Abstract
Purpose
To evaluate the usefulness of Hounsfield unit (HU) measurements for diagnosing of congenital cholesteatoma.
Materials and Methods
A total of 43 patients who underwent surgery due to middle ear cavity lesions were enrolled. Twenty-one patients were confirmed to have congenital cholesteatoma by histopathological results and the other 22 patients were confirmed to have otitis media (OM) by operation. Their computed tomography images were retrospectively reviewed. We measured HU of the soft tissue mass in the middle ear cavity. In addition, we evaluated the largest diameter and location of the mass, the presence of bony erosion in the ear ossicle, and the status of the tympanic membrane in the cholesteatoma group.
Results
The mean HU was 37.36 ± 6.11 (range, 27.5-52.5) in the congenital cholesteatoma group and 76.09 ± 8.74 (range, 58.5-96) in the OM group (p < 0.001). The cut-off value was 55.5. The most common location for congenital cholesteatoma was the mesotympanum, and ear ossicle erosion was present in 24%. All patients had an intact tympanic membrane.
Congenital cholesteatoma appears as a whitish mass in the middle ear with an intact tympanic membrane in children, and it is a rare disease accounting for approximately 2% of all cholesteatoma cases (1).
Both computed tomography (CT) and magnetic resonance imaging (MRI) are used in the diagnosis of cholesteatoma and MR diffusion weight imaging or delayed enhancement imaging are evaluated for the differential diagnosis (2, 3). However, the cost of MRI scans is high and contrast media has complications such as allergic reaction and anaphylactic shock. In addition, CT is superior to MRI for delineating fine bone structure. Therefore, temporal bone CT is the imaging technique of choice for clinically suspected cholesteatoma. Although temporal bone CT has high sensitivity of detection, its specificity is low because it is not a contrast-enhanced image, and occasionally the findings are similar to those of granulation tissue, secretions, cholesterol granuloma, or neoplasm, particularly when the lesion is not accompanied by changes in bone (4). Congenital cholesteatoma requires a complete resection to prevent recurrence, whereas treatment for cholesterol granuloma or secretions is marsupialization (5, 6). Therefore, the preoperative diagnosis of cholesteatoma is important.
According to a recent study (7), Hounsfield unit (HU) measurements may aid in the diagnosis of cholesteatoma. Cholesteatoma can be divided into congenital and acquired types, which differ in their location, clinical history, and the status of the tympanic membrane but are indistinguishable histologically (4). Therefore, we hypothesized that the HU measurement in temporal bone CT would be useful for diagnosing congenital cholesteatoma.
The Institutional Review Board approved this retrospective study and waived informed consent.
Among the patients who underwent temporal bone CT between September 2010 and December 2012, 43 who underwent surgery due to middle ear cavity lesions were enrolled. Twenty-one patients were confirmed to have congenital cholesteatoma by histopathological results and the other 22 patients were confirmed to have otitis media (OM) by operation.
Twenty-one patients in the congenital cholesteatoma group were consistent with the diagnostic criteria suggested by Levenson et al. (8), including the following: 1) a whitish mass in the middle ear cavity with a normal tympanic membrane; 2) a normal pars flaccida and pars tensa of the tympanic membrane; 3) no history of otorrhea or perforation; 4) no history of otological surgery; 5) exclusion of an occluded external canal, intramembranous cholesteatoma, or giant cholesteatoma; and 6) no preclusion of a history of OM.
The OM group was used as the control group to compare the measured HU values with the congenital cholesteatoma group. We reviewed medical records including patient age, gender and symptoms in both groups.
Temporal bone CT was performed in the axial plane, and reformatted coronal images were obtained in all cases. CT imaging parameters were as follows: a Somatom Definition Flash (Siemens, Forchheim, Germany), 0.6 mm section thickness, 100 KVp, variable mAs protocol, CT dose index range 2-3 mGy, and 55-68 slices performed per examination.
Two radiologists (Y.W.K and S.H.A) retrospectively reviewed the CT images and independently measured HU of the soft tissue mass in axial and reformatted coronal images. HUs were measured on axial and reformatted coronal image slices that showed the largest diameter of soft tissue mass for each case. The region of interest (ROI) was placed within the mass in the middle ear cavity as large as possible, because a large ROI is generally preferred for measuring HU to decrease the variation of its value. Therefore, the ROI circles were centered on the mass and lay 1 mm inside from the margin of the mass to eliminate potential artifacts from the adjacent bony structure and the pneumatized middle ear cavity (Figs. 1, 2). The lower HU of the two values measured on axial and reformatted coronal images were selected in each case. The average HU value was calculated from the two lower HU values by the two radiologists. This average HU was defined as the representative value and was used for analysis (Table 1).
In addition, we evaluated the location of the mass, the relationship between the mass and ear ossicle, the presence or absence of bony erosions in the ear ossicle, and the status of the tympanic membrane in the congenital cholesteatoma group.
Twenty-one patients were enrolled in the congenital cholesteatoma group: 16 boys and 5 girls (mean age, 3.9 years; range, 2-7 years). Seventeen patients were incidentally discovered to have a white retrotympanic mass with an intact tympanic membrane during physical examination, including otoscopy, due to symptoms of the common cold, rhinitis, or enteritis. The other four patients had symptoms of OM such as otalgia or ear fullness and had a history of OM.
Twenty-two patients were enrolled in the OM group: 13 boys and 9 girls (mean age, 6.2 years; range, 1-18 years). Fourteen patients had symptoms of OM, five patients visited for a hearing test, two patients had symptoms of the common cold, and two patients were suspected to have cholesteatoma.
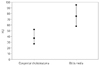
The mean HU value was 37.36 ± 6.11 (range, 27.5-52.5) in the congenital cholesteatoma group and 76.09 ± 8.74 (range, 58.5-96) in the OM group (p < 0.001) (Fig. 3). The HU cutoff value between the congenital cholesteatoma group and the OM group was calculated using the median value from the maximum HU value in the congenital cholesteatoma group and the minimum value in the OM group. The cut-off value was 55.5 between the two groups. A measured HU value < 55.5 can be considered congenital cholesteatoma, whereas an HU > 55.5 is considered OM.
The characteristics of congenital cholesteatoma (the largest diameter, location, ear ossicle erosion, and status of the tympanic membrane) are summarized in Table 1. The mean largest diameter was 4.98 ± 2.13 mm (range, 2.5-12 mm). The most common location was in the mesotympanum (14/21, 66.5%), followed by the epitympanum, and mesotympanum (5/21, 24%), and then the mesotympanum and hypotympanum (2/21, 9.5%). Five patients (24%) had ear ossicle erosion and 16 patients (76%) did not. All patients had intact tympanic membranes.
The HU is a linear transformation of the linear attenuation coefficient measurement, and all biological tissues have a unique HU (9, 10). Although cholesteatoma can be divided into congenital and acquired types, it consists of a combination of keratinous material and stratified squamous epithelium and the two types cannot be distinguished histologically (11). Therefore, congenital cholesteatoma and acquired cholesteatoma will theoretically have a similar HU. In contrast, non-cholesteatoma tissue exhibits a different HU because it has different histological components. A recent study by Park et al. (7) reported a HU of 42.68 ± 24.42 in the cholesteatoma group and 86.07 ± 26.50 in the non-cholesteatoma group. The difference between the two groups improved the diagnosis of cholesteatoma.
In the present study, the HU values of the congenital cholesteatoma group ranged from 27.5 to 52.5 and the mean value was 37.36 ± 6.11. All cases of congenital cholesteatoma had HU values < 64.4, which was consistent with the result of Park et al. (7), who reported a cut-off value of 64.4 HU between cholesteatoma and non-cholesteatoma groups. However, some cases of OM group in our study had HU values < 64.4. Therefore, their cut-off value (64.4 HU) could not be applied in our study. In the present study, no overlap in the value was observed between the cholesteatoma and OM groups. The HU differences between the two groups were significantly different, and the cut-off value was 55.5 HU. This result is probably due to the small sizes of the congenital cholesteatomas in our study. A larger cholesteatoma can lead to obstruction of the Eustachian tube and causes increased middle ear effusion and inflammatory changes. The largest diameter in the present study was small (4.98 ± 2.13 mm), and it did not present with these complications. Unlike congenital cholesteatoma, acquired cholesteatoma results from chronic infection with formation of granulation tissue, which contributes to its higher HU (12).
Another possible explanation for the lower HU in the present study is that little ear ossicle erosion (24%) was observed, and all cases were confined to the middle ear cavity. The mean HU of congenital cholesteatoma with ear ossicle erosion (39.6 ± 8.29) is higher than without ear ossicle erosion (36.65 ± 5.41) in our study. Bony erosion is rare in congenital cholesteatoma rather than acquired cholesteatoma (4). Although bone destruction is a part of acquired cholesteatoma, involvement of the adjacent bony structure leads to a higher HU because acquired cholesteatoma includes the remaining bone structure after bone destruction. Therefore, the lesser involvement of the adjacent bony structure contributes to the lower HU in the patients with congenital cholesteatoma. Furthermore, the mean largest diameter of congenital cholesteatoma with ear ossicle erosion (6.82 ± 2.96 mm) was larger than congenital cholesteatoma without ear ossicle erosion (4.4 ± 1.50 mm). These results support the hypothesis that smaller size and no bony erosion may affect lower HU in congenital cholesteatoma.
In the present study, congenital cholesteatoma was 3.2 times more common in boys, and the mean age was 3.9 years. Previous studies (8, 13, 14) have reported that congenital cholesteatoma is three times more common in boys than girls, and that the mean age of detection is 4.5 years. Our results are similar to those values.
The cholesteatomas of 17 patients (81%) were incidentally discovered, whereas four patients had symptoms of OM and a history of OM. This agreed with previous reports (8, 13) that most cases of congenital cholesteatoma are asymptomatic and incidentally discovered. In addition, all cases were found in the mesotympanum, in agreement with a previous study (14) that claimed that congenital cholesteatoma is often located in the anterior superior quadrant of the middle ear, close to the malleus manubrium.
Congenital cholesteatoma is usually considered when it is incidentally discovered as a white retrotympanic mass on otoscopy and a sharply marginated round soft tissue mass in the middle ear cavity on temporal bone CT. However, some cases are challenging to diagnose because temporal bone CT has low specificity for cholesteatoma. In the present study, the cut-off value was 55.5 HU between the cholesteatoma group and OM group. In conclusion, HU measurement may be useful as an additional indicator in the diagnosis of congenital cholesteatoma.
Figures and Tables
 | Fig. 1Congenital cholesteatoma of the left middle ear cavity in a 3-year-old boy. Axial (A) and reformatted coronal (B) temporal bone CT scans demonstrating a well-defined, round soft-tissue mass in the mesotympanum of the left middle ear cavity. The measured Hounsfield unit (HU) is 36 in axial image and 33 in coronal image. The lower HU of the two measured value were selected in this case. This mass considered as congenital cholesteatoma. |
 | Fig. 2Otitis media of the left middle ear cavity in a 5-year-old boy. Axial (A) and reformatted coronal (B) temporal bone CT scans demonstrating a well defined soft-tissue mass in epitympanum of the left middle ear cavity. It is difficult to distinguish otitis media from congenital cholesteatoma by image finding alone. The measured Hounsfield unit (HU) is 79 in axial image and 90 in coronal image. The lower HU of the two measured value were selected in this case. This mass considered as otitis media. |
References
1. McDonald TJ, Cody DT, Ryan RE Jr. Congenital cholesteatoma of the ear. Ann Otol Rhinol Laryngol. 1984; 93(6 Pt 1):637–640.
2. Trojanowska A, Trojanowski P, Olszanski W, Klatka J, Drop A. Differentiation between cholesteatoma and inflammatory process of the middle ear, based on contrast-enhanced computed tomography imaging. J Laryngol Otol. 2007; 121:444–448.
3. De Foer B, Vercruysse JP, Bernaerts A, Meersschaert J, Kenis C, Pouillon M, et al. Middle ear cholesteatoma: non-echo-planar diffusion-weighted MR imaging versus delayed gadolinium-enhanced T1-weighted MR imaging--value in detection. Radiology. 2010; 255:866–872.
4. Baráth K, Huber AM, Stämpfli P, Varga Z, Kollias S. Neuroradiology of cholesteatomas. AJNR Am J Neuroradiol. 2011; 32:221–229.
5. Smith PG, Leonetti JP, Kletzker GR. Differential clinical and radiographic features of cholesterol granulomas and cholesteatomas of the petrous apex. Ann Otol Rhinol Laryngol. 1988; 97(6 Pt 1):599–604.
6. Franklin DJ, Jenkins HA, Horowitz BL, Coker NJ. Management of petrous apex lesions. Arch Otolaryngol Head Neck Surg. 1989; 115:1121–1125.
7. Park MH, Rah YC, Kim YH, Kim JH. Usefulness of computed tomography Hounsfield unit density in preoperative detection of cholesteatoma in mastoid ad antrum. Am J Otolaryngol. 2011; 32:194–197.
8. Levenson MJ, Michaels L, Parisier SC. Congenital cholesteatomas of the middle ear in children: origin and management. Otolaryngol Clin North Am. 1989; 22:941–954.
9. Phelps ME, Hoffman EJ, Ter-Pogossian MM. Attenuation coefficients of various body tissues, fluids, and lesions at photon energies of 18 to 136 keV. Radiology. 1975; 117(3 Pt 1):573–583.
10. Brooks RA. A quantitative theory of the Hounsfield unit and its application to dual energy scanning. J Comput Assist Tomogr. 1977; 1:487–493.
11. Caponetti G, Thompson LD, Pantanowitz L. Cholesteatoma. Ear Nose Throat J. 2009; 88:1196–1198.
12. Fisch U. Tympanoplasty, Mastoidectomy, and Stapes Surgery. New York: Thieme;1994. p. 146.
13. McGill TJ, Merchant S, Healy GB, Friedman EM. Congenital cholesteatoma of the middle ear in children: a clinical and histopathological report. Laryngoscope. 1991; 101(6 Pt 1):606–613.
14. Nelson M, Roger G, Koltai PJ, Garabedian EN, Triglia JM, Roman S, et al. Congenital cholesteatoma: classification, management, and outcome. Arch Otolaryngol Head Neck Surg. 2002; 128:810–814.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download