Abstract
Purpose
To determine the frequency and clinical significance of a small amount of isolated pelvic free fluid found at follow-up multidetector-row computed tomography (MDCT) in male patients who have undergone a curative surgery for gastric carcinoma.
Materials and Methods
From January 2005 to June 2010, 1680 male patients were enrolled in this retrospective study that underwent a follow-up MDCT at least 6 months after a curative surgery for gastric carcinoma. The mean follow-up duration was 41 months. The computed tomographic assessment included the detection of ascites, any possible cause, volume and attenuation measurement and the determination of the location.
Results
Of 1680 patients, 83 (4.9%) patients had ascites. Isolated ascites was identified in 66 patients (3.9%). All ascites were located below or at the level of the second sacral vertebral body. The mean volume and mean attenuation of isolated pelvic free fluid were 2.3 ± 1.9 mL and 9.8 ± 4.7 Hounsfield units. During the follow-up period, none of the 66 patients showed signs of peritoneal recurrence.
Gastric carcinoma is one of the most common tumors worldwide and is the second most common cause for cancer related death in the world (1). A complete resection of the gastric tumor and regional lymph nodes offers the only chance of cure (2). Although a tumor recurrence after the surgery has a poor prognosis, an early identification is helpful because it potentially allows patients with minimal adenopathy or small recurrent masses to better respond to chemotherapy (2). The multidetector-row computed tomography (MDCT) has emerged as the imaging modality of choice in the evaluation of postoperative complications before performing a radiologic intervention and in determining the presence of recurrent tumors after gastrectomy for gastric carcinoma (2, 3). Ascites is one of the most common computed tomography (CT) findings suggestive of peritoneal carcinomatosis along with peritoneal thickening, nodularity and contrast enhancement after intravenous contrast material administration (4, 5, 6, 7). Furthermore, an ascites can be the only CT finding of peritoneal carcinomatosis if peritoneal metastatic implants are too small and the peritoneal reaction is minimal. A small amount of isolated pelvic free fluid in a female patient of reproductive age is often attributed to physiologic fluid (8, 9, 10, 11). In contrast, a small amount of pelvic free fluid in male patients should not be regarded as just physiologic fluid, especially in those who have undergone a cancer surgery. There have been previous reports on the clinical significance of small amounts of ascites detected with preoperative CT in patients with gastric carcinoma (12). However, to our knowledge, there is no report on the incidence and clinical significance of a small amount of ascites detected with follow-up CT after a curative surgery for a gastric carcinoma. Therefore, the purpose of this study was to retrospectively determine the frequency and clinical significance of a small amount of isolated pelvic free fluid at follow-up MDCT in male patients who have undergone curative surgery for gastric carcinoma.
This retrospective study was approved by the Institutional Review Board of our institute and the requirement for an informed patient consent was waived. The review of the medical image database and radiologic reports of our institution revealed 1680 male patients that were regularly followed up by MDCT at an interval of at least 6 months after a curative surgery for a gastric carcinoma from January 2005 to June 2010. We automatically retrieved the words "ascites or fluid" from the CT reports of the 1680 male patients and then reviewed the selected CT images. The mean age of the 1680 patients was 66.1 years old (age range 23-89 years). The distribution of postoperative pathologic stages according to the seventh edition of the American Joint Committee on Cancer TNM classification system was as follows: stage 0 = 5.1% (n = 86); stage IA = 53.3% (n = 895); stage IB = 16.8% (n = 282); stage II = 12.4% (n = 208); stage IIIA = 8.9% (n = 150); and stage IIIB = 3.5% (n = 59).
In our institution, gastric carcinoma patients are regularly followed after curative surgery using MDCT with a six-month interval follow-up for two postoperative years and thereafter with an annual follow-up for three years.
All CT scans were performed by using a 16 channel multi-detector helical CT scanner (Lightspeed16; GE Healthcare, Milwaukee, WI, USA). For contrast-enhanced CT, a dose of 2 mg/kg of a non-ionic contrast agent (Ultravist 370; Bayer, Berlin, Germany) was intravenously administrated at a flow rate of 3 mL/sec using a power injector. Imaging was conducted as determined from the dome of the diaphragm to the pubic symphysis during the portal venous phase with bolus tracking and automated triggering technology. The protocol was as follows: 120 kVp; autoregulated mA; sections = 16; section thickness = 5.0 mm; pitch = 0.938:1; table speed = 18.75 mm per rotation and gantry speed = 0.8 seconds per rotation. The transverse section data were reconstructed with 5 mm thick sections at 5 mm intervals in the transverse plane. Coronal reformatted images were reconstructed with 3 mm sections at 3 mm intervals. The 5 mm transverse and 3 mm coronal images were reconstructed at the operator's console and transferred to a picture archiving and communication system (PACS) workstation (INFINITT PACS, Infinitt Co., Ltd., Seoul, Korea) as a separate series of scans for interpretation.
All CT images in this study were retrospectively and individually analyzed by two experienced abdominal radiologists at PACS workstations. Discrepancies in individual interpretations were resolved by consensus. The readers were notified of the study design but blinded to the final outcomes of patients.
'Small amount' was defined as when the volume of ascites was estimated to be less than 20 mL using volumetric evaluation. 'Isolated' was defined as when there were no identifiable causes of ascites. 'Pelvic free fluid' was defined as ascites identified below or at the level of the second sacral body upper margin.
The readers evaluated images according to 1) the presence or absence of ascites, 2) any potential causes of the ascites including peritoneal carcinomatosis, liver cirrhosis, chronic renal failure, congestive heart failure, and 3) other organ metastasis. If the readers detected pelvic free fluid, they evaluated additional information as follows: 1) measurement of the volume, 2) measurement of the attenuation, and 3) determination of the location (below or at the level of the sacral vertebral body). Volume measurement was performed by using regions of interest from the PACS, delineating the entire margins of the fluid, adding the number of areas and multiplying the sum of the areas by a section thickness of 0.5 cm. For measurement of fluid attenuation, the possible large cursor was placed in the center of the middle section of the fluid to obtain the Hounsfield units (HU) (Figs. 1, 2).
We reviewed the electric medical records and the next follow-up MDCT images (duration range = 12-48 months; mean duration = 22.5 months) to determine the outcomes of patients. A recurrence of gastric carcinoma was validated by serial imaging study follow-ups with an 1 year interval at minimum. Tumor recurrence was determined by following imaging findings; 1) metastases of organ or lymph nodes, 2) peritoneal carcinomatosis such as nodular thickening and enhancement of peritoneum or omental cake.
Ascites was identified in 83 (4.9%) of the 1680 patients. Of them, 10 patients had a malignant disease as follows; peritoneal carcinomatosis with apparent peritoneal thickening (n = 5), metastatic disease in organs other than the peritoneum (n = 3), and newly developed primary cancers in other organs during the follow-up period (n = 2). In seven patients were potential causes identified as follows; liver cirrhosis (n = 4), history of early postoperative intraperitoneal chemotherapy (n = 2), and chronic renal failure (n = 1). Therefore, an isolated ascites was found in 66 (3.9%) patients (mean age = 63.3 years; age range = 34-78 years). And all isolated ascites met the requirement of the 'small amount of pelvic free fluid'. The mean volume was 2.3 ± 1.9 mL and the mean attenuation of the small amount of isolated pelvic free fluid was 9.8 ± 4.7 HU at the portal venous phase imaging. The fluid was located below or at the level of second sacral vertebral body in 12.1% (8 of 66) of patients, below or at the level of the third sacral body upper margin in 53.0% (35 of 66) and below or at the level of the forth sacral body upper margin in 34.8% (23 of 66) of the patients. We retrospectively reviewed the medical records and the next follow-up CTs in 66 patients. The mean follow-up period after surgery was 41 months (duration range = 18-72 months) and the mean follow-up period after isolated pelvic fluid initially detected by CT was 22.5 months (duration range = 12-48 months). In only 2 of 66 (3.0%) patients, the recurrence of gastric carcinoma was diagnosed on CT scans after 12 months of follow-up, equivalent to isolated lymph node metastasis and lymph nodes and pulmonary metastasis. In recurred cases, the isolated pelvic fluid had persisted in one case only. The remaining 64 of the 66 (86.0%) patients showed no sign of recurrence on their follow-up CT scans. There was no significant difference in the volume, attenuation and location of the pelvic free fluid between the two groups with or without tumor recurrence (Table 1). Isolated pelvic fluid was reduced or completely resolved in 55 of the 64 patients and was persisted or slightly increased in other 9 patients at the last follow CT scan.
CT scan has been established as the most useful modality to detect tumor recurrence in postoperative gastric carcinoma (2, 3). Specifically, follow-up CT scans can detect all recurrences of early gastric carcinoma, so regular follow-up abdominal CT examinations are useful (13). Even contrast enhanced abdominal CT scans are more sensitive to the detection of malignant peritoneal involvement than positron emission tomography/CT (PET/CT) scans (14, 15). The most common CT evidence of recurrent tumor is regional or retroperitoneal lymph node metastasis, followed by peritoneal seeding, local recurrence and remote metastasis (3). Peritoneal implants, ascites, mesenteric implants and omental involvement are common CT findings suggestive of peritoneal carcinomatosis (4, 5, 6, 7).
However, although ascites has been regarded an important finding suggesting peritoneal carcinomatosis, the meaning of ascites may become ambiguous, because the CT detects subtle amounts of peritoneal fluid collection with increased sensitivity (12). In addition, the peritoneal cavity physiologically contains a small amount of serous fluid which has been produced by permeable mesothelium, although this diffusely disperses in the peritoneal cavity and is not usually detected by a CT (12). And as we already know, a small amount of isolated pelvic free fluid can be detected in female patients of reproductive age and it is often attributed to physiologic fluid (8, 9, 10, 11). In addition, recently, Yu et al. (16) reported that 49 of 1000 men with blunt trauma had a small amount of pelvic fluid without an identifiable cause.
Therefore, the clinical management of patients with a small amount of pelvic free fluid not accompanying other causes or signs suggestive of malignant seeding is not straightforward, while the presence of a moderate or large amount of ascites with peritoneal nodularity, thickening or omental mass is a strong indicator of peritoneal carcinomatosis.
In our study, most patients (97.0%, 64/66) with a small amount of isolated pelvic free fluid had no tumor recurrence and only 2 patients (3.0%, 2/66) had tumor recurrence in the follow-up period. In addition, there was no malignant involvement of the peritoneum in the two recurrence cases.
Although, our follow-up duration after gastrectomy was less than 5 years and it was not pathologically confirmed that the small amount of isolated pelvic free fluid is not malignant ascites, there was no other sign suggestive of malignant seeding, such as peritoneal thickening or nodularity in the next follow-up CT at least 1 year later (duration range = 12-48 months; mean duration = 22.5 months). Therefore, based on our findings, a small amount of isolated free pelvic fluid should not be considered as an early indicator of peritoneal carcinomatosis.
Consequently, radiologists do not need to warn physicians on the probability of peritoneal seeding and the physicians don't have to consider anymore additional CT scans at shorter follow-up periods, PET/CT scans or ascites cytology.
There are two limitations to our study. First, the recurrence of gastric carcinoma was not validated by a pathologic diagnosis. However, untreated peritoneal carcinomatosis rapidly progresses and develops obvious signs of peritoneal carcinomatosis on short term follow-up images. Also all patients with a small amount of isolated pelvic free fluid were followed for more than one year and there were no suggestive signs of peritoneal carcinomatosis. Second, we didn't review all CT images of 1680 male patients and automatically retrieved the words "ascites or fluid" from the radiologic reports. But for the past few decades, our radiologist thoroughly and carefully evaluated the presence of ascites on the postoperative follow-up CTs of gastric cancer patients because ascites is one of the most common CT findings suggestive of peritoneal carcinomatosis and can be considered as the only CT finding of peritoneal carcinomatosis.
In conclusion, the presence of ascites likely has no clinical importance, if it is small in amount, equal in attenuation to simple fluid and located in the deep region of the pelvis in patients who have undergone gastrectomy for gastric carcinoma.
Figures and Tables
Fig. 1
Axial contrast-enhanced CT image of lower part of pelvis in 69-year-old man after gastrectomy with no evidence of tumor recurrence shows small amount of pelvic free fluid in presacral area (arrows), with attenuation of 11.0 Hounsfield units.
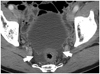
Fig. 2
Coronal contrast-enhanced CT image of lower part of pelvis in 68-year-old man after gastrectomy with no evidence of tumor recurrence shows small amount of pelvic free fluid (arrow) in deep pelvis with attenuation of 13 Hounsfield units.

References
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008; 58:71–96.
2. Kim KW, Choi BI, Han JK, Kim TK, Kim AY, Lee HJ, et al. Postoperative anatomic and pathologic findings at CT following gastrectomy. Radiographics. 2002; 22:323–336.
3. Yoo SY, Kim KW, Han JK, Kim AY, Lee HJ, Choi BI. Helical CT of postoperative patients with gastric carcinoma: value in evaluating surgical complications and tumor recurrence. Abdom Imaging. 2003; 28:617–623.
4. Raptopoulos V, Gourtsoyiannis N. Peritoneal carcinomatosis. Eur Radiol. 2001; 11:2195–2206.
5. Suleiman AJ, Uraiqat NA, Al-Imam OA, Khuliefat SM, Al-Sakran M. Peritoneal carcinomatosis computerized tomography scans findings and causes. JRMS. 2004; 11:63–66.
6. Walkey MM, Friedman AC, Sohotra P, Radecki PD. CT manifestations of peritoneal carcinomatosis. AJR Am J Roentgenol. 1988; 150:1035–1041.
7. Lee HJ, Kim MJ, Lim JS, Kim KW. Follow up CT findings of various types of recurrence after curative gastric surgery. J Korean Radiol Soc. 2007; 57:553–562.
8. Davis JA, Gosink BB. Fluid in the female pelvis: cyclic patterns. J Ultrasound Med. 1986; 5:75–79.
9. Donnez J, Langerock S, Thomas K. Peritoneal fluid volume and 17 beta-estradiol and progesterone concentrations in ovulatory, anovulatory, and postmenopausal women. Obstet Gynecol. 1982; 59:687–692.
10. Takeuchi M, Matsuzaki K, Nishitani H. Manifestations of the female reproductive organs on MR images: changes induced by various physiologic states. Radiographics. 2010; 30:1147.
11. Nance FC. Diseases of the peritoneum, retroperitoneum, mesentery, and omentum. In : Haubrich WS, Schaffner F, Berk JE, editors. Bockus Gastroenterology. 5th ed. Philadelphia: W.B Saunders;1995. p. 3061–3096.
12. Chang DK, Kim JW, Kim BK, Lee KL, Song CS, Han JK, et al. Clinical significance of CT-defined minimal ascites in patients with gastric cancer. World J Gastroenterol. 2005; 11:6587–6592.
13. Ma H, Lee SJ, Kim SA, Lim HK, No JH, Son TS, et al. Usefulness of follow-up computed tomography after surgery for early gastric cancer. J Korean Radiol Soc. 2002; 47:513–518.
14. Kim DW, Park SA, Kim CG. Detecting the recurrence of gastric cancer after curative resection: comparison of FDG PET/CT and contrast-enhanced abdominal CT. J Korean Med Sci. 2011; 26:875–880.
15. Dromain C, Leboulleux S, Auperin A, Goere D, Malka D, Lumbroso J, et al. Staging of peritoneal carcinomatosis: enhanced CT vs. PET/CT. Abdom Imaging. 2008; 33:87–93.
16. Yu J, Fulcher AS, Wang DB, Turner MA, Ha JD, McCulloch M, et al. Frequency and importance of small amount of isolated pelvic free fluid detected with multidetector CT in male patients with blunt trauma. Radiology. 2010; 256:799–805.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download