Abstract
Nodular fasciitis, a benign soft tissue tumor consisting of myofibroblastic proliferation, is commonly located in the subcutaneous or inter- or intra-muscular layer of extremites. Intra-articular nodular fasciitis is extremely rare. We report a case of MRI findings of a nodular fasciitis in the knee of a 13-year-old boy which was removed by arthroscopic surgery and pathologically confirmed.
Intra-articular tumors or tumor-like lesions, occasionally encountered in the locomotor system, often include a variety of synovial proliferative disease, infectious granulomatous disease, benign and malignant tumors such as pigmented villonodular synovitis (PVNS), synovial hemangioma, lipoma arborescens, tuberculous arthritis, rheumatoid arthritis, and synovial sarcoma (1). Intra-articular nodular fasciitis is extremely rare. Nodular fasciitis is a benign soft tissue lesion consisting of myofibroblastic proliferation. Nodular fasciitis is usually self-limiting and arising most commonly in the subcutaneous and fascial tissues (2). Here we describe a rare case of intra-articular nodular fasciitis of the knee.
A 13-year-old boy presented with left knee pain and tenderness for 3 months. He had an uncertain history of knee sprain 3 months ago. After the knee sprain incident, his symptoms had been gradually worsened. The patient visited a private orthopedic surgery clinic and underwent knee joint aspiration several times. However, the symptoms did not improve. After undergoing a magnetic resonance imaging (MRI) at a local radiological clinic, the patient was referred to the orthopedic department at our hospital. Physical examination revealed a palpable tender mass in the anterior knee, medial to the patella. Range of motion of the joint was slightly restricted in the flexion. There was no instability of the joint or sign of meniscal tear. Radiographs of the knee showed no abnormality. MRI of the knee showed a solitary well defined mass-like lesion (measuring 2 × 2 cm) which was located intra-articularly along the joint capsule inferomedial aspect to the patella. The lesion was iso- to slightly hyper-intense compared to that of adjacent normal muscle on T1-weighted images and hyper-intense on fast spin echo on gradient T2-weighted images. Area of low signal intensity suggesting collagen-rich stroma was observed in ventral aspect of the mass. Joint effusion was evident on T2-weighted images (Fig. 1). Contrast enhancement study was not included.
Pre-operative radiological impression was intra-articular benign solid mass. At arthroscopy, a white, well-defined and encapsulated mass was attached to the joint capsule in the inferomedial aspect in the knee joint. The mass was excised arthroscopically. Histopathological examination revealed spindle-shaped myofibroblastic cell proliferation in a variably collagenous or myxoid stroma. Nuclear atypia or mitotic figures were absent. Based on immunohistochemical study, spindle cells were diffusely positive for a-smooth-muscle actin but negative for desmin. These histological features were consistent with those of nodular fasciitis (Fig. 2).
Nodular fasciitis is a benign self-limiting reactive process most commonly encountered in the subcutaneous fascial soft tissues of the extremities of adults between 20 and 40 years of age (3). Intra-articular occurrence of nodular fasciitis is extremely rare, especially in pediatric patients. To the best of our knowledge, a search of the English literature revealed only a few case reports of intra-articular nodular fasciitis (3, 4, 5, 6, 7). In pediatric patients, a few cases have been reported only in the ankle, knee, and glenohumeral joint (3, 4, 5).
Histologically, nodular fasciitis is composed of plump, immature-appearing fibroblasts and myofibroblasts in irregular fascicles, regardless of whether they are predominantly fibrous or myxoid. In general, these cells differ little in size with oval shape of pale stained nuclei and prominent nucleoli. Mitotic figures are fairly common. However, atypical mitoses are virtually never seen. Immunohistochemically, the cells stain positively for smooth-muscle actin but negatively for desmin, suggesting a smooth-muscle cell differentiation (2). In the present case, histological findings and immunohistochemical staining properties were consistent with typical nodular fasciitis.
Clinically, extra-articular nodular fasciitis commonly presents as a rapidly growing painful mass in the subcutaneous fascia (2). However, intra-articular nodular fasciitis grows relatively slow, with a longer preoperative history in a report (3). Patients with intra-articular nodular fasciitis typically complain of pain, swelling, restriction of joint motion, and a palpable mass around the joint (2, 3, 7). The pathogenesis of nodular fasciitis is currently unclear. Some described that nodular fasciitis was a reactive lesion related to trauma, others suggested that nodular fasciitis had chromosomal abnormalities of neoplastic origin (3).
MRI findings of extra-articular nodular fasciitis are nonspecific, with iso- to slightly hyper-intense signal intensity on T1-weighted images and hyper-intense signal intensity on T2-weighted images. Inhomogenous enhancement is common (8, 9). Surrounding edema, trans-compartmental spread and osseous changes are also reported (8).
Although information on imaging studies for intra-articular nodular fasciitis is limited, the current case showed nonspecific findings on MRI images, with homogeneous iso to low signal intensity on T1-weighted images and a heterogeneous, low to high signal intensity on T2-weighted images as reported previously (3, 4, 5, 6, 7). In this present case, conventional MRI with no contrast study showed nonspecific signal intensity of the lesion similar to previous reports, resulting in difficulty in making a precise pre-operative diagnosis on MRI. Differential diagnoses include PVNS, synovial hemangioma, lipoma arborescens, rheumatoid arthritis, and infectious granulomatous disease such as tuberculous arthritis (1, 10).
This report has several limitations. Firstly, imaging sequences were not fully performed in every cross-sectional plane. Secondly, additional imaging study such as ultrasound or follow-up MRI was not performed.
In conclusion, extremely rare intra-articular nodular fasciitis may be included to the list of differential diagnosis of intra-articular tumor or tumor-like lesions, although its MRI findings are nonspecific.
Figures and Tables
Fig. 1
Magnetic resonance imaging in a 13-year-old man with intra-articular nodular fasciitis of left knee.
A. Fast spin echo axial T2-weighted image shows a well defined mass (arrowheads) with a increased signal intensity compared to normal muscle. Area of low signal intensity suggesting collagen-rich stroma is seen in ventral aspect of the mass. This mass is located in the joint capsule of inferomedial aspect of patella. Joint effusion is also noted.
B. Sagittal T1-weighted image reveals iso- to slightly high signal intensity to the normal muscle.
C. Gradient coronal T2-weighted image demonstrates well defined homogeneous high signal intensity.
D. Coronal T1-weighted image also shows well defined iso- to slightly high signal intensity of the mass.
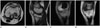
Fig. 2
Pathologic images of the intra-articular nodular fasciitis.
A. Microphotograph shows myofibroblastic cell proliferation in the subsynovial layer (H&E; × 40).
B. Mixed collagenous and myxoid stroma is seen (H&E; × 100).
C. Immunohistochemical staining shows a positive reaction with a-smooth-muscle actin (× 200).

References
1. Sheldon PJ, Forrester DM, Learch TJ. Imaging of intraarticular masses. Radiographics. 2005; 25:105–119.
2. Weiss Sw, Goldblum Jr. Enzinger and Weiss's soft tissue tumors. 5th ed. St. Louis: Mosby;2008. p. 190–194.
3. Hornick JL, Fletcher CD. Intraarticular nodular fasciitis--a rare lesion: clinicopathologic analysis of a series. Am J Surg Pathol. 2006; 30:237–241.
4. Lädermann A, Kindynis P, Taylor S, Ceroni D, Hoffmeyer P, Kaelin A, et al. Articular nodular fasciitis in the glenohumeral joint. Skeletal Radiol. 2008; 37:663–666.
5. Gans I, Morrison MJ 3rd, Chikwava KR, Wells L. Intra-articular nodular fasciitis of the knee in a pediatric patient. Orthopedics. 2014; 37:e313–e316.
6. Matsuzaki T, Akisue T, Kishimoto K, Kishimoto S, Imabori M, Hara H, et al. Intra-articular nodular fasciitis of the knee: a rare cause of recurrent hemarthrosis. Rheumatol Int. 2012; 32:1691–1694.
7. Hagino T, Ochiai S, Sato E, Watanabe Y, Senga S, Kondo T, et al. Intraarticular nodular fasciitis causing limitation of knee extension: a case report. Knee. 2010; 17:424–427.
8. Coyle J, White LM, Dickson B, Ferguson P, Wunder J, Naraghi A. MRI characteristics of nodular fasciitis of the musculoskeletal system. Skeletal Radiol. 2013; 42:975–982.
9. Leung LY, Shu SJ, Chan AC, Chan MK, Chan CH. Nodular fasciitis: MRI appearance and literature review. Skeletal Radiol. 2002; 31:9–13.
10. Botez P, Sirbu PD, Grierosu C, Mihailescu D, Savin L, Scarlat MM. Adult multifocal pigmented villonodular synovitis--clinical review. Int Orthop. 2013; 37:729–733.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download