Abstract
Purpose
Materials and Methods
Results
Conclusion
Figures and Tables
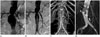 | Fig. 2A 74-year-old female with abdominal aortic aneurysm (patient number 7 on Table 1).
A. Preimplantation abdominal aortogram demonstrated "hostile" proximal neck (arrow) which has flask shaped appearance.
B. Postimplantation abdominal aortogram showed good placement of aortic stent-graft without evidence of endoleak.
C. Volume-rendering CT image showed no endoleak on 5 days of the placement of aortic stent-graft.
D. Maximum intensity projection CT image revealed newly developed type 3 endoleak (arrow) between main body and right limb stent-graft on 48 months after the placement of aortic stent-graft.
|
 | Fig. 3An 82-year-old male with abdominal aortic aneurysm with bilateral common iliac artery involvement (patient number 24 on Table 1).
A. Preimplantation abdominal aortogram showed diffuse dilatation of infrarenal abdominal aorta and bilateral common iliac arteries. The proximal neck had "hostile" anatomy due to severe angulation.
B. Postimplantation abdominal aortogram showed good placement of aortic stent-graft without evidence of endoleak. However, left proximal limb stent-graft (arrow) showed significant stenosis due to angulation.
C, D. On 19 days after aortic stent-graft placement, we performed balloon angioplasty (C) and placement of balloon-expandable stent (D) at left proximal limb stent-graft. There was a waist (arrow) during balloon angioplasty showing significant stenosis.
|
Table 1
Summary of 33 Patients with Aortoiliac Aneurysms Treated with SEAL Aortic Stent-Graft Placement

| Pts | Sex/Age | Initial Diagnosis* | Proximal Neck | CIA | EIA | SG Type‡ | TS§ | Endoleak∥ | Other Cx¶ | CS** | Cause of Death | Figures | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diameter | Length | Angle | Wall† | Diameter | Length | Diameter | Type | Detection Time | Additional Intervention | Outcome | |||||||||
| 1 | M/72 | AAA | 28 | 25 | 35 | T | 18 | 40 | 8 | B | O | Steno | O | Aspiration | |||||
| 2 | M/79 | AAA with R | 26 | 30 | 5 | T | 16 | 28 | 8 | B | O | Steno | O | Sepsis | |||||
| 3 | M/68 | IAA | 28 | 105 | 24 | 55 | 11 | B | O | O | |||||||||
| 4 | M/62 | IAA | 28 | 180 | 19 | 140 | 12 | B | O | O | |||||||||
| 5 | M/64 | AAA | 24 | 35 | 18 | T | 12 | 56 | 6 | B | O | O | |||||||
| 6 | M/56 | AAA | 20 | 35 | 15 | 13 | 68 | 7 | B | O | O | Gastric cancer | |||||||
| 7 | F/74 | AAA | 34 | 0 | 25 | 12 | 39 | 7 | B | O | 3 | N (48 mo) | Additional stent-graft | On F/U | Migr | O | Fig. 2 | ||
| 8 | M/69 | AAA + IAA | 26 | 35 | 60 | 46 | 77 | 8 | B | O | O | ||||||||
| 9 | M/78 | AAA | 19 | 21 | 51 | 16 | 27 | 8 | B | O | O | ||||||||
| 10 | M/66 | AAA | 32 | 16 | 11 | 18 | 32 | 7 | B | O | 1B | N (59 mo) | Additional stent-graft | F/U loss | Migr | X | Delayed AAA rupture | ||
| 11 | M/65 | AAA | 27 | 40 | 18 | C | 15 | 25 | 9 | B | O | 2 (IMA) | R | IMA embolization | Disapp | Steno | O | ||
| 12 | M/75 | AAA | 22 | 50 | 35 | C | 16 | 25 | 10 | B | O | 1B | R | ↓ | O | ||||
| 13 | M/69 | AAA + IAA | 20 | 50 | 13 | 52 | 45 | 12 | B | O | O | ||||||||
| 14 | M/83 | AAA with CR | 32 | 33 | 116 | T | 19 | 33 | 11 | B | X | X | AAA rupture | ||||||
| 15 | F/76 | AAA | 32 | 30 | 39 | 24 | 24 | 8 | B | O | O | ||||||||
| 16 | F/88 | AAA | 23 | 79 | 89 | 17 | 33 | 8 | B | O | 1A | R | F/U loss | X | |||||
| 17 | M/81 | AAA | 31 | 30 | 57 | C | 21 | 35 | 9 | B | O | 1B | R | F/U loss | X | ||||
| 18 | M/67 | AAA with R | 26 | 45 | 32 | 14 | 25 | 7 | B | O | 1B | N (41 mo) | Additional stent-graft | On F/U | Migr | O | |||
| 19 | M/64 | AAA | 26 | 55 | 44 | T | 13 | 40 | 7 | B | O | O | |||||||
| 20 | M/70 | AAA + IAA | 20 | 75 | 46 | 39 | 40 | 10 | B | O | 2 (L) | R | ↓ | Steno | O | ||||
| 21 | F/77 | AAA with R | 20 | 27 | 91 | 12 | 18 | 9 | B | O | O | ||||||||
| 22 | F/75 | AAA with CR | 23 | 45 | 41 | T | 14 | 20 | 7 | B | O | O | |||||||
| 23 | M/58 | AAA with CR | 23 | 36 | 33 | 16 | 37 | 10 | B | O | O | ||||||||
| 24 | M/82 | AAA | 22 | 27 | 68 | T | 17 | 39 | 11 | B | O | 2 (IMA) | R | F/U loss | X | Acute MI | Fig. 3 | ||
| 25 | F/85 | AAA with R | 17 | 30 | 30 | C | 9 | 20 | 6 | B | O | X | AAA rupture | ||||||
| 26 | M/71 | AAA | 21 | 75 | 30 | 12 | 20 | 11 | B | O | 2 (IMA) | R | ↓ | O | |||||
| 27 | M/74 | AAA | 33 | 59 | 93 | T | 24 | 36 | 11 | B | O | 2 (L) | R | Disapp | X | ||||
| 5 | N (28 mo) | On F/U | |||||||||||||||||
| 28 | M/80 | AAA | 26 | 35 | 89 | 25 | 25 | 11 | B | O | 2 (L) | R | ↓ | O | |||||
| 29 | M/80 | AAA | 25 | 24 | 78 | 15 | 39 | 9 | B | O | O | ||||||||
| 30 | M/66 | AAA | 22 | 21 | 74 | 12 | 21 | 10 | B | O | O | ||||||||
| 31 | M/84 | AAA | 28 | 35 | 62 | 20 | 20 | 9 | B | O | O | Medullary paralysis | |||||||
| 32 | M/76 | IAA with R | 29 | 120 | C | 36 | 55 | 12 | B | O | 2 (IIA) | R | ↓ | O | |||||
| 33 | M/79 | AAA | 25 | 30 | 38 | 20 | 30 | 8 | B | O | O | ||||||||
Note.-*Initial diagnosis: AAA = abdominal aortic aneurysm, IAA = iliac artery aneurysm, R = rupture, CR = contained rupture
†Proximal neck wall: T = thrombosis, C = calcification
‡Stent-graft types: B = bifurcated type, T = tubular type
§Technical success: O = success, X = failed
∥Endoleak type: IMA = inferior mesenteric artery, L = lumbar artery, Endoleak detection time = interval between initial intervention and initially detected time (months), N = newly appeared endoleak, R = residual endoleak, Outcome: F/U = follow-up, Disapp = disappeared endoleak on follow-up CT, ↓ = decreased endoleak on follow-up CT
¶Other complications: Steno = limb stent-graft stenosis, Migr = stent-graft migration
**Clinical success: O = success, X = failed




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download