Abstract
Various musculoskeletal findings incidentally detected on abdominopelvic computed tomography (CT) images have risen with the increasing use of abdominopelvic CT; however, it is not uncommon for radiologists to overlook the musculoskeletal system when they examine abdominopelvic CT images. Some musculoskeletal lesions may have more clinical significance than abdominopelvic lesions, although most lesions are of little to no significance. Many osseous lesions can be diagnosed using the bone window setting and reconstructed images. The purpose of this article was to review the wide variety of musculoskeletal lesions depicted on abdominopelvic CT images and to emphasize the use of the bone window setting.
As abdominopelvic computed tomography (CT) scans are increasingly used, "incidental findings", or detection of lesions unrelated to the original purpose of the scan, have increased (1). Abdominopelvic CT images usually provide sufficient information to identify several incidental musculoskeletal abnormalities, which may or may not be related to the patient's symptoms. However, radiologists often overlook musculoskeletal lesions depicted on abdominopelvic CT images, which typically include various osseous and soft tissue lesions of the pelvis, hip, or spine (Table 1). Some musculoskeletal lesions may have more clinical significance than abdominopelvic lesions, although most lesions may have little or no significance.
The purpose of this article was to illustrate the various musculoskeletal lesions depicted on abdominopelvic CT images and to emphasize the importance of analyzing the musculoskeletal system during interpretation of abdominopelvic CT images.
Various minor, incidental musculoskeletal lesions, such as spondylolisthesis, perineural cysts and benign tumorous lesions (hemangioma, lipoma, intraosseous lipoma, and osteochondroma) are encountered in daily practice.
Spondylolisthesis refers to the ventral slip of one vertebra relative to the vertebra below. Radiologists are likely to overlook spondylolisthesis on abdominal CT because abdominal CT typically does not acquire a sagittal image. Isthmic spondylolisthesis (type II) is characterized by bilateral defects of pars interarticularis. The most common site is at the level of L5 and S1. Common radiographic features include pars defects with double facet joint sign on axial CT scan and a widened spinal canal (Fig. 1).
Degenerative spondylolisthesis (type III) occurs as a consequence of the general aging process. It may be associated with spinal canal stenosis and lower back or leg pain (2). The most common location is the L4 and L5 level of the lower spine. CT shows malalignment of the facet joint and the intact neural arch. Sagittal orientation of the facet joints can be shown on axial CT scans (Fig. 2). MRI is an excellent device to confirm spondylolisthesis and central canal stenosis with nerve root compression.
Soft tissue hemangiomas are benign vascular soft tissue tumors. They are location-dependent, and represent approximately 7% of all benign soft-tissue tumors (3). They occur in various locations, including the skin, striated muscle, subcutaneous tissue, and synovial tissue. Unenhanced CT images reveal an ill-defined mass with a similar attenuation to muscle. The differential diagnosis on CT images includes lipoma and hematoma. Hemangiomas can be associated with phleboliths (Fig. 3). Phleboliths are present in up to 85% of intramuscular hemangiomas and can be a highly specific sign of soft tissue hemangioma. Ultrasonography can show a complex mass with acoustic shadowing associated with phleboliths. Hemangiomas may appear as a lobulated and heterogeneous mass on magnetic resonance imaging (MRI). T1-weighted images reveal intermediate to slightly high signal with some focal high signal areas. On T2-weighted images, hemangiomas show high signal intensity (4).
Intraosseous lipomas are rare, benign bone lesions. They commonly occur in the metaphyseal region of long bones and the calcaneus. They can also appear in the pelvis, flat bones, and other locations. A major symptom is pain, but more than 30% of intraosseous lipomas are found incidentally on imaging done for other reasons (5). On plain radiography, an intraosseous lipoma presents as a well-circumscribed, osteolytic lesion surrounded by a sclerotic border with osseous septations or calcification. CT and MRI scans are extremely valuable for the diagnosis of intraosseous lipoma. Fatty components of intraosseous lipomas may show varying degrees of involution and necrosis. CT images show a lesion that has a density similar to fat with an expanded cortex (Fig. 4). MRI can be useful for a final diagnosis. Fatty tissue shows high signals on T1-weighted and T2-weighted MRI but low signals on fat-suppressed MR images.
Osteochondromas are usually considered as benign bone tumors. They typically originate in the appendicular skeleton, especially around the knee. They can appear at any age and their finding is mostly incidental. Osteochondromas exhibit continuity of the cortex and cancellous bone with the parent bone and have a cap of hyaline cartilage. On CT images, an osteochondroma can be seen as a peripheral bone projection with medullary cancontinuity and a cartilage cap (Fig. 5). MRI is the best modality to assess cartilage thickness, as a cartilage cap of over 1.5 cm thickness is suspected for malignant degeneration.
A perineural cyst is identified as a cerebrospinal fluid (CSF)-filled mass of the nerve root sheath. Most perineural cysts are detected incidentally and are asymptomatic. Some have associated symptoms such as lower back pain. Perineural cysts appear as isoattenuated cystic masses relative to CSF of the neural foramen on CT images (Fig. 6). Bone remodeling and enlargement of the neural foramen may occur as a result of increased CSF pressure. Perineural cysts show low signal intensity on T1-weighted MRI and high signal intensity on T2-weighted images (6).
As some musculoskeletal findings on abdominopelvic CT are misdiagnosed and overestimated, the finding of these lesions may lead to unnecessary workup. For example, bony sclerotic lesions in cancer patients can be misdiagnosed as bone metastasis, although the lesions are benign. Moreover, compression fractures in cancer patients are often misdiagnosed as malignant lesions. Conversely, other musculoskeletal lesions may have more clinical significance than abdominopelvic lesions, which may require treatment.
Bone metastases are a frequent complication in advanced canincer. Bone involvement is common, especially in metastatic breast or prostate cancer (Fig. 7) (7). Skeletal involvement can cause various symptoms, including severe pain and pathologic fractures. Bone metastases are generally classified as osteolytic or osteoblastic, and both are characterized by dysregulation of the normal bone remodeling process.
Avascular necrosis of the femoral head is caused by decreased vascular supply to the subchondral bone. Most causes of avascular necrosis of the femoral bone are trauma, chronic steroid use, alcoholism and prior hip surgery. The most common symptom is pain in the hip, thigh, groin, and buttock. On CT scan, avascular necrosis can be seen in central or peripheral areas of reduced attenuation with sclerosis (Fig. 8A) and subchondral fractures. MRI is the most effective diagnostic method for osteonecrosis. A "double line sign" is characteristic of avascular necrosis, consisting of inner high signal intensity with a low intensity peripheral rim on T2-weighted MRIs (Fig. 8B). The inner rim represents granulation tissue and the outer rim represents sclerotic bone. On T1-weighted images, avascular necrosis can be seen as a thin, low-signal rim with a variable signal at the center (Fig. 8C) (8).
Compression fracture is a common problem in elderly patients. It is difficult to differentiate malignant compression fractures from benign compression fractures. CT findings of benign compression fractures include well-defined, fracture lines and cortical fractures involving an anterolateral aspect of the vertebral body (Fig. 9). However, malignant compression fractures usually involve the pedicle or posterior elements and show a paraspinal or epidural mass (Fig. 10). MRI is the most reliable method to differentiate between benign and malignant compression fractures. MRI findings, including abnormal signal intensity of the pedicle or posterior element, convex posterior border of the vertebral body, and epidural mass or paraspinal mass, are suggestive of metastatic compression fracture.
Total hip arthroplasty has become common over the past 50 years. Despite technological improvements, a small but significant minority of patients develop complications. Recognizing and diagnosing these complications are important as many of these patients require revision. Complications related to total hip replacement include infection, abscess, fracture, osteolysis, and mechanical loosening (Fig. 11).
Various musculoskeletal abnormalities can be identified incidentally on abdominopelvic CT images. It is important to review musculoskeletal findings and report the abnormalities to the patient. Some of these findings could be related to the patient's symptoms, although most lesions may have little or no significance. If the bone setting window is used and radiologists become aware of musculoskeletal abnormalities in CT images, they are better able to identify musculoskeletal lesions on abdominopelvic CT images.
Figures and Tables
Fig. 1
Isthmic spondylolisthesis in a 65-year-old male with lung cancer.
A. Axial CT scan with bone window setting demonstrates lucent defects of both pars interarticularis with double facet joint sign (arrows) and widening of the spinal canal at the level of L4.
B. Sagittal T2-weighted MRI shows defect of pars interarticularis (arrow) and anterior spondylolisthesis of L4.
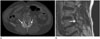
Fig. 2
Spondylolisthesis in a 56-year-old female with cecal colon cancer undergoing a routine follow-up CT scan.
A, B. Axial CT scans show subluxation of the facet joint with a sagittal orientation of the facet joints (A, arrow) and narrowing of the spinal canal space (B, arrow). This suggests degenerative spondylolisthesis.
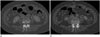
Fig. 3
Soft tissue hemangioma in a 51-year-old man with early gastric cancer.
A. Axial CT scan reveals a soft tissue mass containing phleboliths (arrow) on the right lower abdominal wall.
B. Abdominal wall ultrasonography shows an ill-defined, heterogeneous, nodular lesion with echogenicity and calcific foci (arrow) in the subcutaneous layer at the right lower quadrant of the abdominal wall. This suggests soft tissue hemangioma.

Fig. 4
Intraosseous lipoma of the left ilium in a 48-year-old man with left abdominal pain.
A. Axial non-enhanced axial CT scan shows osteolytic bone lesions (arrow) in the left ilium.
B. Axial CT scan with bone window setting shows a calcification or septa-like structure (arrow) in the lesion. The lesion shows low attenuation (Hounsfield unit -50), suggestive of fat components in the left ilium.
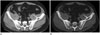
Fig. 5
Osteochondroma of the iliac tuberosity in 62-year-old man. Axial CT scan shows exophytic outgrowths (arrow) on the surface that are composed of cortical and medullary bone of the iliac tuberosity, which is suggestive of osteochondroma.

Fig. 6
Perineural cyst in a 49-year-old female with left abdominal pain. Axial CT scan shows an enlarged left sacral foramen filled with soft tissue (arrow), which indicates a perineural cyst.

Fig. 7
Multifocal metastases in a 54-year-old female with invasive ductal carcinoma.
A. Coronal CT scan shows several low-attenuated lesions (arrow) on the right hepatic lobe, which suggests hepatic metastasis. It shows a sclerotic lesion on the T12 body (arrowhead).
B. Coronal CT scan does not show a definite bony lesion on the sacrum.
C. Follow-up CT scan after one year shows decreased size of the hepatic metastatic lesions (arrow). The size of the previous sclerotic lesion is increased (arrowhead).
D. Follow-up CT scan after one year shows a new visible mixed osteolytic and osteoblastic lesion (arrows) on the sacrum, which suggests bone metastasis.

Fig. 8
Avascular necrosis of both femoral heads in a 44-year-old woman with lower abdominal pain.
A. Axial CT scan shows curvilinear zones of sclerosis (arrows), suggestive of ischemic necrosis of the both femoral heads. There is no collapse of the articular surface.
B. Axial T2-weighted MR image reveals peripheral line of low signal intensity and an inner zone of high signal intensity in the subchondral region of the both femoral head (arrows).
C. Coronal T1-weighted MR image shows low signal peripheral lines in the subchondral region of the both femoral heads (arrows).

Fig. 9
Benign compression fracture in a 61-year-old man with cholangiocarcinoma.
A. Axial CT scan shows definite fracture lines (arrow) in the anterior column at the level of L4; however, the posterior element is relatively intact. Moreover, paraspinal mass or epidural mass are not seen.
B. Coronal CT scan reveals loss of vertebral height and cortical depression and discontinuity of the lower endplate (arrow), which indicates a compression fracture at the L4 level.

Fig. 10
Malignant compression fracture in a 55-year-old patient with lung cancer.
A. Axial CT scan shows an osteolytic lesion in the vertebral body and a spinous process with an epidural mass (arrow) at the level of L5.
B. Coronal CT shows a compression fracture at the L5 level (arrow) and multiple osteolytic lesions on the L-spine.

Fig. 11
Incidental periprosthetic abscess found in an 88-year-old woman with lower abdominal pain.
A. Coronal CT scan shows a low-attenuated lesion with uniformly thick enhancing wall (arrow) surrounding the left total hip replacement.
B. Fluoroscopy shows a contrast-filled space (arrow) in the posterolateral portion of the left hip joint. Turbid and brownish exudative fluid was drained by aspiration.

Table 1
Classification of the Incidental Musculoskeletal Findings Detected on Abdominopelvic CT According to Their Clinical Importance

References
1. Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010; 7:754–773.
2. Butt S, Saifuddin A. The imaging of lumbar spondylolisthesis. Clin Radiol. 2005; 60:533–546.
3. Pourbagher A, Pourbagher MA, Karan B, Ozkoc G. MRI manifestations of soft-tissue haemangiomas and accompanying reactive bone changes. Br J Radiol. 2011; 84:1100–1108.
4. Olsen KI, Stacy GS, Montag A. Soft-tissue cavernous hemangioma. Radiographics. 2004; 24:849–854.
5. Campbell RS, Grainger AJ, Mangham DC, Beggs I, Teh J, Davies AM. Intraosseous lipoma: report of 35 new cases and a review of the literature. Skeletal Radiol. 2003; 32:209–222.
6. Hain KS, Pickhardt PJ, Lubner MG, Menias CO, Bhalla S. Presacral masses: multimodality imaging of a multidisciplinary space. Radiographics. 2013; 33:1145–1167.
7. Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J Cancer. 1987; 55:61–66.
8. Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007; 63:16–28.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download