Abstract
Neurocutaneous melanosis is a rare disorder characterized by the presence of a large or multiple congenital melanocytic nevus with proliferation of melanocytes in the central nervous system. The prognosis of neurocutaneous melanosis is extremely poor and its diagnostic approach requires understanding its brain magnetic resonance imaging findings. We report a patient with asymptomatic neurocutaneous melanosis and its radiologic findings.
Figures and Tables
Fig. 1
The patient has giant hairy dark nevus covering most of back, shoulder, and posterior neck as well as multiple satellite nevus scattered over the whole body.
Fig. 2
Histopathologic findings show that nevus cells are present near and around appendages and the deep dermis (A. H&E, × 40, B. H&E, × 100).
Fig. 3
Neurocutaneous melanosis in a 20-year-old man. (A) T1-weighted MR image and (B) T2-weighted MR image show ill-defined high signal intensity lesion at the ventral part of the left side pons (arrow). (C) Gadolinium-enhanced T1-weighted MR image shows no enhancement in the ill-defined high signal intensity lesion (arrow). (D) FLAIR image shows ill-defined high signal intensity lesion at the ventral part of the left side pons (arrow).
Note.-FLAIR = fluid attenuated inversion recovery
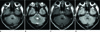
Fig. 4
Upper level of Fig. 3 in the same patient (A) T1-weighted MR image and (B) FLAIR image show high signal intensity focus at the right amygdala (arrow). (C, D) Gadolinium-enhanced T1-weighted MR image shows no enhancement in the high signal intensity focus (arrow). (E) T2-weighted MR image shows indeterminate signal intensity focus at the right amygdala.
Note.-FLAIR = fluid attenuated inversion recovery

References
1. Smith AB, Rushing EJ, Smirniotopoulos JG. Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics. 2009; 29:1503–1524.
2. Vanzieleghem BD, Lemmerling MM, Van Coster RN. Neurocutaneous melanosis presenting with intracranial amelanotic melanoma. AJNR Am J Neuroradiol. 1999; 20:457–460.
3. Ye BS, Cho YJ, Jang SH, Lee BI, Heo K, Jung HH, et al. Neurocutaneous melanosis presenting as chronic partial epilepsy. J Clin Neurol. 2008; 4:134–137.
4. Agero AL, Benvenuto-Andrade C, Dusza SW, Halpern AC, Marghoob AA. Asymptomatic neurocutaneous melanocytosis in patients with large congenital melanocytic nevi: a study of cases from an Internet-based registry. J Am Acad Dermatol. 2005; 53:959–965.
5. Hsueh CW, Ho CS, Chiu NC, Shen EY. Neurocutaneous melanosis with hydrocephalus: report of one case. Acta Neurol Taiwan. 2004; 13:29–33.
6. Hayashi M, Maeda M, Maji T, Matsubara T, Tsukahara H, Takeda K. Diffuse leptomeningeal hyperintensity on fluid-attenuated inversion recovery MR images in neurocutaneous melanosis. AJNR Am J Neuroradiol. 2004; 25:138–141.
7. Warakaulle DR, Anslow P. Differential diagnosis of intracranial lesions with high signal on T1 or low signal on T2-weighted MRI. Clin Radiol. 2003; 58:922–933.
8. Bittencourt FV, Marghoob AA, Kopf AW, Koenig KL, Bart RS. Large congenital melanocytic nevi and the risk for development of malignant melanoma and neurocutaneous melanocytosis. Pediatrics. 2000; 106:736–741.
9. DeDavid M, Orlow SJ, Provost N, Marghoob AA, Rao BK, Wasti Q, et al. Neurocutaneous melanosis: clinical features of large congenital melanocytic nevi in patients with manifest central nervous system melanosis. J Am Acad Dermatol. 1996; 35:529–538.
10. Chu WC, Lee V, Chan YL, Shing MM, Chik KW, Li CK, et al. Neurocutaneous melanomatosis with a rapidly deteriorating course. AJNR Am J Neuroradiol. 2003; 24:287–290.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download