Abstract
Although endoscopic retrograde cholangiopancreatography (ERCP) is an effective modality for diagnosis and treatment of biliary and pancreatic diseases, the risk for procedure-related complications is high. Hemorrhage is one of major complications of ERCP. Most ERCP-associated bleeding is primarily a complication related to sphincterotomy rather than diagnostic ERCP. We are reporting a case of massive hemobilia due to hepatic arteriobiliary fistula caused by guidewire-associated injury during ERCP, which was successfully treated with transarterial embolization of the hepatic artery.
Endoscopic retrograde cholangiopancreatography (ERCP) is commonly performed to diagnose and treat hepato-pancreato-biliary diseases. But it has a higher potential for procedure-related complications compared to other endoscopic procedures in the upper gastrointestinal tract (1). Even in the best hands, serious complications from therapeutic ERCP occur in 2.5-8% of cases, with mortality ranging from 0.5-1.1% (2). Guidewire cannulation is widely used for bile duct cannulation during ERCP. Although complications of ERCP due to guidewire-related injury are rare and can be managed conservatively, they can be life-threatening (3). We report on a case of massive hemobilia due to hepatic arteriobiliary fistula caused by guidewire-associated injury during ERCP that was successfully treated with hepatic arterial embolization. To the best of our knowledge, this is the first report of a hepatic arteriobiliary fistula caused by guidewire-associated injury during ERCP.
A 67-year-old woman presented with acute upper abdominal pain, nausea, and vomiting. She denied any fever, chills, recent gastrointestinal bleeding, or taking anticoagulant medication. Biochemistry tests revealed cholestatic liver function and pancreatitis. Laboratory tests data were as follows: total bilirubin, 3.0 mg/dL (0.1-1.2 mg/dL); direct bilirubin, 2.1 mg/dL (0.1-0.4 mg/dL); aspartate aminotransferase, 360 U/L (15-40 U/L); alanine aminotransferase, 314 U/L (0-40 U/L); alkaline phosphatase, 315 U/L (25-100 U/L); γ-glutamyltransferase, 182 U/L (0-50 U/L); amylase, 529 U/L (20-104 U/L); and lipase, 1723 U/L (5.6-51.3 U/L). Coagulation was within normal limits. Abdominal computed tomography (CT) revealed diffuse dilatation of the common bile duct with left intrahepatic duct stones and a normal pancreatic appearance.
The next day, she underwent ERCP under a diagnosis of choledocholithiasis with biliary pancreatitis. Duodenoscopy revealed no mass in the ampulla of Vater and confirmed that there was no bleeding from the papilla. To cannulate the bile duct, a 0.025-inch guidewire was advanced during the sphincterotomy under endoscopic and fluoroscopic guidance. The patient suddenly complained of sharp upper abdominal pain and was extremely irritability during ERCP. Duodenoscopy revealed fresh blood gushing from the papilla. The patient was immediately moved to the angiographic suites for an angiography. Hepatic arteriography revealed active contrast extravasation into the bile duct from the anterior superior branch of the right hepatic artery (Fig. 1). Fluoroscopy following arteriography showed irregular, cast-like filling defects that occupied the majority of the bile duct (Fig. 2). Subsequently, selective coil embolization of the hepatic artery branch was successfully performed (Fig. 3). Percutaneous transhepatic biliary drainage (PTBD) was performed simultaneously. Although the patient remained hemodynamically stable, follow-up laboratory tests on the same day revealed decreased hemoglobin levels from 11.4 to 9.2 g/dL. The patient had no further bleeding.
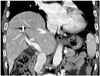
Follow-up CT was performed 2 weeks after coil embolization, which showed no evidence of a subcapsular hematoma or perihepatic free air, which suggests liver perforation (Fig. 4). During the 1-month follow-up period, the patient's liver function and pancreatic enzymes were normalized, and the intrahepatic duct stones were cholangioscopically removed.
There are a few published reports of guidewire-associated injury during ERCP that resulted in subcapsular hepatic hematoma (4), subcapsular biloma (5), liver parenchyma perforation (6), and portobiliary fistula (7). Most of these reports explain that these complications are the result of accidental puncture of the intrahepatic bile duct by the guidewire. To the best of our knowledge, this is the first report of a hepatic arteriobiliary fistula caused by guidewire-associated injury during ERCP.
Post ERCP-associated hemorrhage is primarily a complication related to the sphincterotomy rather than the diagnostic ERCP. Bleeding following a sphincterotomy has been variably reported in < 1% to 10% of the patients. Most sphincterotomy site bleedings are managed successfully by supportive conservative measures with or without an endoscopic hemostatic procedure. In only a small percentage of cases, refractory bleeding occurs and requires angiographic embolization or surgery (8). In addition, while bleeding at the site of a sphincterotomy usually presents as duodenal bleeding, hemobilia due to arteriobiliary fistula presents as massive hemorrhage in the intrahepatic bile duct, which increases intraductal pressure and may aggravate biliary complications such as obstructive jaundice, cholangitis, and sepsis. Therefore, if there is sudden fresh bleeding from the bile duct, as in this case, a diagnosis of hepatic arteriobiliary fistula should be considered to differentiate from sphincterotomy site bleeding.
Although hemobilia is an uncommon cause of upper gastrointestinal bleeding, its incidence is increasing due to more frequent use of local diagnostic and therapeutic interventions. As a result, hemobilia, which used to occur as a consequence of blunt or penetrating liver trauma in the past, is now mostly iatrogenic following liver biopsy, PTBD, hepatic intraarterial chemotherapy, or hepatobiliary surgery (9). The possible explanation for an arteriobiliary fistula include direct injury to the arteries of the bile duct, tumor necrosis, mycotic pseudoaneurysm of hepatic artery, and endothelial toxicity due to chemotherapeutic medication. In the present case, the hepatic arteriobiliary fistula resulted from a direct injury to the hepatic artery, which led to massive hemobilia requiring urgent treatment.
Although complications of ERCP that are caused by guidewire-related injury are rare and can be managed conservatively, they may be life-threatening and require arteriographic embolization or surgery. In the literature, subcapsular hematomas that have been the most commonly reported guidewire-associated complication of ERCP, which usually developed a few hours after ERCP and was successfully managed conservatively or by a simple drainage procedure (4). Massive hemobilia from hepatic arteriobiliary fistula should be considered a serious complication that requires more aggressive and urgent therapeutic interventions. Transcatheter arterial embolization is a safe and effective life-saving treatment for massive hemobilia and should be considered a first-line therapy (10). The primary goal of therapy is to decrease pulsatile blood pressure distal to the artificial occlusion. The risk of hepatic necrosis is minimal with superselective embolization. In the present case, selective angiography of the hepatic arteries was performed immediately after ERCP and selective coil embolization of the hepatic artery was successfully performed.
In conclusion, massive hemobilia in the present case was most likely due to an arteriobiliary fistula caused by a guidewire-related injury during ERCP and was successfully treated with selective coil embolization of the hepatic artery. A hepatic arteriobiliary fistula caused by guidewire-associated injury during ERCP is an extremely rare complication, but should be part of the differential diagnosis when there is bleeding at the site of a sphincterotomy. More attention should be paid to the possibility of guidewire-related complications, and if an arteriobiliary fistula is suspected, immediate hepatic angiography is required to detect and eventually embolize the damaged artery.
Figures and Tables
Fig. 1
Selective hepatic arteriography showed an arteriobiliary fistula (arrow) with active contrast extravasation into the bile duct (arrowheads).

Fig. 2
Fluoroscopy following hepatic arteriography revealed irregular cast-like filling defects (arrows) in the bile duct due to massive hemobilia.

References
1. Aliperti G. Complications related to diagnostic and therapeutic endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 1996; 6:379–407.
2. Hart R, Classen M. Complications of diagnostic gastrointestinal endoscopy. Endoscopy. 1990; 22:229–233.
3. Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, Pappas TM, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298.
4. Del Pozo D, Moral I, Poves E, Sanz C, Martín M. Subcapsular hepatic hematoma following ERCP: case report and review. Endoscopy. 2011; 43:Suppl 2 UCTN. E164–E165.
5. Dupas JL, Mancheron H, Sevenet F, Delamarre J, Delcenserie R, Capron JP. Hepatic subcapsular biloma. An unusual complication of endoscopic retrograde cholangiopancreatography. Gastroenterology. 1988; 94(5 Pt 1):1225–1227.
6. Kayashima H, Ikegami T, Kasagi Y, Hidaka G, Yamazaki K, Sadanaga N, et al. Liver Parenchyma Perforation following Endoscopic Retrograde Cholangiopancreatography. Case Rep Gastroenterol. 2011; 5:487–491.
7. Kawakami H, Kuwatani M, Kudo T, Ehira N, Yamato H, Asaka M. Portobiliary fistula: unusual complication of wire-guided cannulation during endoscopic retrograde cholangiopancreatography. Endoscopy. 2011; 43:Suppl 2 UCTN. E98–E99.
8. Ferreira LE, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007; 102:2850–2858.
9. Green MH, Duell RM, Johnson CD, Jamieson NV. Haemobilia. Br J Surg. 2001; 88:773–786.
10. Srivastava DN, Sharma S, Pal S, Thulkar S, Seith A, Bandhu S, et al. Transcatheter arterial embolization in the management of hemobilia. Abdom Imaging. 2006; 31:439–448.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download