Abstract
One common complication after major pancreatic surgery is bleeding. Herein we describe a case of pancreatic pseudoaneurysm which developed after pylorous preserving pancreaticoduodenectomy for common bile duct cancer. Three attempts of transcatheter embolization failed since feeders to the pseudoaneurysm had unfavorable anatomy. Direct percutaneous N-butyl cyanoacrylate injection was performed under fluoroscopy-guidance and the pseudoaneurysm was successfully treated. Percutaneous fluoroscopy-guided direct N-butyl cyanoacrylate injection may be a useful alternative when selective transcatheter embolization fails or is technically challenging.
Hemorrhage after pancreatic surgery is not an uncommon complication. Among them, a ruptured pseudoaneurysm is a life-threatening complication, necessitating urgent intervention (1). Radiologic intervention such as transcatheter embolization is a useful tool to treat gastrointestinal bleeding, aneurysms, and pseudoaneurysms of the visceral arteries. We herein describe a case of a pancreatic pseudoaneurysm which developed after pylorous preserving pancreaticoduodenectomy (PPPD) that was treated successfully via direct percutaneous N-butyl cyanoacrylate (NBCA) injection after failing selective transcatheter embolization.
This case report met the requirement of the Institutional Review Board. A 61-year-old male patient presented with epigastric pain and dyspepsia. On an abdominal CT scan, a mass lesion was found in the common bile duct, and it was confirmed as adenocarcinoma on the following endoscopic retrograde cholangiopancreatography with cytology and biopsy. After admission, he underwent PPPD without immediate complication. However, the fluid from the drainage tube became bloody four days after the surgery, and a follow-up CT scan revealed a 5.0-mm pseudoaneurysm at the distal portion of the dorsal pancreatic artery and an associated 10.0 × 8.0-cm hematoma between the pancreas and the stomach. His hemoglobin level decreased from 11.8 g/dL to 9.0 g/dL between the first and fourth days after the surgery. The clinician decided to manage this pseudoaneurysm conservatively, given its relatively small size and the patient's stable hemodynamics. A percutaneous drainage catheter was inserted to evacuate the hematoma. However, a follow-up CT scan, taken 12 days after the initial CT scan, revealed that the pseudoaneurysm became more prominent in size and its degree enhanced (Fig. 1).
Subsequently, endovascular treatment was attempted. The celiac angiography demonstrated the pseudoaneurysm at the dorsal pancreatic artery (Fig. 2A). Selective angiography of the dorsal pancreatic artery revealed multiple fine vessels communicating with the pseudoaneurysm (Fig. 2B). Embolization was attempted with a 1:3 mixture of NBCA and iodized oil, however, the NBCA mixture only filled some of the fine pancreatic arteries before reaching the pseudoaneurysm. We thought that the microcatheter was located just in front of the pseudoaneurysm based on the anteroposterior projection image, however, it turned out that the tip of the microcatheter was actually apart from the pseudoaneurysm. Splenic angiography showed persistent pseudoaneurysm supplied by the fine pancreatic arteries arising from the splenic artery. Catheterization of those fine pancreatic arteries arising from the splenic artery was unsuccessful due to their small sizes. A second attempt was made on the following day. Splenic and superior mesenteric angiographies showed the persistent pseudoaneurysm supplied by fine pancreatic arteries arising from the splenic and superior mesenteric arteries. However, the second attempt resulted in failure for the same reason.
After the failed attempts at transcatheter embolization, the patient was managed conservatively and underwent another follow-up CT scan seven days later. The size of the pseudoaneurysm increased to 9.0-mm, necessitating repeated endovascular treatment. Superior mesenteric angiography revealed a feeder of the pseudoaneurysm. Nonetheless, selection of the feeder with a micro-wire and a microcatheter was technically demanding because of the tortuosity and acute angulation of the feeder vessel (Fig. 3).
As an alternative, we decided to perform direct percutaneous NBCA injection. Under fluoroscopic guidance, a 21-guage Chiba needle (Cook, Bloomington, IN, USA) was advanced into the pseudoaneurysm sac. Pulsatile blood was regurged through the needle and contrast media was also injected through this needle to confirm that the needle tip was located within the pseudoaneurysm. A 1:3 mixture of NBCA and iodized oil was injected as an embolic material (Fig. 4). A post-procedural fluoroscopic image showed compact filling of the pseudoaneurysm with the glue mixture. The patient did not experience any complications and his hemoglobin and pancreatic enzyme level were stable after the procedure. A subsequent CT scan taken seven days after the procedure revealed successful embolization of the pseudoaneurysm (Fig. 5) and the patient was discharged one week later. The patient underwent intermittent chemoradiotherapy and abdominal CT scan during the 18 months follow-up period; the CT scans showed no recurrence of pseudoaneurysm.
Prior to the advent of interventional radiologic equipment and techniques, surgical hemostasis had been recognized as the treatment of choice for pseudoaneurysms which developed after pancreatic surgery. However, surgical exploration is often technically challenging because of factors such as tissue adhesion and rebleeding vulnerability of the affected arteries. Accordingly, compared with endovascular treatment surgical hemostasis has leads to longer hospital stays and a higher overall mortality rate (2). Nowadays, surgical treatment is hence generally reserved for those cases where bleeding focuses cannot be identified by angiography or when endovascular treatment does not seem to be promising due to vascular anatomy or other technical difficulties (3).
Selective arterial embolization has been considered to be the most appropriate therapy in the treatment of visceral pseudoaneurysm, with a success rate greater than 80% and a low complication rate (4). Various embolic materials have successfully been used, including NBCA, microcoils, gelatin sponge particles, ethanol, polyvinyl alcohol, and thrombin.
N-butyl cyanoacrylate is an efficient and permanent embolic agent which has been successfully for decades. Since this material polymerizes immediately in blood providing instant vessel occlusion, iodized oil is mixed to delay polymerization and to provide radioopacity. However, longer polymerization time increases the risk of distal embolization, requiring considerable experience to achieve optimal results. In addition to the ratio of iodized oil to NBCA, flow dynamics of the target vessel must be carefully analyzed considering the sizes of the vessel itself and collateral channels (5). In this case, the pseudoaneurysm had contact with several pancreatic arteries, which produced significant back flow, hindering the spread of the NBCA mixture into the pseudoaneurysm. If a microcatheter had been placed just in front of the pseudoaneurysm, transcatheter embolization might have been successful. After initial embolization through the dorsal pancreatic artery, the pseudoaneurysm was supplied by fine pancreatic arteries arising from the splenic and superior mesenteric arteries, which made transcatheter embolization even more difficult.
As with our case, achieving selective endovascular access to the affected artery can be technically challenging due to vasospasm or unfavorable vascular anatomy such as tortuosity, length, and acute angulation. For those cases, percutaneous fluoroscopy guided embolization might be an alternative method before considering surgical treatment. A direct percutaneous approach was first described by Cope and Zeit (6) in 1986 for the treatment of the common iliac artery aneurysm. Several study groups reported their experience of direct percutaneous embolization for the treatment of splanchnic aneurysms and pseudoaneurysms (7, 8). In this case, the size of the pseudoaneurysm was too small to be well visualized on ultrasonography. Thus, we performed the direct puncture of the pseudoaneurysm with fluoroscopic guidance. The major complication of percutaneous direct NBCA injection is distal embolization (9). Injection of NBCA at the periphery away from the neck of pseudoanuerysm can reduce the risk and one study group introduced assistance with balloon occlusion of the parent artery (10).
In conclusion, direct percutaneous injection of NBCA into a pancreatic pseudoaneurysm may be a useful alternative method when selective transcatheter embolization fails or is technically challenging.
Figures and Tables
Fig. 1
The contrast-enhanced abdominal CT scan (arterial phase) taken 16 days after pylorous preserving pancreaticoduodenectomy for common bile duct cancer shows a 6.2-mm pseudoaneurysm (arrow). The extent of hematoma between the pancreas and the stomach (arrowhead) was slightly decreased after insertion of a drainage catheter (not shown).
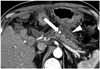
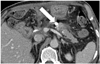
Fig. 2
Angiography was performed 16 days after pylorous preserving pancreaticoduodenectomy.
A. Celiac angiography shows a pseudoaneurysm at the dorsal pancreatic artery (arrow).
B. Selective angiography of the dorsal pancreatic artery demonstrates the pseudoaneurysm (arrow) connected with several small pancreatic branches.

Fig. 3
The 3rd trial of transcatheter embolization was performed 24 days after pylorous preserving pancreaticoduodenectomy.
A. Superior mesenteric angiography at the second attempt reveals a feeding vessel to the pseudoaneurysm (arrow).
B. Selective angiography of the pancreaticoduodenal artery from the superior mesenteric artery shows that the feeding vessel of the pseudoaneurysm (arrow) is very tortuous and angulated.

Fig. 4
Percutaneous fluoroscopy-guided direct N-butyl cyanoacrylate injection was performed 24 days after pylorous preserving pancreaticoduodenectomy.
A. Direct percutaneous puncture of the pseudoaneurysm (arrow) was carried out under fluoroscopic guidance.
B. The post-procedural fluoroscopic image shows compact filling of N-butyl cyanoacrylate in the pseudoaneurysm (arrow) as well as vessels (arrowheads) connected with the pseudoaneurysm.

References
1. Ding X, Zhu J, Zhu M, Li C, Jian W, Jiang J, et al. Therapeutic management of hemorrhage from visceral artery pseudoaneurysms after pancreatic surgery. J Gastrointest Surg. 2011; 15:1417–1425.
2. Bergert H, Dobrowolski F, Caffier S, Bloomenthal A, Hinterseher I, Saeger HD. Prevalence and treatment of bleeding complications in chronic pancreatitis. Langenbecks Arch Surg. 2004; 389:504–510.
3. Schäfer M, Heinrich S, Pfammatter T, Clavien PA. Management of delayed major visceral arterial bleeding after pancreatic surgery. HPB (Oxford). 2011; 13:132–138.
4. Otah E, Cushin BJ, Rozenblit GN, Neff R, Otah KE, Cooperman AM. Visceral artery pseudoaneurysms following pancreatoduodenectomy. Arch Surg. 2002; 137:55–59.
5. Vyas S, Ahuja CK, Yadav TD, Khandelwal N. Emergency ultrasound-guided percutaneous embolization of post-traumatic bleeding hepatic artery pseudoaneurysms. Minim Invasive Ther Allied Technol. 2012; 21:372–376.
6. Cope C, Zeit R. Coagulation of aneurysms by direct percutaneous thrombin injection. AJR Am J Roentgenol. 1986; 147:383–387.
7. Araoz PA, Andrews JC. Direct percutaneous embolization of visceral artery aneurysms: techniques and pitfalls. J Vasc Interv Radiol. 2000; 11:1195–1200.
8. Ghassemi A, Javit D, Dillon EH. Thrombin injection of a pancreaticoduodenal artery pseudoaneurysm after failed attempts at transcatheter embolization. J Vasc Surg. 2006; 43:618–622.
9. Aytekin C, Firat A, Yildirim E, Kirbas I, Boyvat F. Ultrasound-guided glue injection as alternative treatment of femoral pseudoaneurysms. Cardiovasc Intervent Radiol. 2004; 27:612–615.
10. Gulati GS, Gulati MS, Makharia G, Hatimota P, Saikia N, Paul SB, et al. Percutaneous glue embolization of a visceral artery pseudoaneurysm in a case of sickle cell anemia. Cardiovasc Intervent Radiol. 2006; 29:665–668.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download