Abstract
Enterobacter species have increasingly been identified as pathogens over the past several decades. These bacterial species have become more important because most are resistant to cephalothin and cefoxitin, and can produce extended-spectrum β-lactamase. Enterobacter Asburiae (E. asburiae) is a gram-negative rod of the family Enterobacteriaceae, named in 1986. Since then, there has been only one clinical report of E. asburiae pneumonia. We report a case of E. asburiae pneumonia with cavitation and compare it with the previous case.
Enterobacter species have increasingly been identified as pathogens over the past several decades (1). Enterobacter Asburiae (E. asburiae) is a gram-negative rod of the family Enterobacteriaceae (2), classified as the Enteric group 17 by Farmer et al. (3). The species was named in 1986 (2), and since then, there has only been one clinical report of E. asburiae pneumonia (1). We report a case of E. asburiae pneumonia with cavitation and compared it with the previous case.
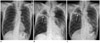
A 74-year-old man was admitted to our hospital and underwent radiofrequency ablation due to hepatocellular carcinoma. His chest radiograph was clear at that time (Fig. 1A).
Six months later, he was admitted to the emergency department with fever, chills and facial rash. His legal guardian said that he was in the habit of playing computer games and smoking through the night. Chest radiography revealed a large cavity in the right upper lobe and extensive consolidation in the left lung (Fig. 1B).
Because our location is an area of endemic pulmonary tuberculosis, we started anti-tuberculous medication (Isoniazid 300 mg, Rifampin 450 mg, Ethambutol 600 mg, Pyrazinamide 1000 mg). The consolidation improved slightly after 3 weeks, but the patient's condition did not get better. In the meantime, E. asburiae was cultured from his sputum. This bacterium was resistant to several antibiotics: Amoxicillin, Ampicillin, Cefoxitin and Cephalothin. We therefore stopped anti-tuberculous medication and changed to IV antibiotics (Tazoperan 4.5 g). Subsequently, patient's condition improved and the consolidation in the left lower lobe disappeared (Fig. 1C). However, the cavitary lesion in the right upper lobe has persisted until now.
Enterobacter species have increasingly been identified as pathogens over the past several decades (1). These bacteria have become more important because most of them are resistant to cephalothin and cefoxitin (4), and they can produce extended-spectrum β-lactamase (ESBL). In Korea, Choi et al. (5) reported that 12.8% of Enterobacter isolates produce ESBL.
There has been only one clinical report of E. asburiae pneumonia (1). This previous case and ours have in common the presence of cavitation on chest radiography. Of course, other gram-negative bacteria can cause cavitation, especially Klebsiella, Proteus, and Pseudomonas (6), but cavitation due to Enterobacter species appears to be less common than cases due to other gram-negative bacilli (7). The clinical and laboratory manifestations of E. asburiae pneumonia differ little from those of other gram-negative pneumonias, but the symptoms of E. asburiae pneumonia may be subtle or muted, especially in the elderly (7).
Although there is only one previous reported case of E. asburiae pneumonia, both it and our case involve cavitation. The subtlety of the symptoms of E. asburiae pneumonia may be the reason why patients only come to the hospital after a considerable progression of pneumonia, and the delay could be responsible for lung cavitation. Another possible cause of cavitation is the tendency of E. asburiae to grow rapidly. These characteristics tend to lead to abscess formation.
Figures and Tables
Fig. 1
Enterobacter asburiae pneumonia with cavitation in a 74-year-old man.
A. Chest radiograph after radiofrequency ablation for hepatocellular carcinoma is clear.
B. Radiograph obtained after 6 months for the evaluation of fever shows a large cavity in the right upper lobe (arrow) and extensive consolidation in the left lung.
C. After administration of IV antibiotics (Tazoperan 4.5 g), consolidation in the left lower lobe disappeared. The cavitary lesion in the right upper lobe (arrow) has persisted until now.
References
1. Stewart JM, Quirk JR. Community-acquired pneumonia caused by Enterobacter asburiae. Am J Med. 2001. 111:82–83.
2. Brenner DJ, McWhorter AC, Kai A, Steigerwalt AG, Farmer JJ 3rd. Enterobacter asburiae sp. nov., a new species found in clinical specimens, and reassignment of Erwinia dissolvens and Erwinia nimipressuralis to the genus Enterobacter as Enterobacter dissolvens comb. nov. and Enterobacter nimipressuralis comb. nov. J Clin Microbiol. 1986. 23:1114–1120.
3. Farmer JJ 3rd, Davis BR, Hickman-Brenner FW, McWhorter A, Huntley-Carter GP, Asbury MA, et al. Biochemical identification of new species and biogroups of Enterobacteriaceae isolated from clinical specimens. J Clin Microbiol. 1985. 21:46–76.
4. Ehrhardt AF, Sanders CC, Thomson KS, Watanakunakorn C, Trujillano-Martin I. Emergence of resistance to imipenem in Enterobacter isolates masquerading as Klebsiella pneumoniae during therapy with imipenem/cilastatin. Clin Infect Dis. 1993. 17:120–122.
5. Choi SH, Lee JE, Park SJ, Kim MN, Choo EJ, Kwak YG, et al. Prevalence, microbiology, and clinical characteristics of extended-spectrum beta-lactamase-producing Enterobacter spp., Serratia marcescens, Citrobacter freundii, and Morganella morganii in Korea. Eur J Clin Microbiol Infect Dis. 2007. 26:557–561.
6. Hansell DM, Lynch DA, McAdams HP, Bankier AA. Imaging of the diseases of the chest. 2005. Philadelphia: Elsevier Mosby.
7. Sanders WE Jr, Sanders CC. Enterobacter spp.: pathogens poised to flourish at the turn of the century. Clin Microbiol Rev. 1997. 10:220–241.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download