Abstract
We describe a case of immunoglobulin G4 (IgG4)-related sclerosing esophagitis occurring in a 63-year-old man with progressive dysphagia and 10-kg weight loss over 9 months. An esophagoscopy revealed significant stricture with diffuse mucosal friability and ulceration at mid esophagus level. Barium esophagogram showed diffuse stenosis at the mid and lower esophagus levels with ulcerations and irregularity of the mucosa. Multidetector computed tomography revealed diffuse edematous and circumferential thickening of the submucosa and muscle layer of this esophageal segment. Fluorine 18 fluorodeoxyglucose positron emission tomography (FDG PET) revealed diffuse mild FDG uptake in mid to lower esophagus. Although benign inflammatory lesion was suspected based on the imaging findings, the patient underwent surgery for worsening esophageal stricture and the esophageal lesion was pathologically confirmed as IgG4-related sclerosing esophagitis. Radiologic benignancy and high clinical suspicion for IgG4-related sclerosing disease may help making a proper decision and avoiding unnecessary operation.
Immunoglobulin G4 (IgG4)-related sclerosing disease is characterized by extensive infiltration of numerous IgG4 positive plasma cells in various organs including the pancreas, biliary tree, salivary glands, thyroid gland, lungs, stomach, colon, kidneys, liver, retroperitoneum, prostate and lymph nodes (12). Most IgG4-related sclerosing diseases have been associated with auto-immune pancreatitis (AIP), but in some cases, IgG4-related sclerosing diseases without AIP and involving only one or two organs have been reported. These can be presented as a form of pseudotumor and frequently be confused with malignant tumor both clinically and radiologically (2). We recently experienced a rare case of isolated involvement of the esophagus as part of the IgG4-related sclerosing disease and presented with worsening stricture of the esophagus. Although the pre-operative radiologic findings revealed the tumors benign nature with its diffuse wall thickening of the entire esophagus and mild fluorodeoxyglucose (FDG) uptake, the patient underwent an esophagectomy for progressive stricture and the possibility of a hidden malignancy. This report may contribute to the recognition of the possibility of IgG4-related disorders and avoidance of unnecessary surgery in conditions clinically suspected as malignant.
The same case has already been published by Lee et al. (3) in the department of internal medicine of our institute but focused on the clinical aspect. However, the figures of multidetector computed tomography (MDCT) and FDG positron emission tomography (PET) have not been included and there was a lack of radiologic description for the esophagogram. Our paper places more emphasis on radiologic findings, especially MDCT and FDG PET findings and has a totally different point of view compared with Lee's article.
A 63-year-old man with a 9 month-history of progressive dysphagia and 10 kg weight loss was referred to our institution. The man had no history of autoimmune disease or connective tissue disorder, radiation, lye ingestion, or any medication. In addition, the patient had no abnormalities on a physical examination and laboratory data. An esophagoscopy revealed diffuse mucosal friability and ulceration with fibrotic change at 28 cm from the upper incisor and significant stricture at the esophageal level. An endoscope could not proceed to the distal esophagus due to the presence of stricture. A barium esophagogram demonstrated diffuse stenosis at the mid and lower esophageal levels with a few ulcerations and irregularity of the mucosa (Fig. 1). However, the finding of smooth narrowing without abrupt shouldering in the stenotic portion of the esophagus on an esophagogram suggested benign stricture rather than malignancy. An axial and coronal reformatted MDCT scan revealed diffuse edematous and circumferential thickening of the submucosa and muscle layer with mucosal enhancement involving the mid to distal segment of the esophagus (Fig. 2). The MDCT findings of diffuse circumferential edematous thickening without layer destruction involving long segment of esophagus are also in favor of a benign inflammatory or infectious condition than malignancy. There were centrilobular nodular infiltrations in the right upper lobe and the right lower lobe as well as a strong suspicion of active pulmonary tuberculosis. Acid fast bacilli were isolated 3 weeks later on a sputum culture. Consequently, we included tuberculous esophagitis as a possible diagnosis.
An endoscopic biopsy showed chronic active inflammation and granulation tissue, but a polymerase chain reaction for Mycobacterium tuberculosis was negative. There was no microscopic evidence of caseating granuloma. Although there was no histological evidence of malignancy, FDG PET-CT was performed to exclude a possible hidden malignancy at the distal esophagus level (Fig. 3). PET-CT revealed diffuse mild FDG uptake with about standardized uptake value 2.6 in the mid to lower esophagus and the PET findings were suggestive of an inflammatory condition rather than malignancy. Mild FDG uptake was also noted in the pulmonary tuberculosis lesion. The patient received conservative treatment with proton pump inhibitors, as well as antacids and anti-tuberculosis medication. A follow-up endoscopy performed 2 months later revealed extended mucosal fibrotic change at 20 cm from upper incisor and progression of luminal stricture with hemorrhage. The follow-up chest CT scan also revealed mild progression of circumferential wall thickening with mucosal enhancement at the mid to distal esophagus. However, the finding of pulmonary tuberculosis was improved after anti-tuberculosis medication. The patient presented debilitating symptoms and worsening esophageal stricture, thus suggesting the possibility of a hidden malignancy. As a result, an esophageal resection with colonic interposition was performed. The gross specimen revealed a circumferential stricture of 10 cm in length with mucosal ulceration and thickening. The narrowest luminal circumference was approximately 1.6 cm. A microscopic examination revealed transmural chronic inflammation with lymphoplasmacytic infiltration and stromal sclerosis (Fig. 4). IgG4 immunostaining revealed abundant IgG4-positive plasma cells; up to 200 per high power field.
The post-operative serum level of IgG4 was elevated at 138 mg/dL. The pre-operative IgG4 level was not obtained because there was no suspicion for IgG4-related condition. A postoperative abdominal CT scan and preoperative chest CT scans demonstrated no evidence of autoimmune pancreatitis, cholangitis, lymphadenopathy, retroperitoneal or mediastinal fibrotic mass. Consequently the patient was diagnosed with isolated IgG4-related sclerosing esophagitis.
IgG4-related sclerosing disease is a systemic disease, characterized histopathologically by extensive IgG4-positive plasma cells and T-lymphocyte infiltration of various organs including the pancreas, biliary tree, salivary glands, thyroid gland, lungs, stomach, colon, kidneys, liver, retroperitoneum, prostate and lymph nodes. Gastrointestinal involvement of IgG4-related slcerosing disease is rarely reported. Fujita et al. (4) first reported a IgG4-related gastric ulcer without auto-immune pancreatitis. Lopes et al. (2) first reported a case of isolated involvement of the esophagus, manifesting as a focal circumferential mass secondary to IgG4 plasma cell infiltration, which was in contrast to our case manifesting diffuse circumferential wall thickening involving the long segment of the esophagus. The lesion was a chronic form of inflammation resulting in a pseudotumor.
Hamano et al. (5) have first reported elevated serum IgG4 levels in sclerosing pancreatitis. Elevated serum IgG4 is a sensitive marker and supportive serologic criteria for diagnosis of autoimmune pancreatitis that is indicative of IgG4-related sclerosing disease (16). However, this finding was not specific for this disease and also could be observed in other disorders such as asthma or atopic dermatitis (7). Due to the lack of specificity of serum IgG4 level and wide spectrum of radiologic and clinical findings, pre-operative diagnosis of IgG4-related disease can be difficult (2). Patients with auto-immune pancreatitis or other auto-immune disorders have often been treated with resection because their clinical and radiological appearance was suggestive of a malignancy (28). Our case was also suspected as esophageal cancer due to ulceration with stricture on endoscope. However, the finding of smooth narrowing without abrupt shouldering in the stenotic portion of the esophagus on an esophagogram, suggested benign stricture rather than malignancy. The MDCT findings of diffuse circumferential edematous thickening of submucosa and muscle layer involving a long segment of the esophagus without layer destruction or serosal invasion are also in favor of the benign inflammatory or infectious condition than malignancy. No definable mass-forming lesion was observed in the esophagus, which was different from the usual imaging findings of esophageal cancer or previously reported pseudotumors which showed isolated involvement of the esophagus via the IgG4 plasma cell. Also, there were no necrotic lymph nodes or significant enlarged lymph nodes in the mediastinum, hence suggesting metastatic lymphadenopathy. Radiologic benignancy with accompanying active pulmonary tuberculosis initially led to the misdiagnosis of the esophageal lesion as esophageal tuberculosis.
In conclusion, this is the first report describing the MDCT and FDG PET findings of a case of IgG4-related sclerosing esophagitis manifesting as a diffuse wall thickening form as seen in the radiologic literature. Although malignant tumors are frequently suspected on initial presentation of IgG4-related sclerosing disease, isolated IgG4-related sclerosing esophagitis is relatively rare. Radiologic benignancy and high clinical suspicion for IgG4-related sclerosing disease in cases of worsening stricture or debilitating dysphagia may help making proper decision-making and avoiding unnecessary surgery.
Figures and Tables
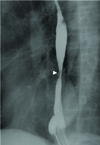 | Fig. 1Right lateral oblique image of an esophagography shows smooth stricture at the and lower esophageal level with mucosal irregularity. Ulceration is noted at the stenotic portion of the mid esophagus level (arrowhead). |
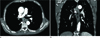 | Fig. 2A 63-year-old man with progressive dysphagia and 10 kg weight loss for 9 months. (A) Axial and (B) reformatted coronal images of a 64 slice MDCT with enhancement demonstrate circumferential edematous thickening in the submucosa and muscle layer (arrow) with mucosal enhancement (arrowhead) involving a long segment of the mid and distal esophagus.Note.-MDCT = multidetector computed tomography
|
 | Fig. 3PET images.
A. MIP image of 18F-FDG PET shows diffuse mild FDG uptake at the mid and distal esophagus level (arrowhead).
B. PET/CT fusion image shows mild FDG uptake in the esophageal mucosa at the subcarinal level (arrowhead). Mild FDG uptake is also demonstrated in active tuberculosis lesions of the right lung (arrow).
Note.-18F-FDG PET = 18F-fluorodeoxyglucose positron emission tomography, MIP = Maximum-Intensity-Projection
|
References
1. Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008; 14:3948–3955.
2. Lopes J, Hochwald SN, Lancia N, Dixon LR, Ben-David K. Autoimmune esophagitis: IgG4-related tumors of the esophagus. J Gastrointest Surg. 2010; 14:1031–1034.
3. Lee H, Joo M, Song TJ, Chang SH, Kim H, Kim YS, et al. IgG4-related sclerosing esophagitis: a case report. Gastrointest Endosc. 2011; 73:834–837.
4. Fujita T, Ando T, Sakakibara M, Hosoda W, Goto H. Refractory gastric ulcer with abundant IgG4-positive plasma cell infiltration: a case report. World J Gastroenterol. 2010; 16:2183–2186.
5. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.
6. Chen CC. Autoimmune pancreatitis and IgG4-related sclerosing disease: an emerging disease entity. J Chin Med Assoc. 2008; 71:1–3.
7. Okazaki K, Uchida K, Matsushita M, Takaoka M. How to diagnose autoimmune pancreatitis by the revised Japanese clinical criteria. J Gastroenterol. 2007; 42:Suppl 18. 32–38.
8. Hirano K, Komatsu Y, Yamamoto N, Nakai Y, Sasahira N, Toda N, et al. Pancreatic mass lesions associated with raised concentration of IgG4. Am J Gastroenterol. 2004; 99:2038–2040.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download