1. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiol ogy of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990; 132:910–925.
2. Körner H, Söndenaa K, Söreide JA, Andersen E, Nysted A, Lende TH, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997; 21:313–317.
3. Al-Omran M, Mamdani M, McLeod RS. Epidemiologic features of acute appendicitis in Ontario, Canada. Can J Surg. 2003; 46:263–268.
4. Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP. Appendectomy: a contemporary appraisal. Ann Surg. 1997; 225:252–261.
5. Quillin SP, Siegel MJ. Diagnosis of appendiceal abscess in children with acute appendicitis: value of color Doppler sonography. AJR Am J Roentgenol. 1995; 164:1251–1254.
6. Oliak D, Yamini D, Udani VM, Lewis RJ, Vargas H, Arnell T, et al. Nonoperative management of perforated appendicitis without periappendiceal mass. Am J Surg. 2000; 179:177–181.
7. Jeffrey RB Jr, Federle MP, Tolentino CS. Periappendiceal inflammatory masses: CT-directed management and clinical outcome in 70 patients. Radiology. 1988; 167:13–16.
8. Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992; 58:264–269.
9. Siewert B, Raptopoulos V, Liu SI, Hodin RA, Davis RB, Rosen MP. CT predictors of failed laparoscopic appendectomy. Radiology. 2003; 229:415–420.
10. Liu SI, Siewert B, Raptopoulos V, Hodin RA. Factors associated with conversion to laparotomy in patients undergoing laparoscopic appendectomy. J Am Coll Surg. 2002; 194:298–305.
11. Puylaert JB, Rutgers PH, Lalisang RI, de Vries BC, van der Werf SD, Dörr JP, et al. A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med. 1987; 317:666–669.
12. Borushok KF, Jeffrey RB Jr, Laing FC, Townsend RR. Sonographic diagnosis of perforation in patients with acute appendicitis. AJR Am J Roentgenol. 1990; 154:275–278.
13. Quillin SP, Siegel MJ, Coffin CM. Acute appendicitis in children: value of sonography in detecting perforation. AJR Am J Roentgenol. 1992; 159:1265–1268.
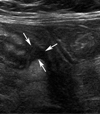
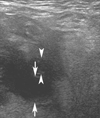
14. Choi GC, Kim S, Im HH, Lee SJ, Yang SB, Lee SW, et al. High-resolution ultrasonography of appendiceal specimens: differentiation of acute non-perforated appendicitis from perforated appendicitis. J Korean Soc Ultrasound Med. 2007; 26:145–153.
15. Abu-Yousef MM, Bleicher JJ, Maher JW, Urdaneta LF, Franken EA Jr, Metcalf AM. High-resolution sonography of acute appendicitis. AJR Am J Roentgenol. 1987; 149:53–58.
16. Gaensler EH, Jeffrey RB Jr, Laing FC, Townsend RR. Sonography in patients with suspected acute appendicitis: value in establishing alternative diagnoses. AJR Am J Roentgenol. 1989; 152:49–51.
17. Jeffrey RB Jr, Laing FC, Lewis FR. Acute appendicitis: high-resolution real-time US findings. Radiology. 1987; 163:11–14.
18. Jeffrey RB Jr, Laing FC, Townsend RR. Acute appendicitis: sonographic criteria based on 250 cases. Radiology. 1988; 167:327–329.
19. Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986; 158:355–360.
20. Lee JH, Jeong YK, Park KB, Park JK, Jeong AK, Hwang JC. Operator-dependent techniques for graded compression sonography to detect the appendix and diagnose acute appendicitis. AJR Am J Roentgenol. 2005; 184:91–97.
21. Tsuboi M, Takase K, Kaneda I, Ishibashi T, Yamada T, Kitami M, et al. Perforated and nonperforated appendicitis: defect in enhancing appendiceal wall--depiction with multi-detector row CT. Radiology. 2008; 246:142–147.







 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download