Abstract
Variceal bleeding is an unusual complication of ileal conduits. We report a case in which recurrent stomal variceal hemorrhage from an ileal conduit for bladder cancer was successfully treated by percutaneous transhepatic obliteration (PTO) using microcoils and N-butyl cyanoacrylate. Therefore, PTO can be one treatment option to prevent recurrent stomal variceal bleeding from ileal conduits.
The term "ectopic varix" is used to describe a dilated portosystemic collateral vein occurring anywhere in the abdomen except the gastroesophageal region. Ectopic varices account for up to 5% of all variceal bleeding (1). Stomal varices are rare and different from other ectopic varices in terms of clinical presentation, severity, and their management. Several treatments have been reported for stomal variceal bleeding, including local therapy such as epinephrine-soaked gauze, pressure dressings, suture ligation, refashioning the stoma, and portosystemic procedures such as transjugular intrahepatic portosystemic shunts (TIPS) or liver transplantation (1, 2). Percutaneous transhepatic obliteration (PTO) is another option for treating this serious condition (3). Here, we report a case of an 82-year-old man who had an ileal conduit placed for previous cystectomy due to bladder cancer. He presented stomal variceal hemorrhage that was successfully treated by PTO using microcoils and N-butyl cyanoacrylate (NBCA).
An 82-year-old man with liver cirrhosis was admitted to our institution due to recurrent intermittent stomal site bleeding. The patient underwent radical cystectomy with ileal conduit placement for bladder cancer 20 years ago. Recurrent stomal site bleeding from the ileal conduit occurred for 8 months, which required transfusion at several occasions. The patient underwent suture ligation at a local hospital but was transferred to our institution due to recurrent bleeding. Contrast-enhanced computed tomography (CT) demonstrated dilated mesenteric varices communicating with the stomal site and draining into the femoral vein through the abdominal wall collaterals (Fig. 1A). On admission, his pulse was regular at 54/min, temperature was normal, and blood pressure was 117/65 mm Hg. Laboratory testing revealed a hemoglobin value of 9.6 g/dL. Ultrasonography-guided left portal vein puncture was performed. After 6-Fr sheath placement, a portogram was obtained. The portogram revealed hepatofugal blood flow and engorgement of the mesenteric vein that communicated with the ileal conduit.
A 5-Fr David catheter (Cook, Bloomington, IN, USA) was placed in the superior mesenteric vein. A coaxial 3-Fr microcatheter (MicroFerret; Cook) was advanced into the feeders of the stomal varices (Fig. 1B). To avoid NBCA migration to the porta vein, embolization was performed with two microcoils (interlock detachable coil; Boston Scientific Corp., Natick, MA, USA) of 8 mm × 20 cm and 6 mm × 20 cm in size. Embolization with NBCA (Grelan Pharmaceutical, Tokyo, Japan)/iodized oil mixture at 1:2 volume ratio was additionally employed after coil placements. Portogram after embolization demonstrated complete obliteration of the stomal varices (Fig. 1C). The percutaneous transhepatic tract was also embolized with the NBCA/iodized oil mixture at 1:2 volume ratio.
There were no acute complication within 48 hours following the procedure. Currently, at 7 months after embolization, the patient remained well without stomal varix bleeding recurrence (Fig. 1D).
Stomal varices are ectopic varices commonly encountered in patients who have undergone colectomy with ileostomy for the management of inflammatory bowel disease. Stomal varices are less frequently found in patients with ileal conduits for urinary diversion (1). Stomal varices were first described by Resnick et al. (4) in 1968 with a reported incidence of up to 27% in patients with chronic liver failure and permanent stoma. The pathogenesis of this lesion has been attributed to the development of postsurgical anastomoses between the high-pressure portal system and the low-pressure venous system of the abdominal wall which permits the development of an abundant conglomeration of mucocutaneous varices at the stomal site. The time for variceal development and subsequent hemorrhage reportedly ranging from 1.5 months to 29 years is probably governed by the rate of progression of the underlying liver disease (5). The risk of death from a stomal bleeding incident is estimated to be 3-4% (1). This is considerably less than the 30-40% mortality associated with acute gastroesophageal variceal hemorrhage. This could be due to the fact that stomal bleeding patients are usually aware of the bleeding early in its clinical course or that they were taught how to control the hemorrhage with pressure.
There exists no clear consensus regarding the optimal treatment for stomal bleeding. Treatment options range from local measures such as pressure dressings, suture ligation, beta blockade, and injection sclerotherapy to more invasive surgical interventions, including stomal revision, portosystemic shunts, and liver transplantation (1, 2).
As an initial measure, application of pressure on the stoma, including local pressure, positioning of the patient, suturing, or cautery is effective. However, such measure rarely achieves long-term control (1). Sclerotherapy of the stoma has been reported as effective method in controlling the bleeding acutely. However, due to several fatal complications (6), sclerotherapy is no longer recommended.
Carrafiello et al. (2) reported a 71-year-old male with a stomal varix from an ileal conduit was treated by TIPS. TIPS is an attractive alternative treatment for stomal varices because it has the advantage of decreasing portal pressure. Although TIPS seems to be a safe and effective treatment for stomal varices, about 25% of patients experienced re-bleeding with a patent TIPS despite the fact that the portosystemic pressure gradient had been reduced to less than 12 mm Hg (7). These data suggest that the threshold portal pressure gradient leading to a bleeding stomal varix may be lower than that for esophageal or gastric varices. Therefore, the risk of developing encephalopathy and hepatic decompensation after TIPS might increase. Parvinian et al. (8) reported that older patient age was associated with early mortality in patients with intermediate-risk Model for End-stage Liver Disease scores undergoing TIPS. Specifically, mortality in patients ≥ 55 years old was significantly higher than in patients aged ≤ 54 years old. Thus, TIPS was not considered as a treatment option in our patient who was 82 year old. Instead, we performed PTO and observed no re-bleeding throughout 3 months of follow-up.
In 1989, Samaraweera et al. (9) first reported 4 patients (3 patients with ileostomies and a patient with ileal conduit) underwent PTO as a treatment option for stomal variceal bleeding. They were worried about the risks of surgical shunt and underwent embolization of their varices without complications. Two cases of PTO for treating ileal conduit stomal varices have been reported (3, 9). One patient embolized with coil and gelfoam had recurrent bleeding after 5 months. The other patient treated with thrombin-soaked coils and a sclerosing agent exhibited no further bleeding episodes after 8 months of follow-up. PTO can be combined with other treatment. Han et al. (10) reported one patient with enterostomy site variceal bleeding treated with the combination of TIPS and coil embolization. We employed coils and additional permanent embolic NBCAs using microcatheters threaded through the coils. No bleeding was identified at 7 months follow-up in this patient, although a longer-term follow-up will be conducted. Tract bleeding could be an issue when PTO was performed. However, we embolized the tract with NBCA which was effective in preventing tract bleeding.
In conclusion, PTO can be one treatment option to prevent recurrent stomal variceal bleeding. PTO is a safe approach for older patients.
Figures and Tables
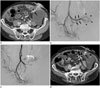 | Fig. 1Radiography of an 82-year-old man who had recurrent stomal variceal hemorrhage from an ileal conduit that was treated with percutaneous transhepatic obliteration.
A. Axial CT scan revealed tortuous and dilated mesenteric varices (arrows) at the stomal site.
B. Percutaneous transhepatic portography demonstrated mesenteric varices (arrows) and stomal varices (arrowheads).
C. After percutaneous transhepatic obliteration using microcoils and N-butyl cyanoacrylate, the stomal varices were no longer visualized.
D. Axial CT scan, obtained 7 months later, revealed no bleeding recurrence (arrows).
|
References
1. Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998; 28:1154–1158.
2. Carrafiello G, Laganà D, Giorgianni A, Lumia D, Mangini M, Paragone E, et al. Bleeding from peristomal varices in a cirrhotic patient with ileal conduit: treatment with transjugular intrahepatic portocaval shunt (TIPS). Emerg Radiol. 2007; 13:341–343.
3. Lashley DB, Saxon RR, Fuchs EF, Chin DH, Lowe BA. Bleeding ileal conduit stomal varices: diagnosis and management using transjugular transhepatic angiography and embolization. Urology. 1997; 50:612–614.
4. Resnick RH, Ishihara A, Chalmers TC, Schimmel EM. A controlled trial of colon bypass in chronic hepatic encephalopathy. Gastroenterology. 1968; 54:1057–1069.
5. Goldstein MB, Brandt LJ, Bernstein LH, Sprayragen S. Hemorrhage from ileal varices: a delayed complication after total proctocolectomy in a patient with ulcerative colitis and cirrhosis. Am J Gastroenterol. 1983; 78:351–354.
6. Wolfsen HC, Kozarek RA, Bredfeldt JE, Fenster LF, Brubacher LL. The role of endoscopic injection sclerotherapy in the management of bleeding peristomal varices. Gastrointest Endosc. 1990; 36:472–474.
7. Vidal V, Joly L, Perreault P, Bouchard L, Lafortune M, Pomier-Layrargues G. Usefulness of transjugular intrahepatic portosystemic shunt in the management of bleeding ectopic varices in cirrhotic patients. Cardiovasc Intervent Radiol. 2006; 29:216–219.
8. Parvinian A, Shah KD, Couture PM, Minocha J, Knuttinen MG, Bui JT, et al. Older patient age may predict early mortality after transjugular intrahepatic portosystemic shunt creation in individuals at intermediate risk. J Vasc Interv Radiol. 2013; 24:941–946.
9. Samaraweera RN, Feldman L, Widrich WC, Waltman A, Steinberg F, Greenfield A, et al. Stomal varices: percutaneous transhepatic embolization. Radiology. 1989; 170(3 Pt 1):779–782.
10. Han SG, Han KJ, Cho HG, Gham CW, Choi CH, Hwang SY, et al. A case of successful treatment of stomal variceal bleeding with transjugular intrahepatic portosystemic shunt and coil embolization. J Korean Med Sci. 2007; 22:583–587.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download