Abstract
Purpose
To evaluate factors which affect the longevity of tunneled central venous catheters (T-CVCs).
Materials and Methods
A retrospective study was conducted on 363 T-CVCs. We evaluated the relevant factors affecting the longevity of the T-CVCs, such as age, gender, indication for catheterization, site of entry vessel, diameter and type of T-CVC, catheter tip position, and underlying diseases.
Results
Of the 363 T-CVCs which had been inserted, 331 (91%) were placed through the right internal jugular vein (RIJV). The catheter tip position was the strongest predictor for the longevity of the T-CVC. The short limb of the catheter tip placed either at the cavoatrial junction (CA junction) or below the lower margin of the right main bronchus had a good prognosis. The vessel through which the T-CVC was placed significantly influenced the longevity of the T-CVC; the RIJV was associated with better results than the left internal jugular vein. Also, a split-type catheter was significantly associated with a better result.
Nowadays, one of the most commonly performed vascular interventional procedures is the insertion of tunneled central venous catheters (T-CVCs). Greater than 70% of patients beginning chronic hemodialysis in the United States have a T-CVC as their first blood access device (1). The primary indications for tunneled dialysis catheters are in those patients who cannot have a fistula, graft or peritoneal catheter (2). Also, T-CVCs have gained increasing acceptance for multiple uses, including long-term access for patients without peripheral access, total parenteral nutrition, and administration of chemotherapeutic agents, antibiotics, and fluids (3). However during the catheterization, many complications occur; particularly catheter related bacteremia and sepsis, blockage and malfunction (either by thrombus or fibrin sheath), as well as malposition and migration (4). In addition, repeated re-positioning of T-CVCs may also be responsible for interruptions or delays in medical treatment. In spite of these limitations, long-term placement of T-CVCs is increasingly required due to increased dependency on T-CVCs during medical treatment (15). Since the first description by Schwab et al in 1988, a number of differing designs of T-CVCs have evolved to minimize problems associated with their use (4). As results, various patterns of the catheter tip and lumen have been modified to improve catheter function.
In general, most procedures are done under Kidney Disease Outcomes Quality Initiative (K/DOQI) guideline (6). According to the K/DOQI guidelines, a catheter tip should be adjusted to the level of the caval atrial junction or into the right atrium (RA); catheter choice may be based on local experience, goals for use, and cost. Aside from the K/DOQI guidelines for hemodialysis, there is no more detailed information in the literature providing guidance to medical personnel regarding the T-CVC procedure for purposes other than hemodialysis.
In this study we report the results from an audit of all tunneled catheter insertions performed under various purposes at our institution over a three year period. We have evaluated the outcomes and complications of three different catheters. The purpose of the current study was to evaluate the factors determining the longevity of T-CVCs with a focus on the catheter tip position.
Three hundred sixty-three T-CVCs were inserted during the study period. The study population was comprised of 189 males (52%) and 174 females (48%). The age of the subjects ranged from 10-90 years, with a mean of 51.6 years.
A retrospective study was conducted on 363 T-CVCs (14.5F Hemo-Glide® and 14.5F HemoSplit®, Bard Access System, Salt Lake City, UT, USA and 13.5F Permcath®, Quinton, Seattle, WA, USA), which were inserted into patients at the interventional radiology suites in our institute from January 2005 to August 2008. One hundred ninety Permcath® catheters, 50 HemoGlide®, and 123 HemoSplit® catheters were inserted. Since three kinds of catheters were introduced into our hospital sequentially and the latter model replaced the former model, three subject groups by catheter model were included consecutively by time. The clinical requirements of T-CVCs were inserted either chemotherapy or hemodialysis in our institute. The number of T-CVCs for chemotherapy versus hemodialysis was 101 versus 89, 17 versus 33, and 53 versus 70 for the Permcath®, Hemoglide®, and Hemosplit® catheters, respectively. Since a single model of T-CVC was available in our institute, the T-CVC was commonly used for hemodialysis and chemotherapy. Practically, the dual lumen T-CVC was required for chemotherapy due to its mechanical stability, constant longevity, and spare lumen for either drug infusion or blood sampling.
All T-CVCs were inserted by an in-house radiologist with 8 years of experience and the choice of T-CVC design reflected what was available in the ward. The tip position of T-CVCs was originally aimed to the level of the cavoatrial (CA) junction. However, due to body size, entry position of subcutaneous tunnel, puncture level in the internal jugular vein, and the elevation level of the RA floor, the resultant position of catheter tip varied from above to below the CA junction level. The whole procedure including decision of catheter tip level was performed on supine position.
The data collected in this study included the subject's age and gender, indication for T-CVC placement, date and time of the procedure, complications, site of entry vessel, diameter and type of T-CVC, catheter tip position, and underlying pathologies, such as systemic hypertension (HTN), diabetes mellitus (DM), and congestive heart failure. All T-CVCs were dual lumens, dual catheters with longer and shorter separated limbs. The levels of the two limbs were evaluated separately.
The catheter tip position was evaluated with reference to the caval atrial junction (CAJ) and the right main bronchus (RMB) (Fig. 1). When the catheter tip was positioned at the level of the CAJ, it was recorded as the mid-level position. If the tip was positioned at the upper or lower levels in relation to the CAJ, it was recorded as the upper or lower level positions, respectively. Similarly, when the catheter tip was positioned above the upper margin, between the upper and lower margin, or below the lower margin of the RMB, it was recorded as upper, mid, or lower level positions, respectively. For follow-up of the T-CVCs, subsequent serial chest radiographs of the patients were retrospectively evaluated. When the removal of the T-CVCs was noticed, the catheter indwelling time was calculated and the cause of removal was investigated on medical records. T-CVCs were removed in cases of impaired function, peri-catheter super-infection, malposition, or no further clinical requirements.
During the statistical evaluation a "catheter failure" was declared when the function of the T-CVC was shorter than the indwelling time. The statistical analysis was performed using Cox regression analysis. In order to investigate the impact of covariates on the longevity of T-CVCs, a proportional hazard model was fitted. Patients were followed up for the lifespan of the T-CVCs and were censored when T-CVCs were removed if no longer needed. Kaplan-Meier survival curves were plotted to investigate the impact of the entry vessel, catheter tip position, and gender. All analyses were performed using PASW statistics for Windows, version 18.0 (SPSS, Inc., Chicago, IL, USA).
In this study, the majority of patients required long-term, large-bore venous catheter access for multiple reasons. The primary indications included administration of chemotherapy (n = 171) and hemodialysis (n = 192). The sites of entry included the right internal jugular vein (RIJV) in 91.2% of patients (n = 331) and the left internal jugular vein (LIJV) in 8.8% of patients (n = 32). Of the 363 T-CVCs inserted, 52.3% (n = 190) were 13.5 Fr catheters, and 47.7% (n = 173) were 14.5 Fr catheters. Of the 363 T-CVCs inserted, 66.1% (n = 240) had a dual catheter with two distinct attached circular lumens and 33.9% (n = 123) had dual catheters with two distinct and separate lumens. Of the 363 T-CVCs, the tip position of the short limb (SL) of the catheter was at the CAJ in 46.3% of the patients (n = 168) and above or below the CAJ in 34.4% (n = 125) and 19.3% of the patients (n = 70), respectively. Of the 363 T-CVCs, the tip position of the SL of the catheter was at the mid-level of the RMB in 37.7% of the patients (n = 137) and the upper or lower level of the RMB in 5.8% (n = 21) and 56.5% of the patients (n = 205), respectively (Table 1).
Of the 363 T-CVCs, 46 cases were removed unexpectedly. Among these 46 cases, 21 T-CVCs were removed due to simple occlusion of catheter lumen. Fifteen T-CVCs had to be removed by superimposed infection. In 10 cases, the catheters occluded with displaced malposition. The remaining 317 T-CVCs were censored, and for the following reasons: 142 T-CVCs were removed due to well-functioning A-V fistula or graft, 15 for recovering of native renal function, and 53 due to the conclusion of chemotherapy. Moreover, 15 patients died with functioning T-CVCs, 78 T-CVCs were still working at time of completion of audit, and 14 patients were lost to follow up.
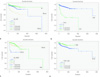
In order to investigate the impact of covariates on time-to-failure for T-CVCs, a Cox proportional hazards model was fitted and included the covariates of gender, site of entry vessel, catheter tip position, catheter type, catheter diameter, and underlying disease such as HTN and DM. The catheter tip position, entry vessel, and catheter type were important factors in determining the longevity of T-CVCs (Table 2). Placement of the short limb catheter tip at the CAJ in comparison to above or below the CAJ significantly increased the longevity of the T-CVC (p < 0.001, RR = 3.888, 95% CI 2.191-6.902). The mean survival of T-CVCs placed at the CAJ, below the CAJ, and above the CAJ were 136.7 ± 112.6 days, 98.9 ± 119.2 days and 119.6 ± 107.8 days, respectively (Fig. 2A). The site of the entry vessel was a significant predictor of increased longevity of the T-CVCs (p < 0.001, RR = 3.841, 95% CI 1.908-7.732). The mean survival of the RIJV and LIJV entry vessels were 126.1 ± 113.0 days and 96.7 ± 110.1 days, respectively (Fig. 2B). The tip of the short limb below or at the lower margin of the RMB in comparison to above the lower margin of the RMB significantly increased the longevity of T-CVCs (p = 0.032, RR = 0.478, 95% CI 0.243-0.940). The mean survival of T-CVCs placed in the upper, mid, and lower levels than the lower margin of RMB were 61.4 ± 69.1 days, 121.2 ± 98.9 days, and 131.4 ± 123.1 days, respectively (Fig. 2C). A two distinct and separate type T-CVC increased the longevity of T-CVCs (p = 0.023, RR = 0.406, 95% CI 0.186-0.883) (Fig. 2D).
Although no statistical significance could be observed, some trends were noted in the influence of some other covariates on the longevity of T-CVCs in this study. A trend that male gender was better for the longevity of T-CVCs than female was observed as mean longevities of 135.0 ± 114.8 days and 111.0 ± 109.7 days, respectively. The longevities of T-CVCs by the three age groups (younger than 50 years, from 50 to 70 years, older than 70 years) were 134.0 ± 103.1 days, 119.0 ± 117.3 days, and 106.8 ± 125.5 days, respectively. The older group showed shorter longevity of T-CVCs. However, the indications for T-CVCs did not show a trendy difference in the longevity. Compared to the mean longevity of whole T-CVCs (123.5 ± 112.9 days), the chemotherapy and hemodialysis groups showed mean longevities of 130.3 ± 83.6 days and 117.4 ± 133.6 days, respectively. The presence versus absence of HTN, DM, and congestive heart failure showed longevities of 120.3 ± 140.0 versus 126.0 ± 86.7, 122.8 ± 130.0 versus 124.0 ± 103.2, and 128.5 ± 184.6 versus 123.0 ± 101.7 days, respectively.
Catheterization with T-CVCs is one of the most commonly performed procedures in the hospital setting today. Most patients who require T-CVCs are for long-term use, such as chemotherapy and hemodialysis patients (3). Attempts to increase T-CVC longevity and preventing repeated re-insertions are therefore justified and desirable.
The present study focused on determining how many and which factors determined the longevity of T-CVCs. Petersen et al. (7) put forth the hypothesis that catheter tip positien and the diameter of the T-CVC have an important effect on T-CVC longevity. Inspite of the K/DOQI guidelines, we needed more information about catheter manipulation during T-CVC procedure.
In our institute, the puncture of the internal jugular vein under ultrasonographic (US) guidance was the routine approach and was more popular than unguided or subclavian vein punctures. The placement of T-CVC insertion via the internal jugular vein under US-guidance was performed without any early complications, such as pneumothorax or massive hematoma. A follow-up evaluation did not demonstrate procedure-related delayed complications requiring catheter removal. In the literature, concordant to our results, image-guided placement of internal jugular vein chest ports had a high success rate and a low complication rate compared with reported series of unguided subclavian vein port insertion (7). The increased longevity of the T-CVC catheters via RIJV compared to via LIJV may be due to a longer draining course from the LIJV to the superior vena cava (SVC) than from the RIJV to the SVC. Also in oncology patients, the suitability and safety of venous port implantation with catheter insertion via the RIJV has been verified (8).
In addition, catheter tip position at the site of vessel entry was another important factor affecting the longevity of the T-CVC. In our results, the use of a large diameter T-CVC, of which the short limb of the catheter tip was placed at the CAJ, significantly increased T-CVC longevity. There is controversy over the optimal catheter tip position to balance catheter performance against the risk of adverse events. Many studies suggest different catheter tip positions for different reasons. In the case of T-CVCs for hemodialysis, Ash (1) suggested placing both the removal and return lumens within the RA where the tips cannot rest against a venous wall, and only one lumen usually rests against the atrial wall. The rationale for such placement was that removal of blood through the ports of a CVC in a vein creates a negative pressure around these ports due to direct suction. Petersen et al. (7) concluded that malfunctions can be minimized by locating the catheter tip as close to the SVC/right atrial junction as possible, or slightly inside the RA. Other studies, however, have recommended that catheter tips should not be placed in the RA to avoid the risk of cardiac tamponade (9). We experienced more fibrous cap formation when the shorter limb of catheter located above the CA junction possibly due to a higher chance for catheter tip to touch the vascular wall. When both limbs of catheter located below CA junction were within RA, we experienced higher risk of cardiac arrhythmia. In addition, diaphragmatic elevation by ascites were used to elevate the floor of RA. This event increased the risk of contact between catheter tip and floor of RA which subsequently increase the risk of cardiac arrhythmia or catheter occlusion. Based on these experiences, we speculate that the short limb of a catheter at the CA junction level would support longevity of T-CVC.
The reasons why T-CVCs last longer in certain circumstances is likely related to the size of the vein into which it is placed, as borne out by the finding that the site of placement is important (10). This may also account for the finding that males are more likely to benefit from an increased T-CVC lifespan, although no statistical significance was noted in the present study. Females may have smaller caliber vein than males (1112). Certainly, there is evidence that T-CVC insertion is more difficult in females (13). In the present study, since all insertions of T-CVCs was performed under US-guidance, the success rate of puncture or the number of puncture trials did not show any difference between male and female patients. In the present study, the luminal diameter of T-CVCs did not significantly influence the longevity since large bore catheters of either 13.5 F or 14.5 F were used in all cases.
In the literature, analysis of the various substances administered, whether it was a medication or hemodialysis fluid, was also tested, and was not shown to influence the T-CVC lifespan. Administered substances, such as antibiotics, have been found to increase phlebitis in some studies (1314), but not in other studies (1516). Administered substances associated with phlebitis could affect the longevity of catheter malfunction (13); however, more detailed studies seem to demonstrate that any possible effect is limited to very specific antibiotics (17). Lifespan of indwelled central venous catheter may be curtailed for a number of reasons. This may explain why the administered substances were not factors affecting longevity in this study. Age was also found to have no effect in our study, which agreed with the reports by Malach et al. (18) and Monreal et al. (19), who analyzed age with respect to phlebitis.
The findings of this study should be considered despite its limitations. Decisions regarding the site of the entry vessel and diameter of the T-CVC were made by individual physicians as in a normal clinical setting, considering the nature of the accessible veins, as well as the physician's own individual preferences. Since no guidelines for entry vessel selection were utilized in this study, a natural bias might exist in the selection process. A second limitation of the study was that not all patients were followed until the removal of the T-CVC. Even though some patients were followed until removal of the T-CVC due to either malfunction or no further need, some patients are still using catheters. For this reason, the proportional hazard model and Kaplan-Meier survival curve analysis were performed in this study.
In conclusion, the catheter tip position, entry vessel, and catheter type were important factors in determining the longevity of T-CVCs. We recommend a two distinct and separate type T-CVC placed through the RIJV with tip position at the CAJ level for the longevity of T-CVCs.
Figures and Tables
Fig. 1
Stratification of the catheter tip position based on cavoatrial junction (CAJ) and right main bronchus (RMB).
A. First, during the procedure, the upper (arrows) and lower margins (arrowheads) of RMB are depicted under fluoroscopic guidance. Subsequently the catheter is located with a shorter limb above the upper margin of RMB and a longer limb below lower margin of RMB
B. After initial placement of the catheter along the RMB level, transcatheter angiography is performed through each catheter hub by manual injection of 10 mL of 1 : 1 iodinated contrast medium and normal saline solution. By checking the sequential opacification of superior vena cava, right atrium, right ventricle, and pulmonary artery, the tip position is adjusted based on CAJ (arrow).

Fig. 2
Kaplan-Meier survival curve analysis about the longevity of tunneled central venous catheters (T-CVCs) by the influence of statistically significant covariates.
A. The short limb level of T-CVCs at cavoatrial junction (CAJ) shows the best longevity followed by the levels below and above the CAJ. At = at the CAJ, Below = below the CAJ, Above = above the CAJ
B. T-CVCs inserted through right internal jugular vein (IJC) shows better longevity than left IJC. RIJV = right internal jugular vein, LIJV = left internal jugular vein
C. The short limb level of T-CVCs below the level of right main bronchus (RMB) shadow shows the better longevity than midlevel and above levels. Below = below the lower margin of RMB, Above = above the upper margin of RMB, Mid = between upper and lower margin of RMB
D. Split type T-CVCs shows better patency than non-split type. Split = two distinct lumens and separated type, None = two distinct lumens and non-separated type
Notes
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), which was funded by the Ministry of Education, Science and Technology (2010-000-7337) and also by the MKE (The Ministry of Knowledge Economy), Korea, under the ITRC (Information Technology Research Center) Support program supervised by the NIPA (National IT Industry Promotion Agency) [NIPA-2010-(C1090-1021-0002)].
References
1. Ash SR. Advances in tunneled central venous catheters for dialysis: design and performance. Semin Dial. 2008; 21:504–515.
2. O'Dwyer H, Fotheringham T, O'Kelly P, Doyle S, Haslam P, McGrath F, et al. A prospective comparison of two types of tunneled hemodialysis catheters: the Ash Split versus the PermCath. Cardiovasc Intervent Radiol. 2005; 28:23–29.
3. Robertson LJ, Mauro MA, Jaques PF. Radiologic placement of Hickman catheters. Radiology. 1989; 170:1007–1009.
4. Fry AC, Stratton J, Farrington K, Mahna K, Selvakumar S, Thompson H, et al. Factors affecting long-term survival of tunnelled haemodialysis catheters--a prospective audit of 812 tunnelled catheters. Nephrol Dial Transplant. 2008; 23:275–281.
5. Quarello F, Forneris G, Borca M, Pozzato M. Do central venous catheters have advantages over arteriovenous fistulas or grafts? J Nephrol. 2006; 19:265–279.
6. Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006; 48:Suppl 1. S176–S247.
7. Petersen J, Delaney JH, Brakstad MT, Rowbotham RK, Bagley CM Jr. Silicone venous access devices positioned with their tips high in the superior vena cava are more likely to malfunction. Am J Surg. 1999; 178:38–41.
8. Charvát J, Linke Z, Horáèková M, Prausová J. Implantation of central venous ports with catheter insertion via the right internal jugular vein in oncology patients: single center experience. Support Care Cancer. 2006; 14:1162–1165.
9. Darling JC, Newell SJ, Mohamdee O, Uzun O, Cullinane CJ, Dear PR. Central venous catheter tip in the right atrium: a risk factor for neonatal cardiac tamponade. J Perinatol. 2001; 21:461–464.
10. Dillon MF, Curran J, Martos R, Walsh C, Walsh J, Al-Azawi D, et al. Factors that affect longevity of intravenous cannulas: a prospective study. QJM. 2008; 101:731–735.
11. Kröger K, Ose C, Rudofsky G, Roesener J, Weiland D, Hirche H. Peripheral veins: influence of gender, body mass index, age and varicose veins on cross-sectional area. Vasc Med. 2003; 8:249–255.
12. Yang F, Minutello RM, Bhagan S, Sharma A, Wong SC. The impact of gender on vessel size in patients with angiographically normal coronary arteries. J Interv Cardiol. 2006; 19:340–344.
13. Jacobson AF, Winslow EH. Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung. 2005; 34:345–359.
14. Maki DG, Ringer M. Risk factors for infusion-related phlebitis with small peripheral venous catheters. A randomized controlled trial. Ann Intern Med. 1991; 114:845–885.
15. Haddad FG, Waked CH, Zein EF. Peripheral venous catheter-related inflammation. A randomized prospective trial. J Med Liban. 2006; 54:139–114.
16. Cornely OA, Bethe U, Pauls R, Waldschmidt D. Peripheral Teflon catheters: factors determining incidence of phlebitis and duration of cannulation. Infect Control Hosp Epidemiol. 2002; 23:249–253.
17. Uslusoy E, Mete S. Predisposing factors to phlebitis in patients with peripheral intravenous catheters: a descriptive study. J Am Acad Nurse Pract. 2008; 20:172–180.
18. Malach T, Jerassy Z, Rudensky B, Schlesinger Y, Broide E, Olsha O, et al. Prospective surveillance of phlebitis associated with peripheral intravenous catheters. Am J Infect Control. 2006; 34:308–312.
19. Monreal M, Quilez F, Rey-Joly C, Rodriguez S, Sopena N, Neira C, et al. Infusion phlebitis in patients with acute pneumonia: a prospective study. Chest. 1999; 115:1576–1580.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download