Abstract
The complication of growth disturbance after physeal fracture of the distal tibia has been well recognized. Although irreducible fractures of the physis due to trapped soft tissue, including periosteum, are not common, it could still cause growth disturbances. Therefore, the detection of periosteal interposition with physeal injury on imaging study is important. We present a case of a 10-year-old girl with surgically confirmed periosteal interposition in the distal tibial Salter-Harris type I fracture, through magnetic resonance imaging findings.
The distal tibia is the second most common site of physeal fracture, followed by the distal radius (1). Salter-Harris (S-H) type I fracture has been considered as a low-grade physeal injury and usually needs conservative management with closed reduction and immobilization (2). However, although not commonly seen, soft tissue structures, including periosteum, tendons and ligaments, can be interposed in the physis, and it has been associated with subsequent growth disturbances and requires open surgical reductions to remove the entrapped structures (3-5). Particularly, interposed periosteum in the physis has been reported as the most common cause of failed closed reductions (3-5). Although irreducible fractures of the physis due to interposed soft tissues have been reported in the orthopedic literature, there are only a few reports concerning the preoperative magnetic resonance (MR) imaging diagnosis. We report MR imaging findings of distal tibial S-H type I fracture with periosteal interposition, which underwent open surgical reduction.
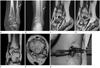
A 10-year-old girl was being presented with a distal lower left extremity injury by a traffic accident. Initial CT scans of the left ankle demonstrated a widening of the medial aspect of the distal tibial physis, which was consistent with Salter-Harris type I fracture and fracture of distal shaft of the fibula (Fig. 1A). Closed reduction with immobilization was performed. Subsequent plain radiographs showed physeal widening (4 mm width) of medial portion of the distal tibia one month later (Fig. 1B). The possibility of soft tissue entrapment within the fractured physis of the distal tibia was considered, and MR imaging was performed. MR imaging of the left ankle demonstrated a linear low signal structure on T2-weighted images extended into the widened physis of anteromedial portion of the distal tibia and surrounding intermediate to low signal lesion (Fig. 1C-F). These lesions were interpreted as an entrapment of torn displaced periosteum within the fractured physis and the surrounding granulation tissues.
Subsequently, she underwent open surgical reduction. At surgery, trapped periosteum within the widened physis was identified in an anteromedial aspect of the distal tibial physis, and fibrous or granulation tissues were filled in the widened physis. These lesions were removed. After the removal of the entrapped periosteum, a widening of the distal tibial physis was noted up to a width of 4 mm (Fig. 1G). A diagnosis of periosteal interposition in distal tibial S-H type I fracture was confirmed.
Ankle fractures account for approximately 15% of physeal injuries and the overall incidence of physeal complications after physeal fracture has been reported to be between 2% and 14.1% (2, 6). S-H type I fractures account for approximately 15% of distal tibia physeal fractures (2). While S-H type I fracture has been previously considered as a low-risk injury, a high incidence of premature physeal closure was reported with a rate of 22% to 36% in the few recent studies (4, 6).
Multiple factors proposed as influencing rates of growth disturbances included fracture type and location, displacement, energy of injury, patient's remaining growth potential (age and skeletal maturity) and quality of reduction (4, 6). Also, entrapped periosteum has been described as one of the common causes for irreducible fractures of the distal tibia (5). Other soft tissue structures, such as muscles, tendons and ligaments, also result in irreducibility by trapping in the physeal injury site (5). Studies in animal models have reported that the combination of physeal cartilage injury with periosteal interposition produces poor organizations of the remaining physeal growth plate; thus, producing increased risks of physeal bar formation and also showed significant growth disturbances as compared with fractures of the intact physes (7, 8).
Plain radiography is the initial modality to evaluate physeal injuries and could be sufficient in majority of the cases. In a previous study, it has been reported that the radiographic presence of post-reduction residual physeal gap in S-H type I and II fractures of the distal tibia could suggest interposed periosteum (4). In their study, a gap of more than 3 mm on anteroposterior or lateral radiograph was identified as positive, and their result showed a 3.5-fold increase in the incidence of premature physeal closure, if a gap was presented on the postreduction radiography in S-H type I and II fractures (5). In our case, the residual gap measured as 4 mm on an anteroposterior radiograph, was followed up one month after a closed reduction. The findings in our case suggest the possibility of interposed periosteum within the fractured physis.
MR imaging can clearly demonstrate the morphology, signal intensity of the physis, as well as the relationship between the physis and surrounding structures (9). In a previous study, it has been reported that physeal injury was presented as a low signal intensity, which was similar to the normal physis, on T1-weighted imaging; and as a high signal intensity, which was different from an intermediate signal intensity of the normal physis, on T2-weighted imaging (9). Also, MR imaging has been used for detecting patterns of growth plate injury not depicted on a plain-film, particularly in S-H type I and V fractures (3). Soft tissue entrapments, especially periosteal interposition in physeal fractures, can be demonstrated as linear low signal intensity structures within the widened physis on proton density weighted images with or with156out fat saturation and T2-weighted images (3, 10). MR imaging of ankle in our case also showed entrapped low signal intensity structures within the widened physis on T2-weighted images. However, only a few literatures reported MR imaging findings of trapped periosteum in physeal injury (3, 10).
The usual treatment of S-H type I and II fractures of the distal tibia is closed reduction and immobilization, while S-H type III and IV fractures are treated with open reduction and internal fixation. However, S-H type I and II fractures, which failed with closed reduction, are indications of open surgical reductions. In the orthopedics literature, the most common cause of reduction failure has been recognized as an entrapped periosteum (3). In these cases, open reduction and removal of interposed periosteum in the fractured physis allow for more anatomic reductions and may decrease the incidence of complications, such as non-unions and growth disturbances (4).
The detection of entrapped periosteum with physeal injury on imaging technique is important because perioteal interposition can be the cause of irreducibility and result in complications after physeal fracture. MR imaging can be effective in demonstrating soft tissue entrapments including periosteum or granulation tissue in physeal fractures, as in our case; thereby, allowing a prompt, appropriate operation, which may prevent potential complications.
Figures and Tables
 | Fig. 1Periosteal interposition in a distal tibial Salter-Harris type I fracture in 10-year-old girl.
A. Coronal reformatted image of left ankle CT scan shows a widening of the medial aspect of distal tibial physis (arrowheads), suggesting Salter-Harris type I fracture. Fracture of distal fibular shaft is also noted (arrow).
B. Follow-up radiograph (one month after trauma) shows physeal widening (4 mm width) of medial portion of the distal tibia (arrowheads) and fracture of distal fibular shaft (arrow).
C-F. Sagittal (C, D) and coronal (E) T2-weighted images show linear low signal structure (arrowhead) in the anteromedial physis of the distal tibia representing entrapped periosteum and surrounding thick intermediate to low signal lesion (arrow) which is suspected as granulation tissue. Axial T2-weighted image (F) obtained at level of physis shows low signal periosteum (arrowhead) and broad intermediate to low signal lesion (arrow) trapped in anteromedial growth plate of distal tibia.
G. Intraoperative photograph of distal tibia shows a widening of physis (arrowheads), up to 4-mm width. The entrapped periosteum is clearly removed.
|
References
1. Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop. 1990; 10:713–716.
2. Kay RM, Matthys GA. Pediatric ankle fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001; 9:268–278.
3. Whan A, Breidahl W, Janes G. MRI of trapped periosteum in a proximal tibial physeal injury of a pediatric patient. AJR Am J Roentgenol. 2003; 181:1397–1399.
4. Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003; 23:733–739.
5. Grace DL. Irreducible fracture-separations of the distal tibial epiphysis. J Bone Joint Surg Br. 1983; 65:160–162.
6. Leary JT, Handling M, Talerico M, Yong L, Bowe JA. Physeal fractures of the distal tibia: predictive factors of premature physeal closure and growth arrest. J Pediatr Orthop. 2009; 29:356–361.
7. Gruber HE, Phieffer LS, Wattenbarger JM. Physeal fractures, part II: fate of interposed periosteum in a physeal fracture. J Pediatr Orthop. 2002; 22:710–716.
8. Phieffer LS, Meyer RA Jr, Gruber HE, Easley M, Wattenbarger JM. Effect of interposed periosteum in an animal physeal fracture model. Clin Orthop Relat Res. 2000; 15–25.
9. Shi DP, Zhu SC, Li Y, Zheng J. Epiphyseal and physeal injury: comparison of conventional radiography and magnetic resonance imaging. Clin Imaging. 2009; 33:379–383.
10. Raman S, Wallace EC. MRI diagnosis of trapped periosteum following incomplete closed reduction of distal tibial Salter-Harris II fracture. Pediatr Radiol. 2011; 41:1591–1594.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download