of AS (3). Also FAI triggers damage to the acetabular labrum and articular cartilage in the hip, which would aggravate hip pain. Radiographic findings may be very subtle and missed easily in the early stage of hip involvement of AS. Thus, early diagnosis and treatment are critical to prevent development of OA and/or delay the need for a more radical treatment option (24).
There are several limitations to our study. The group with hip involvement showed FAI like feature on radiograph, but it is unclear whether these patients had typical clinical hip symptoms of FAI. Many patients visited the rheumatologist for management of AS and in such cases there was no objective physical exmaination done regarding FAI, particularly flexion and internal rotation (9). We did not include control group of general population without symptom in our study, because there have been recent reports shown prevalence of radiographic findings of FAI in asymptomatic general population. Conventional pelvic radiographs were routinely used to initial assessment in AS patients, but it has limitations in evaluation of intra-articular structure damage. So if "FAI morphometric" features are present on routine conventional radiographs or patients presenting with severe hip symptoms, additional MRI should be done to visualize specific morphology around the hip joint that might need to be addressed surgically in the case of a clinical diagnosis of FAI.
In conclusion, FAI pattern of hip involvement was frequently seen in AS (36.7%), more frequent in male patients and associated with significantly greater grade of sacroiliitis (2.49 ± 1.19). Regarding type of FAI, pincer type was the most common pattern, followed by combined and cam types. Combined type FAI pattern had greater sacroiliitis score than pincer and cam-types.
Figures and Tables
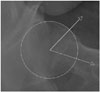 | Fig. 1Radiographic presentations of alpha angle on translateral radiograph by drawing a circle along the femur head circumference, drawing a line between the center of the circle and the point of head-neck offset, according to the method described by Nötzli et al. (6). |
 | Fig. 2Radiographic presentations of lateral center-edge angle on anteroposterior radiographs. The lateral center edge angle is the angle formed by a vertical line and a line connecting the femoral head center with the lateral edge of the acetabulum. |
 | Fig. 3Radiographic presentations of flattening of the head-neck junction (so called pistol grip deformity) on anteroposterior radiographs. |
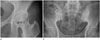 | Fig. 4Pelvic radiograph of 33-year-old man with ankylosing spondylitis.
A. Pincer type femoroacetabular impingement pattern showing lateral center-edge angle estimated to be 52.3°.
B. Demonstrating bilateral sacroiliitis grade 3, showing subchondral sclerosis and irregularities of the joint surface, including erosions.
|
 | Fig. 5Pelvic radiograph of in 26-year-old man with ankylosing spondylitis.
A. Cam type femoroacetabular impingement pattern showing alpha angle estimated to be 62.4°.
B. Demonstrating bilateral sacroiliitis grade 2, showing equivocal subchondral sclerosis.
|
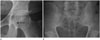 | Fig. 6Pelvic radiograph of 31-year-old man with ankylosing spondylitis.
A. Combined type femoroacetabular impingement pattern showing lateral center-edge angle estimated to be 45.0° and positive pistol grip deformity.
B. Demonstrating bilateral sacroiliitis grade 4, showing complete ankylosis.
|
Table 1
Demographics & Presence of FAI Pattern in Patients with Ankylosing Spondylits

| FAI Pattern (+) | FAI Pattern (-) | p-Value | |
|---|---|---|---|
| Sex | 0.000* | ||
| Male | 123 (67.9%) | 165 (87.2%) | |
| Female | 18 (32.1%) | 78 (12.8%) | |
| Sacroiliitis grade | 2.49±1.19 | 1.75±1.19 | 0.000† |
| Total number | 141 | 243 |
References
1. Baraliakos X, Braun J. Hip involvement in ankylosing spondylitis: what is the verdict? Rheumatology (Oxford). 2010; 49:3–3.
2. Vander Cruyssen B, Muñoz-Gomariz E, Font P, Mulero J, de Vlam K, Boonen A, et al. Hip involvement in ankylosing spondylitis: epidemiology and risk factors associated with hip replacement surgery. Rheumatology (Oxford). 2010; 49:73–78.
3. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007; 188:1540–1552.
4. Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology. 2012; 263:475–483.
5. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010; 92:2436–2444.
6. Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002; 84:556–560.
7. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006; 240:778–785.
8. Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990; (261):214–223.
9. Tannast M, Siebenrock KA, Anderson SE. [Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know]. Radiologia. 2008; 50:271–284.
10. Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995; 77:985–998.
11. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999; 81:1747–1770.
12. Gran JT, Skomsvoll JF. The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol. 1997; 36:766–771.
13. Robertson LP, Davis MJ. A longitudinal study of disease activity and functional status in a hospital cohort of patients with ankylosing spondylitis. Rheumatology (Oxford). 2004; 43:1565–1156.
14. Leunig M, Beck M, Dora C, Ganz R. [Femoroacetabular impingement: trigger for the development of coxarthrosis]. Orthopade. 2006; 35:77–84.
15. Chakraverty JK, Sullivan C, Gan C, Narayanaswamy S, Kamath S. Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms. AJR Am J Roentgenol. 2013; 200:389–395.
16. Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop. 2009; 33:1229–1232.
17. Dodds MK, McCormack D, Mulhall KJ. Femoroacetabular impingement after slipped capital femoral epiphysis: does slip severity predict clinical symptoms? J Pediatr Orthop. 2009; 29:535–539.
18. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005; 87:1012–1018.
19. McBride MT, Muldoon MP, Santore RF, Trousdale RT, Wenger DR. Protrusio acetabuli: diagnosis and treatment. J Am Acad Orthop Surg. 2001; 9:79–88.
20. Doran MF, Brophy S, MacKay K, Taylor G, Calin A. Predictors of longterm outcome in ankylosing spondylitis. J Rheumatol. 2003; 30:316–320.
21. Brophy S, Mackay K, Al-Saidi A, Taylor G, Calin A. The natural history of ankylosing spondylitis as defined by radiological progression. J Rheumatol. 2002; 29:1236–1243.
22. Brophy S, Calin A. Ankylosing spondylitis: interaction between genes, joints, age at onset, and disease expression. J Rheumatol. 2001; 28:2283–2288.
23. Sampaio-Barros PD, Bertolo MB, Kraemer MH, Neto JF, Samara AM. Primary ankylosing spondylitis: patterns of disease in a Brazilian population of 147 patients. J Rheumatol. 2001; 28:560–565.
24. Hickman JM, Peters CL. Hip pain in the young adult: diagnosis and treatment of disorders of the acetabular labrum and acetabular dysplasia. Am J Orthop (Belle Mead NJ). 2001; 30:459–446.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download