INTRODUCTION
Gout is a relatively common, crystal deposition disease that is common in middle-aged males. In chronic tophaceous gout, monosodium urate crystals are deposited in joint and periarticular tissues of the extremities such as feet, hands, wrists, elbows and knees. In contrast, spinal involvement of gout is exceedingly rare. Gout is most common in the feet. In cases of patients with spinal gout, many present with symptomatic cord or root compression (1234). In most of these patients, spinal involvement is secondary to involvement of the appendicular skeleton (2). Herein we present a case of tophaceous gout with extensive spinal involvement that resulted in diffuse spinal cord compression and led to paraplegia.
CASE REPORT
A 52-year-old man presented with a history of progressive motor weakness and sensory loss of both upper and lower extremities over the last two years ago. His status had been deteriorating more rapidly over the previous one year and he was bed-bound on admission. The patient had a past medical history of diabetes mellitus for 22 years and diabetic nephropathy for 12 years. He also had hypertension for over 10 years and was in a state of chronic renal failure. He was suffering from arthralgia of multiple sites in both hands, wrists, knees and shoulders and paresthesia below shoulders. On a neurologic examination, muscle power of all limbs was reduced to grade I.
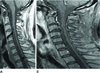
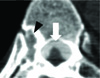
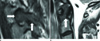
In conventional radiographs of the lumbosacral spine taken on the second day of admission, we noticed focal sclerotic changes at the anterior corner of the superior endplate of the 4th lumbar vertebrae (Fig. 1A). However, after magnetic resonance imaging, we recognized a high density area at the posterior aspect of the vertebral bodies. Other conventional radiographs of both hands and feet revealed radio-opaque, mass-like depositions in soft tissues and marginal bony erosions in multiple sites (Fig. 1B, C). The uric acid level in the blood was 12.2 mg/dL. In an aspirate of the knee joint, monosodium urate crystals were found on monopolarized microscopes. Chronic tophaceous gout was suspected, and an MRI examination of the spine was done to evaluate for motor weakness of the extremities. Sagittal T2-weighted images of the whole spine revealed a long band-like lesion just posterior to the vertebral bodies that showed low signal intensity with heterogeneity (Fig. 2). The band was located in the anterior epidural space and was continuous from the 2nd cervical vertebrae to the 5th lumbar vertebrae. A small erosion was noted at the lower anterior corner of the 6th thoracic vertebral body. The lesion showed low to intermediate signal on T1-weighted images and no enhancement (Fig. 3). The spinal cord was compressed in the long segment from the level of the 3rd cervical vertebrae to the 8th thoracic vertebrae without a clearly notable signal change. Costovertebral joints were involved, with erosion of adjacent vertebrae. The lesion was seen as hyperdense soft tissue, less dense than bone or calcification on an unenhanced CT scan (Fig. 4). The atlantodental joint and the facet joint area were also involved, showing soft tissue deposition in synovial space similar to deposition in epidural space (Fig. 5). Findings were consistent with a diagnosis of chronic tophaceous gout.
The patient is undergoing conservative management because of the high surgical risks which were based on the patient's status and the low possibility of recovery from neurologic symptoms.
DISCUSSION
Gout is a common metabolic disorder caused by deposition of monosodium urate crystals within or around the joints after chronic hyperuricaemia. It affects 1-2% of adults in developed countries. The prevalence of gout is much higher in men than in women and rises with age. Gout frequently presents in the peripheral joints, such as the first metatasophalangeal joint, the knee, the ankle and maybe even the distal interphalangeal joint, but this is not always the case (12). Tophi deposition can happen anywhere in the body including unusual locations such as the proximal appendicular or axial skeleton (15).
Axial gouty arthropathy can clinically mimic spinal metastases, spinal stenosis, or infection (2). Clinical manifestations of spinal gout are nonspecific, with local pain, radicular symptoms and paraparesis or tetraparesis occurring due to neural compression (6).
The appearance of tophaceous gout on an MRI is non-specific and reports are few for spinal gout. The tophi manifested as a low-to-intermediate signal intensity on T1-weighted images. The signal intensity on T2-weighted images was more variable, ranging from a homogenous high signal intensity to a homogenous low signal intensity (37). The high signal intensity on T2-weighted images in some tophi may reflect high protein content or result in locally increased water content. Signal drop-out foci in tophi may be the result of calcification, and can be seen on CT. The enhancement pattern is also variable, probably due to the differences in the relative amounts of vascular fibrous tissue in the tophi. Both homogeneous enhancement and heterogeneous peripheral enhancement have been described (4789).
The differential diagnosis of spinal gout should include infection and malignancy. Some authors reported MR findings indicating less possibility of spinal infection in patients with cervical spinal gout. A segmental pattern of disk involvement and sharply marginated vertebral erosions without surrounding infiltrative change are manifested, and these are unusual finding in diskovertebral infection (310). Clinically, rheumatoid arthritis and periodontoid pseudotumor (calcium pyrophosphate deposition disease) are also mimics of gout. In such cases, dual-energy CT may be used to differentiate gout from inflammatory mimics, hopefully demonstrating urate crystals. In addition, dual-energy CT findings may be valuable in excluding calcium, such as bone or dystrophic calcification from gouty urate crystals. Because dual-energy CT has two X-ray tubes with different peak kilovoltages (80 and 120 kVp), materials react differently depending on the elements of which they are composed. When urate crystals and calcium containing mineralization show indistinguishable hyperattenuation on a routine diagnostic CT, dual-energy CT has an advantage in differentiating urate crystals from calcium containing mineralization (5).
Medical treatment may be effective for local pain with colchicine or non-steroidal anti-inflammatory drugs. However, a patient with neural compression usually requires surgical decompression for acute management (14).
In conclusion, spinal gout is rare, but it is important to be aware of the possibility. Although biopsy is required for the definitive diagnosis, it is not always necessary if clinical and MR findings provide a reasonably high suspicion for gout (3). The diagnosis of spinal gout should be considered when the MRI demonstrates intermediate or low signal on T1 weighted images and deposits with low signal foci on all sequences, especially those involving the posterior elements.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download