Abstract
We describe a case of multiple tuberculous aneurysms of the descending thoracic aorta and abdominal aorta repaired with endovascular stent graft. The case was a 47-year-old man who presented with three saccular pseudoaneurysms of aortoiliac bifurcation at computed tomography (CT) scan. Despite of antimycobacterial treatment, these aneurysms grew rapidly and saccular pseudoaneurysm of the descending thoracic aorta was newly seen. A bifurcated stent graft was successfully implanted in the aortoiliac bifurcation. Subsequently, endovascular stent graft was placed well in the descending thoracic aorta. Fourteen months after the procedure, the patient was stable and serial CT images showed regression of aneurysms with ongoing antimycobacterial treatment. Therefore, endovascular stent graft repair with antimycobacterial therapy may be a treatment option in patients with multiple tuberculous aneurysms.
A tuberculous aortic aneurysm is a rare condition. Multiple tuberculous aneurysms of the aorta are extremely rare and fewer than five cases have been reported (1, 2, 3, 4). If patients with a tuberculous aortic aneurysm are not treated properly, they may die due to aneurysm rupture. In the past, surgery was the standard treatment option for tuberculous aortic aneurysm, but it carries a high risk of mortality and morbidity. Endovascular stent graft is an emerging treatment option for tuberculous aortic aneurysm and can replace surgery in some cases (5, 6, 7). However, no reports of endovascular stent graft repair for multiple tuberculous aneurysms of the aorta are available. Herein, we report a case of successful treatment of multiple tuberculous aneurysms of both the thoracic and abdominal aortas using an endovascular stent graft, combined with antimycobacterial treatment.
A 47-year-old man was admitted to our hospital for further evaluation of persistent fever. He had left buttock abscess, left inguinal lymphadenitis and fever for the past 5 months despite conservative management at another hospital. An ultrasonography-guided gun biopsy from the inguinal lymph node showed a positive result on the Mycobacterium tuberculosis-polymerase chain reaction assay.
Contrast-enhanced pelvic computed tomography (CT) was performed to evaluate the left buttock abscess. The CT showed that the left buttock abscess had almost resolved, but it revealed 22-mm and 7-mm saccular pseudoaneurysms of the infrarenal abdominal aorta and a 27-mm saccular pseudoaneurysm of the right common iliac artery. Despite one month of antimycobacterial treatment, a follow-up CT scan showed that one of the pseudoaneurysms of the infrarenal abdominal aorta had increased in diameter from 22-mm to 34-mm. The CT also revealed a newly developed 7 mm saccular pseudoaneurysm of the descending thoracic aorta (Fig. 1A, B). Because CT scans of the patient had little evidence of active infection such as adjacent soft-tissue mass, fat stranding or fluid in a unusual location, the patient was considered for the endovascular treatment (8).
The patient underwent endovascular repair of the pseudoaneurysms at the aortoiliac bifurcation. A bifurcated stent graft (Medtronic, Minneapolis, MN, USA) was placed without any immediate complication. Completion angiography showed a type II endoleak at the right side of the lower abdominal aorta, although the two pseudoaneurysms of the aortoiliac bifurcation were completely excluded (Fig. 1C). A 1 month follow-up, CT scan demonstrated that the type II endoleak was persistent. Moreover, the pseudoaneurysm of the descending thoracic aorta had increased in diameter from 7-mm to 15-mm.
Transcatheter embolization was performed via the transabdominal approach to repair the endoleak in the lower abdominal aorta (Fig. 2A). The endoleak cavity was directly punctured percutaneously using a 22-gauge needle under fluoroscopic and ultrasound guidance. Then, contrast agent was injected through the puncture needle to evaluate the endoleak cavity and demonstrated that the cavity was supplied from the left fourth lumbar artery. Embolization of the feeding artery was successfully accomplished using a 1:1 mixture of glue and Lipiodol. An endovascular stent graft (Medtronic, Minneapolis, MN, USA) was placed correctly to treat the pseudoaneurysm of the descending thoracic aorta. No immediate complications occurred after the procedure (Fig. 2B).
CT scans at 3 and 8 weeks after the procedure demonstrated that the two stent grafts were placed properly with complete exclusion of the pseudoaneurysms and the endoleak had completely resolved. The patient continued antimycobacterial treatment for 1 year and no longer had a fever 2 months after the procedure. Fourteen months after the procedure, the patient was stable and there was no recurrence on imaging follow-up (Fig. 3).
The incidence of a tuberculous aneurysm of the aorta is very low. About 100 case reports have been published and multiple tuberculous aneurysms of both the thoracic and abdominal aorta are exceptional (1). The natural course of an untreated tuberculous aortic aneurysm is very unfavorable due to aneurysmal rupture and it is not dependent on lesion size. Most tuberculous aneurysms are false, saccular aneurysms and are most common in the thoracic aorta.
Successful treatment of a tuberculous pseudoaneurysm always includes both medical and surgical treatment (9, 10). In one review article, patient mortality increased when treated only by medical or surgical therapy (9). Surgery is part of a standard treatment plan, but it has been associated with a high risk of mortality and morbidity. Therefore, endovascular treatment is considered a current trend and has replaced surgical therapy (5, 6, 7).
Endovascular repair can be the first-line treatment option in selected patients with a tuberculous aortic aneurysm. First, this type of repair should be considered in debilitated patients because of high risk for major complications after surgery. Second, patients with minimally infected tissue would be indicated (8). Third, patients who have limited life expectancy should be considered for palliative treatment (11). Finally, it could also be considered in a patient with a ruptured aneurysm (7).
If active infection or aortoenteric fistula of the patient are evident, there is a high risk for recurrence of infection after the procedure. Therefore, patients who have extensive infection are preferably excluded from endovascular repair. In our case, the endovascular option was considered because the infection was minimal and localized on the CT scan, and the general condition of our patient was relatively stable.
Continued antimycobacterial therapy is required with endovascular treatment. Antituberculous drugs after surgery should be continued from 9 to 12 months, furthermore some advocates indefinite use of antituberculous drugs (1). Therefore, antimycobacterial therapy after endovascular treatment should be continued at least 9 months.
Less than five cases of multiple tuberculous aortic aneurysms have been reported (1, 2, 3, 4). Surgical treatment was performed in three reports and a 16-year-old girl was treated with a multi-layered stent. However, no reports are available on multiple tuberculous aneurysms of both thoracic and abdominal aorta treated with an endovascular stent graft.
In summary, endovascular stent graft repair was successful in a patient with multiple aneurysms of the descending thoracic and abdominal aorta as well as the right common iliac artery. No recurrence was evident 14 months after the procedure.
Figures and Tables
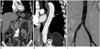 | Fig. 1A 47-year-old man with multiple tuberculous aneurysms of the descending thoracic aorta and abdominal aorta.
A, B. Pre-procedural computed tomography images demonstrated three saccular pseudoaneurysms of the aortoiliac bifurcation (arrows, A) and one saccular pseudoaneurysm of the descending thoracic aorta (arrow, B).
C. Completion angiography after stent graft insertion in the aortoiliac bifurcation showed that the stent graft was well placed and pseudoaneurysms of the aortoiliac bifurcation were completely excluded.
|
 | Fig. 2Treatment of endoleak and pseudoaneurysm of thoracic aorta.
A. One month after the procedure, type II endoleak was persistently seen. Direct puncture of the endoleak sac was performed via transabdominal approach. Angiography through the endoleak sac demonstrated the endoleak sac communicating with the left fourth lumbar artery.
B. After stent graft insertion in the descending thoracic aorta, completion angiography demonstrated that the stent graft was placed correctly in the descending thoracic aorta.
|
References
1. Pierret C, Tourtier JP, Grand B, Boddaert G, Laurian C, de Kerangal X. Multiple tuberculous aneurysms of the aorta. J Vasc Surg. 2011; 53:1720–1722.
2. Strnad BT, McGraw JK, Heatwole EV, Clark P. Tuberculous aneurysm of the aorta presenting with uncontrolled hypertension. J Vasc Interv Radiol. 2001; 12:521–523.
3. Mechchat A, Idrissi R, El Mahi O, Lekehal B, Sefiani Y, Mesnaoui A, et al. [Multiple tuberculous aortic aneurysms in a child. A case report]. J Mal Vasc. 2008; 33:218–220.
4. Benjelloun A, Henry M, Ghannam A, Vaislic C, Azzouzi A, Maazouzi W, et al. Endovascular treatment of a tuberculous thoracoabdominal aneurysm with the Multilayer stent. J Endovasc Ther. 2012; 19:115–120.
5. Clough RE, Topple JA, Zayed HA, Lyons OT, Carrell TW, Taylor PR. Endovascular repair of a tuberculous mycotic thoracic aortic aneurysm with a custom-made device. J Vasc Surg. 2010; 51:1272–1275.
6. Han DK, Chung C, Walkup MH, Faries PL, Marin ML, Ellozy SH. Endovascular stent-graft repair of a tuberculous mycotic aortic aneurysm. Ann Vasc Surg. 2011; 25:699.e13–699.e16.
7. Liu WC, Kwak BK, Kim KN, Kim SY, Woo JJ, Chung DJ, et al. Tuberculous aneurysm of the abdominal aorta: endovascular repair using stent grafts in two cases. Korean J Radiol. 2000; 1:215–218.
8. Lee KH, Won JY, Lee do Y, Choi D, Shim WH, Chang BC, et al. Stent-graft treatment of infected aortic and arterial aneurysms. J Endovasc Ther. 2006; 13:338–345.
9. Long R, Guzman R, Greenberg H, Safneck J, Hershfield E. Tuberculous mycotic aneurysm of the aorta: review of published medical and surgical experience. Chest. 1999; 115:522–531.
10. Park SC, Moon IS, Koh YB. Tuberculous pseudoaneurysm of the descending thoracic aorta. Ann Vasc Surg. 2010; 24:417.e11–417.e13.
11. Steichen O, Pellerin O, Frank M, Emmerich J, Sapoval M, Fiessinger JN, et al. [Endovascular repair of a tuberculous aortic false aneurysm]. Rev Med Interne. 2007; 28:196–198.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download