Abstract
Purpose
To evaluate the efficacy and safety of radiologic venous port placement in children under venous anesthesia.
Materials and Methods
Between April 2009 and July 2011, 44 ports were implanted in 41 children (24 boys, 17 girls). The age of patients ranged from 9 months to 19 years (mean, 6.5 years) and their body weights ranged from 6.8 kg to 56.3 kg (mean, 23.2 kg). Right internal jugular vein access was used in 42 ports, right subclavian vein in 1, and left subclavian in 1. Durability and complications of port implantation were reviewed.
Results
The technical success rate was 100%. The catheter life was 10-661 days (mean 246 days). Two patients died during the follow-up period, 21 and 6 ports were removed at the end of treatment or as a result of complications, respectively. One port was removed and replaced by a Hickmann catheter. Three ports were explanted due to port-related sepsis, one due to a catheter kink, and two for unexplained fever or insertion site pain. The overall port-related infection was 3 cases (6.8%, 0.28/1000 catheter days).
Figures and Tables
Fig. 1
A 3-year-old girl with hemophagocytic syndrome is refered for chemoport insertion.
A. Right internal jugular vein is used for access route. Spot image shows a catheter tip is located at superior vena cava level, that means higher than usual location. Chemoport had been used for 177 days.
B. Spot image of patient just before removal shows kinking of the catheter at the neck area (arrow).
C. Right subclavian vein is used for access route at 2nd insertion. A right subclavian central catheter is changed into chemoport. The port was removed after treatment termination. The catheter has been used about 1 year.
D. Left subclavian vein is used at 3rd insertion. Guide wire is inserted into central catheter and changed into peel-away sheath. Spot image after port insertion shows catheter tip is located slightly above cavoatrial junction (arrow), and port did not function.
E. Catheter tip is pulled by Goose neck snare with transfemoral approach.
F. After reposition of catheter tip, port functions well and has been used during 1-year follow-up period.

Table 1
Primary Disease of Patients

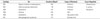
Table 3
Types and Specifications of Ports Used
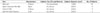
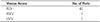
Table 4
Complication Cases
References
1. Reeves AR, Seshadri R, Trerotola SO. Recent trends in central venous catheter placement: a comparison of interventional radiology with other specialties. J Vasc Interv Radiol. 2001; 12:1211–1214.
2. Song WG, Jin GY, Han YM, Yu HC. Central venous catheterization: comparison between interventional radiological procedure and blind surgical procedure. J Korean Radiol Soc. 2002; 47:467–472.
3. Peynircioglu B, Canyigit M, Ergun O, Pamuk GA, Cil BE. Radiologically placed venous ports in children. J Vasc Interv Radiol. 2007; 18:1389–1394.
4. Parker RI, Mahan RA, Giugliano D, Parker MM. Efficacy and safety of intravenous midazolam and ketamine as sedation for therapeutic and diagnostic procedures in children. Pediatrics. 1997; 99:427–431.
5. Krupski G, Fröschle GW, Weh FJ, Schlosser GA. [Central venous access devices in treatment of patients with malignant tumors: venous port, central venous catheter and Hickman catheter. Cost-benefit analysis based on a critical review of the literature, personal experiences with 135 port implantations and patient attitude]. Chirurg. 1995; 66:202–207.
6. Morris SL, Jaques PF, Mauro MA. Radiology-assisted placement of implantable subcutaneous infusion ports for long-term venous access. Radiology. 1992; 184:149–151.
7. Groeger JS, Lucas AB, Thaler HT, Friedlander-Klar H, Brown AE, Kiehn TE, et al. Infectious morbidity associated with long-term use of venous access devices in patients with cancer. Ann Intern Med. 1993; 119:1168–1174.
8. Basford TJ, Poenaru D, Silva M. Comparison of delayed complications of central venous catheters placed surgically or radiologically in pediatric oncology patients. J Pediatr Surg. 2003; 38:788–792.
9. Noh HM, Kaufman JA, Rhea JT, Kim SY, Geller SC, Waltman AC. Cost comparison of radiologic versus surgical placement of long-term hemodialysis catheters. AJR Am J Roentgenol. 1999; 172:673–675.
10. Macdonald S, Watt AJ, McNally D, Edwards RD, Moss JG. Comparison of technical success and outcome of tunneled catheters inserted via the jugular and subclavian approaches. J Vasc Interv Radiol. 2000; 11(2 Pt 1):225–231.
11. Trerotola SO, Kuhn-Fulton J, Johnson MS, Shah H, Ambrosius WT, Kneebone PH. Tunneled infusion catheters: increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology. 2000; 217:89–93.
12. Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994; 331:1735–1738.
13. Cimochowski GE, Worley E, Rutherford WE, Sartain J, Blondin J, Harter H. Superiority of the internal jugular over the subclavian access for temporary dialysis. Nephron. 1990; 54:154–161.
14. Shin BS, Ahn M. Implantable central venous chemoport: comparision of results according to approach routes and methods. J Korean Radiol Soc. 2003; 49:165–171.
15. Crowley JJ, Pereira JK, Harris LS, Becker CJ. Radiologic placement of long-term subcutaneous venous access ports in children. AJR Am J Roentgenol. 1998; 171:257–260.
16. Green SM, Li J. Ketamine in adults: what emergency physicians need to know about patient selection and emergence reactions. Acad Emerg Med. 2000; 7:278–281.
17. Green SM, Clark R, Hostetler MA, Cohen M, Carlson D, Rothrock SG. Inadvertent ketamine overdose in children: clinical manifestations and outcome. Ann Emerg Med. 1999; 34(4 Pt 1):492–497.
18. Fu ES, Miguel R, Scharf JE. Preemptive ketamine decreases postoperative narcotic requirements in patients undergoing abdominal surgery. Anesth Analg. 1997; 84:1086–1090.
19. Roytblat L, Korotkoruchko A, Katz J, Glazer M, Greemberg L, Fisher A. Postoperative pain: the effect of low-dose ketamine in addition to general anesthesia. Anesth Analg. 1993; 77:1161–1165.
20. Miqdady MI, Hayajneh WA, Abdelhadi R, Gilger MA. Ketamine and midazolam sedation for pediatric gastrointestinal endoscopy in the Arab world. World J Gastroenterol. 2011; 17:3630–3635.
21. Cil BE. Radiological placement of chest ports in pediatric oncology patients. Eur Radiol. 2004; 14:2015–2019.
22. Lorenz JM, Funaki B, Van Ha T, Leef JA. Radiologic placement of implantable chest ports in pediatric patients. AJR Am J Roentgenol. 2001; 176:991–994.
23. Nosher JL, Bodner LJ, Ettinger LJ, Siegel RL, Gribbin C, Asch J, et al. Radiologic placement of a low profile implantable venous access port in a pediatric population. Cardiovasc Intervent Radiol. 2001; 24:395–399.
24. Munro FD, Gillett PM, Wratten JC, Shaw MP, Thomas A, MacKinlay GA, et al. Totally implantable central venous access devices for paediatric oncology patients. Med Pediatr Oncol. 1999; 33:377–381.
25. Ross MN, Haase GM, Poole MA, Burrington JD, Odom LF. Comparison of totally implanted reservoirs with external catheters as venous access devices in pediatric oncologic patients. Surg Gynecol Obstet. 1988; 167:141–144.
26. Dillon PA, Foglia RP. Complications associated with an implantable vascular access device. J Pediatr Surg. 2006; 41:1582–1587.
27. Lorch H, Zwaan M, Kagel C, Weiss HD. Central venous access ports placed by interventional radiologists: experience with 125 consecutive patients. Cardiovasc Intervent Radiol. 2001; 24:180–184.
28. Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M. ESPEN. ESPEN Guidelines on Parenteral Nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28:365–377.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download