Abstract
Extrinsic airway compression due to chest wall deformity is not commonly observed. Although this condition can be diagnosed more easily with the help of multidetector CT, the standard treatment method has not yet been definitely established. We report a case of an eighteen-year-old male who suffered from severe extrinsic tracheal compression due to scoliosis and straightening of the thoracic spine, confirmed on CT and bronchoscopy. The patient underwent successful placement of tracheal stent but later died of bleeding from the tracheostomy site probably due to tracheo-brachiocephalic artery fistula. We describe the CT and bronchoscopic findings of extrinsic airway compression due to chest wall deformity as well as the optimal treatment method, and discuss the possible explanation for bleeding in the patient along with review of the literature.
Although the relationship between development of restrictive lung disease and thoracic deformity such as kyphoscoliosis is well documented with accompanying pulmonary function test results (1), extrinsic tracheal compression due to chest wall deformity is not commonly observed or known to occur. The diagnosis of this condition can be made with the help of multidetector CT (2), but the standard treatment method has not yet been definitely established (3, 4, 5). Both endoscopic management with stent placement and surgery can be performed, but making the decision between the two options may often be difficult. Recently, we experienced a patient with severe extrinsic tracheal compression due to scoliosis and straightening of the thoracic spine who underwent successful placement of tracheal stent but later died of bleeding from the tracheostomy site probably due to tracheo-brachiocephalic artery fistula. We would like to present this case and discuss making treatment decisions based on imaging findings, which we think might be useful in treatment planning for similar cases.
An eighteen-year-old male with a history of congenital cerebral palsy, seizure disorder, and recurrent pneumonia was admitted to our hospital for tracheal stent insertion. He had first visited the emergency department of another hospital three months ago due to fever and signs of upper airway obstruction such as dyspnea and tachypnea. He was intubated for one month but could not be extubated due to respiratory distress, and subsequently he underwent tracheostomy, which only resulted in worsening of respiratory acidosis. Bronchoscopy performed in that hospital revealed eccentric tracheal stenosis, and he was transferred to our hospital for placement of tracheal stent.
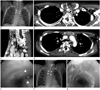
Routine admission tests including complete blood count and blood chemistry showed decreased hemoglobin and hematocrit (8.6 g/dL & 24.8%) and mildly increased C-reactive protein (1.06 mg/dL). On the initial chest radiograph, a segment of distal trachea was not visualized, indicating airway obstruction. Severe scoliosis was also seen (Fig. 1A). Subsequent chest CT examination showed markedly narrowed anteroposterior dimension of the thorax between the upper end of the manubrium and the T3 vertebra, measuring about 1.6 cm, which was significantly smaller than the normal value of 6.2 cm (range 5.0-8.7 cm) (6). Trachea was severely compressed, especially by the right brachiocephalic artery that courses between the manubrium and the vertebral body (Fig. 1B). Straightening of the spine was also seen on the sagittal reconstruction image (Fig. 1C). The lower trachea at the carinal level was also splayed by the T5 vertebra (Fig. 1D). Bronchoscopy also revealed extrinsic tracheal compression (Fig. 1E). Based on these findings, we concluded that the patient was suffering from respiratory failure caused by extrinsic compression of the trachea between the right brachiocephalic artery and the straight thoracic spine. The patient then underwent placement of a tracheal silicone stent by an experienced bronchoscopist, and his symptoms became tolerable afterwards (Fig. 1F, G). However, he suddenly died two weeks later due to massive bleeding of unknown cause from the tracheostomy site.
Abnormalities of the bony thorax can often be an unsuspected and uncommon cause of airway obstruction. These conditions include kyphoscoliosis, pectus excavatum, or straightened thoracic spine, often in conjunction with one another, manifesting in patients with an underlying medical condition such as cerebral palsy or Marfan's syndrome (1). Straightening of the thoracic spine can cause tracheal compression by several mechanisms: trachea could be compressed either directly between the sternum and the vertebral body, by the right brachiocephalic artery crossing the trachea, or by the vertebral bodies splaying the lower trachea at the carina (3), and these findings should be carefully evaluated on axial CT images. Sagittal reconstruction images may be useful in identifying the kyphotic thoracic spine as well as concomitant pectus excavatum, and coronal reconstruction images may be useful in clearly identifying scoliosis.
Treatment of choice for tracheal stenosis has traditionally been open airway reconstruction, but recent studies have shown the usefulness of endoscopic techniques with stent and balloon dilatation (5). Endoscopic techniques are being increasingly used, and successful treatment using a stent has been reported in failed and surgically contraindicated cases (7). Favorable results of stent insertion in congenital tracheal stenosis with vascular sling have also been reported (8).
In our patient, the stent placement was successful without any respiratory problems, but he died later due to sudden bleeding from the tracheostomy site. We suspect that the bleeding may have been due to a tracheo-brachiocephalic artery fistula, a rare but fatal complication after tracheostomy caused by compression injury to the brachiocephalic artery or cuff-induced pressure necrosis of the trachea. Tracheo-brachiocephalic artery fistula is known to occur in 0.6% of patients who undergo tracheostomy within three to four weeks after the procedure, and one of the risk factors for the development of a tracheo-brachiocephalic artery fistula is congenital kyphoscoliosis or thoracic deformity (9). The cause of sudden bleeding in our patient was uncertain as he had not undergone autopsy, but we suspect that either injury to the artery or cuff-induced pressure necrosis, aggravated by the congenital deformity of the spine, may have been the cause for his death.
Surgery has been suggested as the treatment method in few cases of thoracic deformity with tracheal compression. Surgical methods usually include some degree of partial resection of the sternum or manubrium, and suspension, transaction, or reimplantation of the brachiocephalic artery, along with tracheopexy or insertion of reinforcing mesh or plate (3, 4, 10). Surgery may decrease the possibility of development of a tracheo-brachiocephalic artery fistula, but to the best of our knowledge there is no supporting evidence. The incidence of this fistula is very low, and the need for preventive operation in the absence of respiratory problems seems to be controversial.
Surgery for high grade and acquired tracheal stenosis and endoscopic treatment for low grade and congenital tracheal stenosis are the generally accepted treatment methods (5). In our patient, endoscopic treatment seemed to be suitable for tracheal stenosis, but the accompanying thoracic deformity still caused severe compression of the trachea. In retrospect, the correction of thoracic deformity to obviate the extrinsic cause of tracheal compression may have been more useful than placement of tracheal stent alone.
Treatment of tracheal stenosis is highly individualized, and therefore, a thorough image analysis of the trachea and neighboring structures with CT is mandatory for selecting the optimal treatment option. Radiologists should keep in mind the possibility of extrinsic tracheal compression when treating patients suffering from respiratory failure, and if extrinsic tracheal compression is present, they should carefully analyze the neighboring structures to help the clinicians make optimal treatment decisions and warn them about possible complications such as tracheo-brachiocephalic artery fistula.
Figures and Tables
Fig. 1
18-year-old male with intractable respiratory distress.
A. Initial chest radiograph at our hospital shows severe scoliosis and nonvisualization of a segment of distal trachea (arrowheads) caudal to the intubation tube. The carina can still be seen.
B. Axial contrast-enhanced CT image at the level of T3 vertebra and upper end of sternal manubrium shows markedly narrowed mediastinal space and resultant extrinsic compression of the trachea (arrowhead) especially by the brachiocephalic artery (arrow) that courses between the manubrium and the vertebral body.
C. Sagittal reconstructed CT image clearly demonstrates the straightened thoracic spine and extremely narrow space between the sternal manubrium and T3 vertebra. Note how brachiocephalic artery (arrow) also contributes to the compression of the trachea in between.
D. Axial contrast-enhanced CT image at the level of T5 vertebra shows splaying of the lower trachea by the vertebral body.
E. Bronchoscopy before the tracheal stent placement shows the extrinsic compression of the distal trachea, especially on the right side (arrowheads).
F. Chest radiograph after the placement of the silicone stent shows the stent just above the carina, maintaining patency (arrowheads).
G. Bronchoscopy performed four days after the stent insertion shows well-placed silicone stent inside the distal trachea.
Note.-L = left
References
1. Donnelly LF, Bisset GS 3rd. Airway compression in children with abnormal thoracic configuration. Radiology. 1998; 206:323–326.
2. Karoll M, Hernandez RJ, Wessel HU. Computed tomography diagnosis of bronchial compression by the spine after surgical correction of scoliosis. Pediatr Radiol. 1984; 14:335–336.
3. Grillo HC, Wright CD, Dartevelle PG, Wain JC, Murakami S. Tracheal compression caused by straight back syndrome, chest wall deformity, and anterior spinal displacement: techniques for relief. Ann Thorac Surg. 2005; 80:2057–2062.
4. Tatekawa Y, Muraji T. Surgical strategy for acquired tracheomalacia due to innominate artery compression of the trachea. Eur J Cardiothorac Surg. 2011; 39:412–413.
5. Brigger MT, Boseley ME. Management of tracheal stenosis. Curr Opin Otolaryngol Head Neck Surg. 2012; 20:491–496.
6. Keats TE, Sistrom C. Atlas of Radiologic Measurement. 7th ed. St. Louis: Mosby;2001. p. 124–125.
7. Tsakiridis K, Darwiche K, Visouli AN, Zarogoulidis P, Machairiotis N, Christofis C, et al. Management of complex benign post-tracheostomy tracheal stenosis with bronchoscopic insertion of silicon tracheal stents, in patients with failed or contraindicated surgical reconstruction of trachea. J Thorac Dis. 2012; 4:Suppl 1. 32–40.
8. Maeda K, Ono S, Tazuke Y, Baba K. Long-term outcomes of congenital tracheal stenosis treated by metallic airway stenting. J Pediatr Surg. 2013; 48:293–296.
9. Ogawa K, Nitta N, Sonoda A, Takahashi M, Suzuki T, Kitamura S, et al. Tracheo-brachiocephalic artery fistula after tracheostomy associated with thoracic deformity: a case report. J Med Case Rep. 2011; 5:595.
10. Tatekawa Y, Tojo T, Kanehiro H, Nakajima Y. Multistage approach for tracheobronchomalacia caused by a chest deformity in the setting of severe scoliosis. Surg Today. 2007; 37:910–914.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download