INTRODUCTION
The development of metastatic disease from a primary tumor has a major impact on prognosis of the patient. The lungs are the most common site of metastatic disease, as the pulmonary metastases develop at some point in the disease process in approximately 20-50% of the cancer patients (1). Pulmonary metastasectomy has been performed for the past decades, and many studies have reported that it is an effective treatment associated with improved survival. In recent years, pulmonary metastasectomy has become the standard therapy for various types of metastatic tumor in the lungs (2, 3, 4, 5).
There have been a few studies on the prognostic factors that improve the patients' survival after a pulmonary metastasectomy from osteosarcoma. Despite the notion that the pulmonary metastasectomy can improve survival in patients with pulmonary metastases, there are currently no guidelines established to optimize the patients' selection for pulmonary metastasectomy.
The aim of this study was to evaluate the clinical characteristics and chest computed tomography (CT) images of the patients who underwent pulmonary metastasectomy from osteosarcoma, and to identify the prognostic factors associated with the improved survival.
MATERIALS AND METHODS
Patients
We reviewed all surgical files of osteosarcoma patients who underwent surgical removal of pulmonary metastatic nodules at our institution from October 1999 to October 2008. To be considered for pulmonary metastasectomy, all patients had to meet the following criteria: 1) regional control of primary osteosarcoma was obtained, 2) pulmonary lesions were considered resectable by radiologic examinations, 3) curative resection was possible, and 4) metastatic disease was absent in other organs. A total of 59 patients met these criteria. The Institutional Review Board approved our retrospective study with the waiver of informed consent, but the written informed consent from all patients was acquired for the CT study.
Image Acquisition and Analysis
CT scans were obtained using the helical technique; a 4-detector scanner (Volume Zoom, Siemens Medical Solutions, Er-langen, Germany) was used for 36 patients, and a 64-detector scanner (Brilliance 190P, Philips Healthcare, Amsterdam, The Netherlands) was used for 23 patients. The scanning was performed from the level of the thoracic inlet to the level of the middle portion of the kidneys. The unenhanced scans were obtained from 10 patients, and the enhanced scans were obtained from 49 patients. In all of the patients, the scanning parameters were 120 kVp and 270-400 mA, and a reconstruction interval of 1-5.0 mm was used.
Two radiologists with 3 and 9 years of experience on chest CT interpretation, retrospectively assessed the CT scans. The decisions on CT findings were reached by consensus. The CT scans were assessed in terms of the maximum diameter of largest pulmonary metastatic nodule, location (unilobe/multilobe), laterality (unilateral/bilateral), and number of metastatic nodules.
The mean duration of CT follow-ups for the patients was 52 months (range, 26-113 months). The serial CT scans were available for all patients, from the time of the original diagnosis of primary osteosarcoma until the occurrence of pulmonary metastases. The mean follow-up interval was 3 months (range, 1-6 months) in the first year and 7 months (range, 3-12 months) after that.
Statistical Analyses
Statistical analyses were performed using statistical software (STATA version 11.2, StataCorp LP, College Station, TX, USA). Survival time was calculated from the date of pulmonary metastasectomy to the date of death. The death notices were obtained from the charts of the patients who had died or via telephone interviews with the patients' family members. The differences in patients' prognoses for 5-year survival were compared in terms of age, sex, location of the primary osteosarcoma, disease-free interval (DFI) from the date of primary surgery to the date of pulmonary metastases on CT, maximum diameter of largest pulmonary metastatic nodule, laterality (unilateral/bilateral), and location of pulmonary metastatic nodule(s). The log-rank test was used for univariate analyses (p < 0.05) and the Cox proportional hazards model was used for multivariate analyses (p < 0.05).
RESULTS
Patient Group
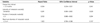
The clinical and imaging variables of the included patients with pulmonary metastases from osteosarcoma are summarized in Table 1. The study group included 38 male and 21 female patients with a median age of 16 years (mean age, 22 years; range, 8-72).
The locations of primary tumors were femur in 34 cases, radius in 1 case, pelvis in 6 cases, tibia in 13 cases, and humerus in 5 cases. The primary tumors were completely resected in all the cases, and the median DFI was 12 months (range, 0-114). Bilateral or multilobar pulmonary metastases were more common than unilateral or unilobar pulmonary metastases. The mean number of metastatic nodule(s) was 3.23 (range, 1-9), and the mean maximum diameter was 15.61 mm (range, 2-61 mm). Wedge-resections were the most common procedures. In 2 of 59 cases, a lobectomy was performed because of the size and central location of the tumor.
Survival and Outcome
The 5-year survival rate after the pulmonary metastasectomy from osteosarcoma was 33.89%. The univariate analyses (Table 2) showed that the following were significant prognostic factors affecting the 5-year survival: the DFI > 12 months (p = 0.0392), the measurement of the maximum diameter of metastatic nodule ≤ 2 cm (p = 0.0112), and the number of metastatic nodules ≤ 3 (p = 0.0217). Other factors including age, sex, location of the primary osteosarcoma, nodule laterality (unilateral/bilateral), and nodule location (unilobar/multilobar) (p > 0.05) were nonsignificant prognostic factors. The multivariate analyses (Table 3) revealed that the DFI > 12 months [p = 0.041, hazard ratio = 0.504, 95% confidence interval (CI) = 0.254-1.001] and the nodule unilaterality (p = 0.029, hazard ratio = 0.291, 95% CI = 0.0961-0.883) were the independent prognostic factors affecting the 5-year survival (Fig. 1). Other factors including age, sex, location of the primary osteosarcoma, the measurement of the maximum diameter of metastatic nodule ≤ 2 cm, the number of metastatic nodules ≤ 3, and location (unilobar/multilobar) of the metastatic nodules (p > 0.05) were not independent prognostic factors (Fig. 2).
The DFI > 12 months was the only significant prognostic factor for the 5-year survival according to both univariate and multivariate analyses. The laterality (unilateral) of metastatic nodule(s) was not a significant prognostic factor for the 5-year survival, according to univariate analysis, but it was an independent prognostic factor according to multivariate analysis.
DISCUSSION
Osteosarcoma is the second most common primary malignant bone tumor, and it is mostly common in children and adolescents. The 5-year survival of patients with osteosarcoma has dramatically improved over the last two decades, because of the adjuvant and neoadjuvant chemotherapy and surgical resections (6, 7). The 5-year survival of osteosarcoma patients without lung metastases has thereby increased to 77% (8). Nevertheless, approximately 50% of the osteosarcoma patients develop metastatic lung disease, and 30-50% of the osteosarcoma patients died from the pulmonary metastases (6, 9, 10). In the previous reports, the 5-year survival rate after pulmonary metastasectomy from osrapteosarcoma was 30-40%. The 5-year survival rate in our study was 33.89%, which is similar to the previous reports (11, 12, 13, 14, 15, 16, 17, 18, 19, 20).
It is recently accepted that when the metastatic disease is limited to the lungs, pulmonary metastasectomy can improve the prognosis of patients with osteosarcoma (1, 3, 4, 9, 12, 15). However, there have been some debates concerning the prognostic factors for improvement in survival, for the patients who undergo pulmonary metastasectomy from osteosarcoma.
Several studies have shown that the DFI, number of metastatic nodules, and maximum diameter of metastatic nodule were statistically significant prognostic factors of pulmonary metastasectomy from osteosarcoma (16, 17, 18, 19, 20). In our study, univariate analyses showed that a DFI > 12 months, maximum diameter of metastatic nodule(s) ≤ 2 cm, and number of metastatic nodules ≤ 3 were significant prognostic factors affecting 5-year survival. On the other hand, multivariate analyses showed that DFI > 12 months and the laterality (unilateral) of metastatic nodule(s) were independent prognostic factors of survival.
Although previous studies have not established a DFI cut-off period, a shorter DFI is associated with a lower 5-year survival after pulmonary metastasectomy from osteosarcoma. In some studies, a DFI < 12 months carries a worse prognosis, but others have found a cut-off at 18 or 24 months to be significant (16, 17, 18). In our study, there were more consistent differences in the 5-year survival, shown by univariate analysis, between using a DFI cut-off at 24 months (p = 0.0084) and using a DFI cut-off at 12 months (p = 0.0392); we adopted the cut-off at 12 months for DFI. In addition, DFI > 12 months was an independent prognostic factor for 5-year survival on multivariate analysis.
Regarding the number of metastatic nodules, some studies have shown that the solitary lesions indicate a better prognosis. In other studies, a total of 3 to 4 metastases was more favorable than 5 metastases (17, 18, 19). In our study, there was a significant difference in 5-year survival when using a cut-off of 3 metastatic nodules (p = 0.0217), but there was no significant difference when using a cut-off of 2 metastatic nodules (p = 0.0712), according to the univariate analysis. However, the number of metastatic nodules ≤ 3 was not an independent prognostic factor for 5-year survival according to the multivariate analysis.
With regard to the maximum diameter of metastatic nodule(s), some studies have shown that nodules ≤ 2 cm in diameter have a better prognosis (16, 20). In our study, there was also a significant difference in the 5-year survival for patients with a maximum diameter of metastatic nodule ≤ 2 cm (p = 0.0112) on univariate analysis. However, this was not an independent prognostic factor for 5-year survival according to the multivariate analysis.
We found that the prognostic factors associated with the improved survival after pulmonary metastasectomy from osteosarcoma were the DFI > 12 months and the nodule unilaterality. The longer DFI was generally considered to indicate a favorable prognosis after pulmonary metastasectomy, and our study confirmed this association. On the other hand, our multivariate analysis revealed that the nodule unilaterality was also an independent prognostic factor. In comparison with the overall 5-year survival rate of 33.89%, the 5-year survival rate for patients with a DFI > 12 months or nodule unilaterality was 44.11% and 39.28%, respectively. Moreover, the 5-year survival rate for patients with both the DFI > 12 months and the nodule unilaterality increased to 52.63% (Fig. 3). Other factors, including age, sex, and the location of primary osteosarcoma, were nonsignificant prognostic factors affecting 5-year survival according to univariate and multivariate analyses.
Our study had several limitations. First, this was a retrospective review. Therefore, a prospective randomized controlled trial is needed to confirm these results. Second, the CT follow-up intervals were not performed consistently among all of the patients. At least during the first year, the CT follow-up interval should be regular and short enough to overcome any measurement error. Third, our sample size was small, so a multi-center study will be needed. Fourth, chemotherapy regimens were not investigated in this study. The chemotherapeutic regimens have evolved rapidly over the past decades and are now highly individualized on the basis of patient status.
In conclusion, pulmonary metastasectomies from primary osteosarcoma were well-performed in our institution. The prognostic factors associated with improved survival were the DFI > 12 months and the unilaterality of the metastatic nodule(s).




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download