Abstract
Tumefactive multiple sclerosis (MS) is a rare type of demyelinating disease. Typical magnetic resonance (MR) image findings show incomplete ring enhancement with a mild mass effect. This lesion is otherwise indistinguishable from other mass-like lesions in the brain. Knowledge of the MR imaging findings for tumefactive MS is thus helpful for correct diagnosis and appropriate therapy. In this report we describe the MR image findings for pathology-confirmed tumefactive MS in an uncommon location, alongside a discussion of its aggressive features.
Tumefactive multiple sclerosis (MS) is an uncommon manifestation of multiple sclerosis (1). The characteristic MRI findings for this demyelinating disease are a large isolated mass in the white matter with incomplete rim enhancement, slight perilesional edema and a mass effect (2, 3). The clinical features of tumefactive MS are variable and polysymptomatic, depending on the location and size of the mass (4). Patients with this lesion commonly present with headache, cognitive abnormalities, and sub-acute progressive motor and/or sensory symptoms (5). Most patients with this type of MS manifest only a single acute clinical presentation, whereas those with typical MS present with recurrent episodes of neurological symptoms (4, 6). For these reasons tumefactive MS is indistinguishable from glial neoplasm, lymphoma, abscess or other similar types of lesions (2). Thus, awareness of the characteristic MRI appearance of these lesions can be helpful for correctly diagnosing this condition in a noninvasive manner (6).
We report herein a case of pathologically confirmed tumefactive MS in an uncommon location, which showed atypical magnetic resonance (MR) imaging findings and a good response to steroid therapy. We also summarize the typical MR imaging findings for tumefactive MS that can be used to differentiate this lesion from others.
A 43-year-old woman presented with paresthesia of the right leg, a limping gait, blurred vision, and motor weakness of the right arm and leg. These symptoms had progressed for three weeks without any prior neurological symptoms. She showed ataxia on the right side on neurological examination.
The laboratory tests were negative, including examination of the cerebrospinal fluid. MRI of the brain showed a 5 cm irregular shaped hyperintense mass-like lesion with a bizarre margin and perilesional edema involving the white matter in the left temporal lobe on T2-weighted imaging. The lesion also involved the left posterior thalamus, posterior limb of the internal capsule, external capsule, and midbrain crus, with extension to the periventricular white matter of the left lateral ventricular atrium (Fig. 1A, B). Thick irregular and open rim enhancement with a central nonenhancing portion was noted on the post-gadolinium enhancement image (Fig. 1B). The left retrolenticular white matter was postulated to be the epicenter of the lesion. The lesion extended along the course of the left internal capsule fiber with incomplete rim enhancement of the left midbrain crus (Fig. 1B, C).
Our first diagnostic impression was of a brain tumor such as a high-grade glioma. The other potential diagnoses were primary lymphoma, tumefactive MS, or brain abscess.
Proton MR spectroscopy was obtained at the center of the mass. An increased concentration of choline and lactate and a decreased concentration of N-acetylaspartate (NAA) was observed (Fig. 1D). These findings were more compatible with brain tumor and tumefactive MS than with abscess. Stereotactic biopsy was then performed. The lesion showed normal brain tissue, and was composed of proliferated astrocytes, histiocytes and perivascular lymphocytes. Immunohistochemical staining for CD68 revealed numerous histiocytes and microglial cells in the lesion, although these findings are not detailed in the present report. The microscopic findings suggested benign reactive gliosis rather than an astrocytic tumor (Fig. 2). Finally, a brain tumor was ruled out and tumefactive MS was confirmed.
The patient was treated with oral methylprednisolone 12 mg/day for two months. Follow-up MRI revealed a marked decrease in the size of the irregular hyperintense lesion in the left temporal white matter, midbrain, internal capsule, external capsule, and posterior thalamus on T2-weighted image (Fig. 3). The neurologic symptoms also showed improvement.
The occurrence of solitary tumor-like multiple sclerosis, which is considered as a fulminant acute demyelinating plaque or conglomeration of acute plaques forming a mass in the brain, is rare (1). According to recent study, the prevalence of tumefactive MS has been reported to be 0.09% (7). However, it is likely that the true incidence rate is unknown, despite attempts in the literature to define it (5, 8). This type of MS commonly occurs in women with an average age of 37 years and usually features a single neurologic episode, whereas in classic MS there are repeated subacute episodes. Although the neurologic symptoms are dependent upon the location of the lesion, the common clinical features are motor, cognitive, sensory, cerebellar, and brainstem symptoms, in that order of frequency (5, 6). Visual disturbances, seizure, the appearance of a sudden cognitive deficit, and bowel dysfunction are relatively uncommon clinical presentations. The frontal lobe and parietal lobe are the most common locations of tumefactive MS (4, 5). Rare locations of the lesion, reported in less than 10% of cases, are the temporal lobe, cerebellum, deep gray matter, and brain stem. Corticosterioid therapy is important for improving the clinical symptoms and for decreasing the size of the lesion (2, 5).
Many researches have reported specific MRI findings in tumefactive MS. First, tumefactive MS lesions present as large isolated mass-like lesions that are round in form, and have a well-circumscribed margin. These lesions usually show homogeneous hypointensity on T1-weighted images and hyperintensity on T2-weighted images (2). Tumefactive MS is typically located in the supratentorial brain and is centered within the white matter (9). Second, tumefactive MS reveals a proportionally minor mass effect and perilesional vasogenic edema relative to the size of the lesion, compared to other mass-like lesions in the brain (1-3). Third, rim-like smooth enhancement, either complete or incomplete, or open rim or arc-like enhancement, is noted in approximately half of patients. This enhancement pattern consists of an enhanced leading edge of demyelination and a central nonenhancing portion representing a more chronic inflammatory state (8, 9). The open part of the ring enhancement is generally oriented towards the basal ganglia and the cortex (2). In addition, a multiplicity of the lesion can be helpful in the diagnosis of tumefactive MS. The lesion is typically located in the periventricular and subcortical white matter, or cervical spine (4, 5). In addition, MR spectroscopy usually shows similar spectrum to that of glioma, presenting as elevated choline and suppressed N-acetylaspartate (9).
Tumefactive MS can mimic tumors including high-grade glioma, primary lymphoma, and solitary metastasis, as well as other pseudotumoral brain lesions such as abscess, acute disseminated encephalomyelitis (ADEM) (2).
High-grade glioma mostly demonstrates heterogeneous signal intensity, irregular edges, extensive peritumoral edema or a mass effect, and there will commonly be an irregularly enhancing solid portion of the tumor present on gadolinium enhanced images (2, 4, 8-10). Brain lymphoma is easily confused with tumefactive MS owing to its unifocal features on MRI and its good response to steroid therapy (11). However, primary lymphoma in the brain shows marked homogeneous enhancement on T1-weighted post-contrast images and iso- or mild hyperintensity on T2-weighted images (2). A solitary cerebral metastasis often demonstrates central heterogeneous signal intensity with peripheral hypointensity on T2-weighted images and complete rim enhancement on gadolinium administration. Brain abscesses commonly have a complete hypointense rim on T2-weighted images, hyperintensity on diffusion weighted imaging, and regular complete rim enhancement on gadolinium enhanced images (2, 10). ADEM usually appears as small and bilateral lesions and the large isolated form is rare. Vaccination or infection commonly precedes ADEM, whereas tumefactive MS is rarely accompanied by this type of preceding history (2).
In our case, central homogeneous signal intensity with rim enhancement of the lesion was compatible with tumefactive multiple sclerosis rather than with intracranial neoplasm. However, the lesion revealed irregular and thick rim-enhancement with a bizarre margin, corresponding to an intracranial neoplasm. In addition, the location of the lesion was an uncommon site for multiple sclerosis. For these reasons, this patient underwent brain biopsy to assist in correct diagnosis. She could then be diagnosed with tumefactive multiple sclerosis and underwent corticosteroid therapy. After two months, the neurologic deficits improved, with a decrease in the size of the brain lesion on MRI.
This case suggests that when a patient who has an isolated large mass in the white matter of the brain with incomplete rim enhancement on MRI shows transient neurological dysfunction, consideration of tumefactive MS may be helpful for avoiding unnecessary procedures and is also likely to be useful in selection of the appropriate treatment.
Figures and Tables
Fig. 1
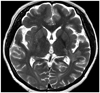
A 43-year-old female with tumefactive multiple sclerosis.
A. An irregularly shaped mass-like lesion approximately 5 cm in size involves the white matter of the left temporal lobe. The lesion shows high signal intensity on axial T2-weighted image and extends to the left posterior thalamus, posterior limb of the internal capsule, and the external capsule. Also this hyperintensity extends to the periventricular white matter near the left lateral ventricular atrium.
B, C. After gadolinium enhancement, the lesion demonstrates thick and irregular rim-like enhancement with extension along the course of the left internal capsule on coronal image (B) and the left midbrain crus, with incomplete rim enhancement on axial image (C).
D. Magnetic resonance spectroscopy of the mass in left temporal lobe demonstrates elevated choline and lactate, and decreased N-acetylaspartate.

References
1. Rusin JA, Vezina LG, Chadduck WM, Chandra RS. Tumoral multiple sclerosis of the cerebellum in a child. AJNR Am J Neuroradiol. 1995; 16:1164–1166.
2. Comi G. Multiple sclerosis: pseudotumoral forms. Neurol Sci. 2004; 25:Suppl 4. S374–S379.
3. Kim DS, Na DG, Kim KH, Kim JH, Kim E, Yun BL, et al. Distinguishing tumefactive demyelinating lesions from glioma or central nervous system lymphoma: added value of unenhanced CT compared with conventional contrast-enhanced MR imaging. Radiology. 2009; 251:467–475.
4. Elsone L, Platkajis A, Karelis G, Dzelzite S, Murzina M. Tumefactive multiple sclerosis mimicking neoplasm. Acta Chirurgica Latviensis. 2010; 10:91–97.
5. Lucchinetti CF, Gavrilova RH, Metz I, Parisi JE, Scheithauer BW, Weigand S, et al. Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosis. Brain. 2008; 131(Pt 7):1759–1775.
6. Mandrioli J, Ficarra G, Callari G, Sola P, Merelli E. Monofocal acute large demyelinating lesion mimicking brain glioma. Neurol Sci. 2004; 25:Suppl 4. S386–S388.
7. Annesley-Williams D, Farrell MA, Staunton H, Brett FM. Acute demyelination, neuropathological diagnosis, and clinical evolution. J Neuropathol Exp Neurol. 2000; 59:477–489.
8. Law M, Yang S, Wang H, Babb JS, Johnson G, Cha S, et al. Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol. 2003; 24:1989–1998.
9. Given CA 2nd, Stevens BS, Lee C. The MRI appearance of tumefactive demyelinating lesions. AJR Am J Roentgenol. 2004; 182:195–199.
10. Schwartz KM, Erickson BJ, Lucchinetti C. Pattern of T2 hypointensity associated with ring-enhancing brain lesions can help to differentiate pathology. Neuroradiology. 2006; 48:143–149.
11. Kantarci OH, Weinshenker BG. Natural history of multiple sclerosis. Neurol Clin. 2005; 23:17–38. v




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download