Abstract
Purpose
To compare digital tomosynthesis with endoscopic retrograde cholangiopancreatography (ERCP) for the evaluation of common bile duct (CBD) stones as a complementary diagnostic tool.
Materials and Methods
Ninety six consecutive patients clinically suspected of having CBD stones underwent ERCP and digital tomosynthesis over 22 months, from December, 2008 to May, 2010. Fourteen patients were excluded. Therefore 82 patients were included in this study. The images were retrospectively reviewed to compare the results with the final analysis based on the consensus of two abdominal radiologists. An evaluation of the presence of CBD stones was followed by a determination of the margins for the stones, scored with a five-point conspicuity scale.
Results
Among the 82 patients, 54 collectively had 89 CBD stones and 28 had no stones. The sensitivity and specificity for the detection of CBD stones were 91.0% and 80.6% for ERCP, 92.1% and 93.5% for digital tomosynthesis, respectively. The average score was 3.29 for ERCP and 3.89 for digital tomosynthesis in 77 similar detected stones. Digital tomosynthesis demonstrated significantly better conspicuity than ERCP (p = 0.001).
Digital tomosynthesis generates slice images using conventional X-ray and offers several advantages over conventional projection radiography. For example, tomographic imaging allows for the determination of depth and improves the conspicuity of structures by removing the visual untidiness associated with the overlying anatomy. It also provides better contrast of local structures by limiting the overall image dynamic range to that of a single slice (123). Earlier conventional geometric tomography found limited use of this method because of image blurring, excessive radiation dose, and a long image-acquisition time. However, digital tomosynthesis overcomes these limitations by enabling the reconstruction of the numerous slices obtained from the patient based on the low-dose acquisition of data from a single imaging session (14).
Tomosynthesis also allows for an arbitrary number of in-focus planes to be generated retrospectively from a sequence of projection radiographs acquired during a single motion of the X-ray tube. By adding and shifting these projection radiographs, specific planes can be reconstructed (12345). Furthermore, with the introduction of flat-panel imaging systems, a digital detector is now available that has all the properties necessary for clinically practical tomosynthesis (1234). With these advanced techniques, a large number of low-dose projection images can be rapidly acquired.
There is growing interest in digital tomosynthesis for a number of clinical applications including chest imaging, mammography, orthopedic imaging, angiography, and dental imaging (2). By contrast, although digital tomosynthesis might be a valuable tool in abdominal imaging, especially for the pancreaticobiliary system, little has been published on clinical trials for abdominal tomosynthesis. Endoscopic retrograde cholangiopancreatography (ERCP) has been widely used for diagnostic purposes and for removal procedures, such as for the common bile duct (CBD) stones.
Therefore, the aim of the present study was to compare the digital tomosynthesis with ERCP to evaluate common bile duct stones as a complementary diagnostic tool, focusing on their detection and conspicuity.
This study was approved by the Institutional Review Board. The study population consisted of 96 consecutive patients (56men, 40 women; mean age: 62.1 years; age range; 16-92 years), clinically suspected of having CBD stones, and underwent ERCP as well as digital tomosynthesis concurrently over 22 months, from December, 2008 to May, 2010. Among the 96 patients, 14 were excluded because of massive pneumobilia (n = 9), poor quality of the obtained images due to incomplete study (n = 3), multiple (> 10) stones (n = 2). Consequently, 82 patients were included in this study.
Digital tomosynthesis with a digital FPD R/F X-ray system (Sonialvision Safire, Shimadzu, Japan) was acquired by continuous fluoroscopic exposure from top to bottom with a 40° range and the target as the center of the CBD. Images collected with 36 frames and a 768 × 768 matrix were reconstructed to a 2 mm thickness interval with filtered back projection. To focus on the CBD, the target point was made at a 120 mm depth from the skin with a 70 mm buffer in all directions and continuous X-ray exposure for 2.5 seconds (Fig. 1). ERCP and digital tomosynthesis were performed with the patient under conscious sedation. Every patient underwent an endoscopical stone removal procedure during ERCP.
The images were retrospectively reviewed to compare the results with the final analysis based on the consensus of two abdominal radiologists. An evaluation of the presence of CBD stones was followed by a determination of the margins of the stones, as scored by a five-point conspicuity scale. The five-point scale was defined by degree of conspicuity of CBD stones as the range of clear margin (1: 0-¼ of circumference, 2: ¼-½ of circumference, 3: ½-¾ of circumference, 4: ¾-entire of circumference, 5: entire circumference). We regarded the results of the stone-removal procedure as the gold standard for stone detection.
Statistical analyses were performed with using SPSS (release 17.0.2; SPSS Inc., Chicago, IL, USA). The sensitivity and specificity of ERCP and digital tomosynthesis for the detection of the CBD stones were calculated. The means of the scores were compared using a two-tailed paired t-test. The data were reported herein as the means and standard deviations. A p-value < 0.05 was considered to indicate statistically significance.
On the basis of the final diagnosis obtained from endoscopic stone removal, 54 of the 82 patients collectively had 89 CBD stones, while the remaining 28 had no stones. ERCP successfully detected 81 of the 89 stones while digital tomosynthesis detected 82 stones; 77 stones were detected by both methods, whereas 4 stones were detected only on ERCP and 5 stones only on digital tomosynthesis. There were 6 false-positive cases using ERCP (Fig. 2), but only 2 using digital tomosynthesis. Moreover, there were 8 false-negative cases on ERCP (Fig. 3), and 7 on digital tomosynthesis (Table 1). The sensitivity and specificity for CBD stone detection were 91.0% and 80.6% for ERCP, and 92.1% and 93.5% for digital tomosynthesis, respectively (Table 2).
The margins of the 77 concurrently detected stones were evaluated for conspicuity according to the 5-point scale. The results are shown in Table 3. The average score was 3.29 for ERCP and 3.89 for digital tomosynthesis. In the evaluation of the stones' margins, digital tomosynthesis demonstrated a statistically superior conspicuity compared to ERCP (p = 0.001) (Table 4). Forty-four stones were seen more clearly by digital tomosynthesis and thus had a higher score than ERCP (4.3 vs 2.9) (Fig. 4). In contrast, twelve stones were detected with a higher score on ERCP than digital tomosynthesis (3.8 vs. 2.8) (Fig. 5), while 21 stones were seen equally well by both ERCP and digital tomosynthesis (Fig. 6).
The symptoms and signs of common bile duct stones include right upper quadrant abdominal pain, jaundice, fever, and biochemical abnormality. A more serious complication is cholangitis, which, if progressive, and can lead to septic shock with a high mortality. Thus, the early diagnosis of CBD stones is important, and their subsequent removal is recommended.
Currently, there are several modalities to detect common bile duct stones including abdominal ultrasound, endoscopic ultrasound, MRI with magnetic resonance cholangiopancreatography (MRCP), ERCP, and computed tomography (CT), which included computed tomographic cholangiography (CTC).
The traditional first-line modality, abdominal ultrasound, is operator-dependent and has a wide-ranging sensitivity (20-80%) (6789). Endoscopic ultrasound is considered as an alternative method, but it is an invasive procedure that is not only operator-dependent but also accompanied by the potential for endoscopy-related complications (10).
CT and CTC yield high-resolution images of the biliary tree and adjacent anatomic structures with low invasiveness, but both require relatively high doses of ionizing radiation (11) in addition to intravenous contrast medium (1213). MRCP is not invasive. Moreover, because diagnostic accuracy does not depend on the skill of the operator, more objective results can be obtained. Many studies have confirmed the high sensitivity of MRCP for detecting CBD stones (14151617). However, MRCP cannot be used in patients who are claustrophobic or who have implanted devices, such as internal cardioverters, pacemakers, or metallic clips for cerebral aneurysms. Furthermore, MRCP has several potential pitfalls including patients with tortuous common bile ducts, compression of the hepatic duct by the right hepatic artery, an origin of the cystic duct mimicking CBD stones, or pneumobilia (17).
For these reasons, ERCP has become the standard diagnostic and therapeutic technique in the evaluation of the pancreaticobiliary tract. However, it is an invasive procedure with a mortality rate of 1-2% (181920212223). Despite its invasiveness, ERCP is widely performed, as it not only accurately detects the presence of stones, but also allows for simultaneous treatment, such as extraction.
In our study, during the ERCP procedure, digital tomosynthesis was conducted concurrently, without the need for additional preparation of the patient to determine its complementary utility in the diagnosis of CBD stones. Tomographic imaging has several advantages such as improved conspicuity and contrast with local structures which offer more accurate diagnosis of CBD stones during the ERCP procedure (1). A drawback in our patient series was the need for conscious sedation during ERCP and digital tomosynthesis, which resulted in the blurring of some images because patients could not perform a spontaneous breath hold during the procedure. In this situation, the higher conspicuity and contrast of local structures achieved with tomographic imaging are likely to improve CBD stone diagnosis.
Our findings demonstrated the sensitivity and specificity of digital tomosynthesis, both of which were slightly higher than those of ERCP with respect to the detection of CBD stones. In terms of conspicuity, the mean score obtained with digital tomosynthesis was significantly higher than that obtained with ERCP, suggesting that digital tomosynthesis is a superior modality to ERCP in the evaluation of CBD stones. Moreover, our findings showed that digital tomosynthesis can better depict the size and extent of CBD stones during the procedure and thus allows a more appropriate treatment choice. Additionally, digital tomosynthesis resulted in fewer false-positive cases than did ERCP, implying that digital tomosynthesis can avoid unnecessary stone-removal procedures. Hence, digital tomosynthesis can be a complementary diagnostic tool for the evaluation of CBD stones during ERCP.
This study has some limitations. First, because some patients were referred for an ERCP examination without a previous non-invasive diagnostic examination, such as MRCP or CT, only 54 of the 82 patients actually had CBD stones. Thus, a relatively small number of patients with CBD stones were evaluated. Further studies with more cases are needed to confirm the clinical usefulness of digital tomosynthesis for applications involving the biliary ductal system. Second, a method to distinguish air in the CBD from a stone is still lacking. This is potentially problematic, as biliary air might be confused with biliary calculi. However, differentiation is usually possible because biliary air moves into a nondependent position when the patient's position is changed, whereas calculi tend to localize in a dependent position.
In conclusion, the advantages of digital tomosynthesis over ERCP in the diagnosis of CBD stones include fewer false positive cases and a higher conspicuity score. Digital tomosynthesis is an effective and complementary diagnostic method to evaluate CBD stones, with clinical usefulness in imaging of the biliary ductal system.
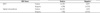
Figures and Tables
Fig. 1
Mimetic diagram of digital tomosynthesis.
Digital tomosynthesis image acquired by continuous fluoroscopic exposure from top to bottom at a range of 40°, and with the target part as the center of the CBD. To focus the CBD, the target point is set at a depth of 120 mm from the skin with 70 mm buffer in all directions and continuous X-ray exposure for 2.5 seconds.
Note.-CBD = common bile duct

Fig. 2
A 79-year-old man without a CBD stone.
A. ERCP image obtained after injection of contrast material showing a CBD stone (arrow), which is considered to be a score of 5.
B. Although the digital tomosynthesis image is slightly blurred, no definite stones are seen in the CBD.
Note.-CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography
Fig. 3
A 70-year-old man with one stone in the proximal CBD.
A. On ERCP image, no definite CBD stone is visualized.
B. Digital tomosynthesis image showing a proximal CBD stone (arrow) with a score of 3 because the upper margin of the CBD stone is obscured.
Note.-CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography
Fig. 4
A 66-year-old man with two proximal CBD stones.
A. ERCP image obtained after injection of contrast material showing 2 CBD stones (arrows) which are considered to have a score of 2 (upper stone) and 3 (lower stone).
B. Digital tomosynthesis image showing 2 CBD stones (arrows) more clearly compared with the visualization in (A), considered as score to have a 5 for both stones.
Note.-CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography

Fig. 5
A 74-year-old woman with a CBD stone.
A. ERCP image clearly showing a CBD stone (arrow) with a score of 5.
B. Digital tomosynthesis image showing the presence of a stone (arrow) in the proximal CBD with blurring of the margin, considered to have a score of 4.
Note.-CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography
Fig. 6
A 47-year-old woman with a CBD stone.
CBD stone (arrow) clearly seen on both the ERCP image (A) and digital tomosynthesis image (B) with a score of 5.
Note.-CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography

References
1. Dobbins JT 3rd, Godfrey DJ. Digital x-ray tomosynthesis: current state of the art and clinical potential. Phys Med Biol. 2003; 48:R65–R106.
2. Vikgren J, Zachrisson S, Svalkvist A, Johnsson AA, Boijsen M, Flinck A, et al. Comparison of chest tomosynthesis and chest radiography for detection of pulmonary nodules: human observer study of clinical cases. Radiology. 2008; 249:1034–1041.
3. Tingberg A. X-ray tomosynthesis: a review of its use for breast and chest imaging. Radiat Prot Dosimetry. 2010; 139:100–107.
4. Dobbins JT 3rd, McAdams HP. Chest tomosynthesis: technical principles and clinical update. Eur J Radiol. 2009; 72:244–251.
5. Dobbins JT 3rd, McAdams HP, Godfrey DJ, Li CM. Digital tomosynthesis of the chest. J Thorac Imaging. 2008; 23:86–92.
6. Pasanen P, Partanen K, Pikkarainen P, Alhava E, Pirinen A, Janatuinen E. Ultrasonography, CT, and ERCP in the diagnosis of choledochal stones. Acta Radiol. 1992; 33:53–56.
7. Pickuth D, Spielmann RP. Detection of choledocholithiasis: comparison of unenhanced spiral CT, US, and ERCP. Hepatogastroenterology. 2000; 47:1514–1517.
8. Rickes S, Treiber G, Mönkemüller K, Peitz U, Csepregi A, Kahl S, et al. Impact of the operator's experience on value of high-resolution transabdominal ultrasound in the diagnosis of choledocholithiasis: a prospective comparison using endoscopic retrograde cholangiography as the gold standard. Scand J Gastroenterol. 2006; 41:838–843.
9. Stott MA, Farrands PA, Guyer PB, Dewbury KC, Browning JJ, Sutton R. Ultrasound of the common bile duct in patients undergoing cholecystectomy. J Clin Ultrasound. 1991; 19:73–76.
10. Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005; 54:271–275.
11. Breen DJ, Nicholson AA. The clinical utility of spiral CT cholangiography. Clin Radiol. 2000; 55:733–739.
12. Persson A, Dahlström N, Smedby O, Brismar TB. Three-dimensional drip infusion CT cholangiography in patients with suspected obstructive biliary disease: a retrospective analysis of feasibility and adverse reaction to contrast material. BMC Med Imaging. 2006; 6:1.
13. Nilsson U. Adverse reactions to iotroxate at intravenous cholangiography. A prospective clinical investigation and review of the literature. Acta Radiol. 1987; 28:571–557.
14. Griffin N, Wastle ML, Dunn WK, Ryder SD, Beckingham IJ. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the diagnosis of choledocholithiasis. Eur J Gastroenterol Hepatol. 2003; 15:809–813.
15. Kim TK, Kim BS, Kim JH, Ha HK, Kim PN, Kim AY, et al. Diagnosis of intrahepatic stones: superiority of MR cholangiopancreatography over endoscopic retrograde cholangiopancreatography. AJR Am J Roentgenol. 2002; 179:429–434.
16. Stiris MG, Tennøe B, Aadland E, Lunde OC. MR cholangiopancreaticography and endoscopic retrograde cholangiopancreaticography in patients with suspected common bile duct stones. Acta Radiol. 2000; 41:269–272.
17. Kats J, Kraai M, Dijkstra AJ, Koster K, Ter Borg F, Hazenberg HJ, et al. Magnetic resonance cholangiopancreaticography as a diagnostic tool for common bile duct stones: a comparison with ERCP and clinical follow-up. Dig Surg. 2003; 20:32–37.
18. Kessler RE, Falkenstein DB, Clemett AR, Zimmon DS. Indications, clinical value and complications of endoscopic retrograde cholangiopancreatography. Surg Gynecol Obstet. 1976; 142:865–870.
19. Silviera ML, Seamon MJ, Porshinsky B, Prosciak MP, Doraiswamy VA, Wang CF, et al. Complications related to endoscopic retrograde cholangiopancreatography: a comprehensive clinical review. J Gastrointestin Liver Dis. 2009; 18:73–82.
20. Rieger R, Wayand W. Yield of prospective, noninvasive evaluation of the common bile duct combined with selective ERCP/sphincterotomy in 1390 consecutive laparoscopic cholecystectomy patients. Gastrointest Endosc. 1995; 42:6–12.
21. Vitale GC, Larson GM, Wieman TJ, Cheadle WG, Miller FB. The use of ERCP in the management of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 1993; 7:9–11.
22. Cotton PB. Endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Am J Surg. 1993; 165:474–478.
23. Shiozawa S, Kim DH, Usui T, Tsuchiya A, Masuda T, Inose S, et al. Indication of endoscopic retrograde cholangiography by noninvasive predictive factors of common bile duct stones before laparoscopic cholecystectomy: a prospective clinical study. Surg Laparosc Endosc Percutan Tech. 2011; 21:28–32.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download