Abstract
Extramedullary plasmacytoma (EMP) is defined as extra-osseous proliferation of neoplastic plasma cells in multiple myeloma (MM). A 55-year-old man presented with painless swelling of his left testis. Chest imaging showed plaque-like pleural thickening in the right hemithorax, and bone imaging revealed multiple sites of bony involvement. Left orchiectomy and pleural biopsy were performed and the histologic assessment revealed a diagnosis of EMP. Although testes and pleura are rarely involved in MM, the possibility of testicular or pleural EMP should be considered when a patient with MM presents with testicular swelling or a chest imaging abnormality.
Extramedullary plasmacytoma (EMP) is defined as extra-osseous proliferation of neoplastic plasma cells, and it may be primary or secondary to bone marrow involvement in multiple myeloma (MM) (1). The testis and pleura are unusual sites of EMP. Testicular EMP has been reported in 0.6-2.7% of all MM cases (2). According to a review of 958 MM cases, only 0.8% of patients were reported to have myelomatous pleural effusion (3). In a study assessing the clinical correlates and prognostic relevance of EMP in the presence of MM, 42 patients had EMP among 467 patients with MM (4). Of these 42 patients, only 9 patients had pleural or peritoneal EMP at the time of diagnosis and none of the patients had testicular EMP.
Giuliani et al. (5) reported a case of MM with EMP involving the testis and pleura. In their case, testicular mass and myelomatous pleural effusion were not present at the time of initial diagnosis, but they appeared after five cycles of chemotherapy. To the best of our knowledge, there are no case reports of testicular and pleural EMP as the initial presenting clinical features in patients with MM. We report the first case of EMP involving the testis and pleura at the time of initial diagnosis in a patient with MM.
A 55-year-old man presented with painless swelling of his left testis. On testicular ultrasonography (US), the left testis measured 3.3 × 6.7 × 4.5 cm in size and 51.9 cm3 in volume, and showed heterogeneous echogenicity with multiple, ill-defined, hypoechoic foci and hypervascularity, which was suggestive of malignancy (Fig. 1). Chest radiography performed for a preoperative work-up showed increased opacity in the right lower lung zone. Chest CT scans performed for further evaluation showed plaque-like pleural thickening in the right lower posterior hemithorax, which was suggestive of pleural metastasis (Fig. 2). During the diagnostic work-up, the patient also complained of painless scalp swelling. Subsequent skull series revealed multiple, punched-out, radiolucent lesions in the skull. On brain CT scans, osteolytic bony lesions with focal scalp swelling were seen in the left parietal area, which were suggestive of bony metastasis. Whole-body bone scan showed multiple areas of uptake in the skull, right 4th, 9th, and 10th ribs, and right proximal femur, which were suggestive of multiple bony metastases. To confirm the diagnosis and to direct treatment, left orchiectomy and pleural biopsy were performed. The histopathologic specimens obtained from left orchiectomy and pleural biopsy revealed plasma cell infiltration of the interstitium of the testis (Fig. 3) and pleura (Fig. 4), positive immunohistochemical staining for CD79a, Bcl-2, cyclin D1, and lambda, and negative staining for CD30 (Ki-1), kappa, and Ki-67 (30%). Taken together, these findings confirmed the diagnosis of EMP (Fig. 3). Serum and urine protein electrophoresis revealed monoclonal gammopathy with a positive M-spike. Serum and urine immunofixation electrophoresis (IFEP) demonstrated an abnormal band of restriction in the lambda light chain. Bence-Jones lambda chains were detected in the urine. On repeated serum IFEP, monoclonal gammopathy of IgD type was detected. Serum and urine beta-2 microglobulin levels were 4.7 mg/L and 7.00 mg/L, respectively. Bone marrow (BM) aspirate showed a high number of plasma cells (44.6%), and BM biopsy specimen showed compact cellularity (100%) with diffuse plasma cells and scanty normal hematopoietic cells. A final diagnosis of IgD-type MM with EMP involving the testis and pleura was made. The patient achieved a very good partial response after two cycles of high-dose dexamethasone chemotherapy, and two cycles of vincristine, doxorubicin, and dexamethasone chemotherapy; however, the disease relapsed after auto-peripheral blood stem cell transplantation. After the patient received the fifth cycle of chemotherapy with bortezomib and dexamethasone, he had complete remission with negative serum and urine IFEP results.
According to the World Health Organization classification of plasma cell neoplasms, plasmacytoma is classified into solitary plasmacytoma of bone and EMP, which presents as a soft tissue mass without any other evidence of myeloma. Some of the researches have defined EMP as a plasma cell neoplasm of soft tissue with or without MM (3, 4, 6). EMP is defined as extra-osseous proliferation of neoplastic plasma cells, and may be primary or secondary to bone marrow involvement in MM. EMP is rare but most often occurs in the nasopharynx, upper respiratory tract, or gastrointestinal tract. The testis and pleura are unusual sites of EMP (1). Testicular EMP has been reported in 0.6-2.7% of all MM cases (2). According to a review of 958 MM cases, only 0.8% of patients were reported to have myelomatous pleural effusion (3). In a study assessing the clinical correlates and prognostic relevance of EMP in the presence of MM, 42 patients had EMP among 467 patients with MM (4). Of these 42 patients, only 9 patients had pleural or peritoneal EMP at the time of diagnosis and none of the patients had testicular EMP.
The clinical incidence of testicular plasmacytoma is reported to be 0.03% to 0.1% of all primary and secondary tumors of the testes (7). It is well known that testes are rare sites of hematologic malignancy because of the blood-testis barrier. Until 2002, 51 cases of testicular plasmacytoma were reported in the literature, either as the initial presenting symptom or not as the initial presenting symptom (8). In our case, the chief complaint of the patient was testicular enlargement, which proved to be testicular EMP involvement of IgD-type MM. Although our patient had a rare IgD-type MM, the US findings were similar to those of other MM types; an enlarged testicle with poorly circumscribed intra-testicular hypoechoic lesions and increased vascularity (8).
Kintzer et al. (3) reported that only eleven (1%) of 958 MM cases had intrathoracic EMP without bone involvement, and only 0.8% of the patients had myelomatous pleural effusion although the evidence of pleural EMP was unclear among these patients. Most of the pleural manifestations of MM have been reported as myelomatous pleural effusion (3, 9). In a few case reports, the CT findings of pleural EMP included focal pleural thickening or diffuse confluent pleural nodularity mimicking mesothelioma (9). In our case, the patient had plaque-like pleural thickening in the right lower posterior hemithorax on the initial CT scan, which was suggestive of pleural metastasis.
In most of the patients with MM, IgG or IgA are the immunoglobulin types that are reported; whereas in our case, the immunoglobulin type was IgD. IgD MM is a rare form of MM, which comprises 2.1% of all myelomas, is predominant in males, and occurs more frequently in younger people (10). The main characteristics of IgD MM include uncertain appearance of the M-component, dominance of the lambda light chain over the kappa chain in serum electrophoresis, and frequent presence of Bence-Jones proteins in urine. IgD MM has been known to be associated with a higher frequency of renal failure than the other types of myelomas. In our case, the patient did not have any evidence of renal failure although results of all serum and urine studies were consistent with IgD MM.
There is only one case report in the literature of MM synchronously involving the testis and pleura according to Pubmed and Medline databases. Giuliani et al. (5) reported a case of IgG MM presenting with testicular swelling and myelomatous effusion after 5 cycles of chemotherapy. In their case, the pleural involvement in MM was proved by myelomatous pleural effusion without a soft tissue mass; therefore, it was not definitive for EMP. However, in our case, the patient presented with testicular swelling and plaque-like pleural thickening at the time of initial diagnosis of MM. These soft tissues were pathologically confirmed as EMP of the testis and pleura. EMP has been reported to occur before the diagnosis of MM in only 0.4% of patients with MM (6). In addition, among patients with IgD MM, there are a few reports of patients with extraosseous disease (11).
In conclusion, we report a case of IgD-type MM with testicular and pleural EMP at the time of initial diagnosis. We think that this is the first case report of IgD MM with synchronous involvement of the testis and pleura. Although the testis and pleura are rarely involved in MM, the possibility of testicular or pleural EMP should be considered when a patient with MM presents with testicular swelling or a chest imaging abnormality.
Figures and Tables
Fig. 1
A 55-year-old man who presented with painless swelling of the left testis. Gray-scale (A) and color Doppler (B) images of testis ultrasonography shows heterogeneous echogenicity with multiple, ill-defined, hypoechoic foci and hypervascularity in the left testis.

Fig. 2
Chest CT scan shows plaque-like pleural thickening in the right lower posterior hemithorax (arrows).
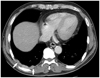
Fig. 3
A 55-year-old man who underwent left orchiectomy.
A. Photograph of surgical specimen obtained from left orchiectomy shows no definite nodular or mass-like lesion in testis.
B. Photomicrograph of surgical specimen obtained from left orchiectomy shows relatively uniform plasma cells with eccentrically located nuclei and the residual seminiferous tubules separated by heavy infiltrates of plasma cells (H&E, × 400).
C, D. Immunohistochemical stains of surgical specimen obtained from left orchiectomy show positive reaction for cytoplasmic lambda light chain in plasma cells (× 400) (C), and negative reaction for kappa light chain in plasma cells (× 400) (D).

References
1. Moulopoulos LA, Granfield CA, Dimopoulos MA, Kim EE, Alexanian R, Libshitz HI. Extraosseous multiple myeloma: imaging features. AJR Am J Roentgenol. 1993; 161:1083–1087.
2. Chica G, Johnson DE, Ayala AG. Plasmacytoma of testis presenting as primary testicular tumor. Urology. 1978; 11:90–92.
3. Kintzer JS Jr, Rosenow EC 3rd, Kyle RA. Thoracic and pulmonary abnormalities in multiple myeloma. A review of 958 cases. Arch Intern Med. 1978; 138:727–773.
4. Chen HF, Wu TQ, Li ZY, Shen HS, Tang JQ, Fu WJ, et al. Extramedullary plasmacytoma in the presence of multiple myeloma: clinical correlates and prognostic relevance. Onco Targets Ther. 2012; 5:329–334.
5. Giuliani N, Caramatti C, Roti G, Geata A, Colla S, Bonomini S, et al. Hematologic malignancies with extramedullary spread of disease. Case 1. Multiple myeloma with extramedullary involvement of the pleura and testes. J Clin Oncol. 2003; 21:1887–1888.
6. Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003; 78:21–33.
7. Hayes DW, Bennett WA, Heck FJ. Extramedullary lesions in multiple myeloma; review of literature and pathologic studies. AMA Arch Pathol. 1952; 53:262–272.
8. Anghel G, Petti N, Remotti D, Ruscio C, Blandino F, Majolino I. Testicular plasmacytoma: report of a case and review of the literature. Am J Hematol. 2002; 71:98–104.
9. Kim YJ, Kim SJ, Min K, Kim HY, Kim HJ, Lee YK, et al. Multiple myeloma with myelomatous pleural effusion: a case report and review of the literature. Acta Haematol. 2008; 120:108–111.
10. Cabrera A, Klein JS. Bilateral pleural masses and shortness of breath associated with multiple myeloma. Chest. 1997; 111:1750–1753.
11. Jancelewicz Z, Takatsuki K, Sugai S, Pruzanski W. IgD multiple myeloma. Review of 133 cases. Arch Intern Med. 1975; 135:87–93.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download