Abstract
Magnetic Resonance-guided Focused Ultrasound Surgery (MRgFUS) is a clinically effective, non-invasive treatment for thermal ablation of various soft tissue tumors, and is effective in pain palliation following radiation therapy, as has been demonstrated in the initial studies of bone metastases. The current study evaluated the safety and clinical efficacy of MRgFUS for pain palliation prior to radiation therapy, in a patient with a solitary metastatic bone lesion. This is the first case report of MRgFUS treatment with a 1-year follow-up in a patient.
Magnetic Resonance-guided Focused Ultrasound Surgery (MRgFUS) is a non-invasive thermo-ablative technique for the treatment of various benign and malignant soft tissue and bone tumors, using focused ultrasound under real-time magnetic resonance imaging (MRI) guidance and control (1). This method of thermal ablation has proved effective in more than 5,000 uterine fibroid treatments and in more than 500 treatments of various other tumors (2).
Recently, MRgFUS was tested for the palliation of pain caused by bone metastases, utilizing the acoustic properties of bone for absorption of ultrasonic energy to achieve palliation and has yielded very promising initial results (34). Applying acoustic energy on the bone surface allows the creation of temperature rise in the part of the bone cortex enclosed in the beam path zone, thus indirectly ablating the adjacent periosteum and tumor tissue (4). Since the periosteum is considered to be a major source of pain in patients with metastatic bone lesions, ablating the source of pain should produce lasting pain relief. High absorption of energy in the bone allows using lower energies (compared to soft tissue MRgFUS treatment), thereby enhancing the safety profile of this procedure. Thus, MRgFUS offers a novel, alternative treatment option for painful bone metastases.
The present report briefly discusses the successful use of this novel technique for pain palliation in bone metastasis in a single patient who did not receive any radiation therapy prior the MRgFUS treatment, and who was followed long-term for a period of one year.
A 62-year-old female with breast cancer presented with a solitary, painful osteoblastic bone metastasis in her left scapula. She had been diagnosed with breast cancer 10 years ago and radical mastectomy had been performed. Her oncologist referred her to our clinic for pain palliation with MRgFUS treatment since the patient was unable to take analgesics due to liver cirrhosis secondary to Hepatitis C viral infection. Despite significant pain, the patient refused the first-line radiation therapy. In order to evaluate the patient's suitability for MRgFUS treatment, computed tomography (CT) and MR images were acquired and evaluated. CT images showed an osteoblastic lesion in the left scapula which was device accessible (Fig. 1). T2-weighted MR images showed hypointensity in most of the left scapula and nearby soft tissue. The lesion was clearly seen on MR images and it was determined to be accessible to the ultrasonic beam of the MRgFUS device (no scars or healthy bone were present in the path of the acoustic energy). After explaining the risks and benefits of this novel technique for pain palliation in bone metastases to the patient, she decided to undergo MRgFUS treatment and provided written informed consent for the procedure.
The patient was asked to complete a standard 11-point pain scale questionnaire (with 0 representing no pain at all and 10 representing the worst pain imaginable) to evaluate her average pain score prior to treatment. The patient's average pain score in the area of the left scapula was 7, during the screening procedure. The patient also reported reduced mobility of her left arm due to the severe pain caused by metastasis in the scapula. The patient did not take any medication for pain control.
The patient underwent MRgFUS treatment to control the pain from bone metastases. The treatment was performed using the MRgFUS system (ExAblate® 2000, InSightec Ltd, Haifa, Israel) integrated with an MRI scanner (GE 1.5-T MRI, Healthcare, Milwaukee, WI, USA). The ExAblate® 2000 system consists of a multi-element focused ultrasound transducer and motion system, which is fully integrated with a conventional diagnostic 1.5 or 3 Tesla MRI scanner. The ExAblate® device is an integrated component of the MR table and provides real-time therapy planning algorithm, thermal dosimetry, and closed-loop therapy control.
On the day of treatment, the patient reported increased pain for the past few days prior to treatment, and her average pain score was 8. Patient preparation prior to treatment included insertion of the intravenous line to provide conscious sedation and wrapping the patient's legs with compression stockings to reduce the risk of deep vein thrombosis from prolonged lying down. The patient was then positioned supine on the ExAblate® table, feet first, with the left scapula centered on the acoustic coupling gel pad above the ultrasound transducer. During the treatment, the patient received sedative and analgesic medications intravenously, to reduce anxiety and pain associated with the treatment (Remifentanil 1 mg mixed in 1,000 mL normal saline, 360 mL on a slow drip, 130-150 mL/hour). MR T2-weighted images were acquired for treatment planning (Fig. 2). The outline of bone cortex of the targeted bone as well as the skin line and the area to be treated were carefully drawn on the planning images. The system automatically compiled the optimal treatment plan, covering the lesion area with a series of ultrasonic spots (sonications). The treatment included 29 sonications with an average energy of 1,450 J per sonication (700-1,850 J). During each sonication, the system displayed the calculated temperature elevation in the target area as well as the acquired real time MR anatomical images to ensure patient immobility (Fig. 2). The overall duration of sonication was 1 hour and 45 minutes.
Immediately following treatment, T2-weighted and contrast enhanced T1-weighted images were acquired to evaluate treatment effectiveness. These images revealed areas of non-perfusion in the treated area and soft tissue edema adjacent to the treated lesion, including the inner part of the scapula in the areas where the bone was thin (Fig. 3). The patient reported sensations of mild pain during the treatment, which correlated well with the energy delivery site at that time. Immediately following treatment, the patient reported improvement in the mobility of the left arm. She was discharged on the same day, after a brief recovery from conscious sedation (approximately 30 minutes). Neither procedure nor device-related adverse events were reported during the treatment.
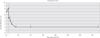
One day after treatment, the patient reported (via a telephone call) a dramatic reduction in the left scapular pain, with an average pain score of 5. The patient was followed for 1 year post-treatment, and reported an average pain score of 5, 4, 3, 2, 2, and 2 on the 3 day, 1 week, 2 week, 1 month, 3 month and
1 year follow-up visits, respectively (Fig. 4). She also reported a significant improvement in arm mobility and stated that she could perform the movements which she was unable to perform prior to treatment. During the entire follow-up period, the patient did not take any pain medication, and no adverse events were reported.
The increased incidence of cancer over the past decade, combined with improvements in the therapeutic management of cancer patients has contributed to a dramatic increase in the number of patients suffering from bone metastases. Thirty percent of cancer patients develop bone metastases during progressive stages of the disease (5) and at least 50% of them will suffer from pain caused by these metastatic lesions (6). Current treatments for patients with bone metastases are primarily palliative and include systemic therapies such as analgesics, chemotherapy, hormonal therapy and bisphosphonates as well as targeted therapies such as radiation, radio frequency ablation and stabilization surgeries (789). Although the standard of care for localized pain associated with bone metastases is palliative external beam radiation therapy (EBRT), 20-30% of patients treated with palliative radiation do not experience any pain relief (10). For those patients in whom the pain subsides, 27% experience a recurrence of pain, but they may be ineligible for subsequent radiation treatments due to high toxicity to the healthy tissues from previous treatments. Such patients resort to an increased dosage of their pain relieving medications, thereby decreasing their quality of life further.
One of the most significant factor that positively influences the quality of life for patients suffering from bone metastases is pain reduction. The encouraging results of the current case report support MRgFUS as a long-lasting, novel, non-invasive, non-ionizing, controlled and accurate treatment for pain reduction caused by bone metastases. The treatment was completed without complications and the patient showed significant clinical and symptomatic improvement following treatment, as indicated by a reduction in the pain score and a reported increase in arm mobility. The results of the case study reported here are consistent with previous studies (34), and suggest that MRgFUS may be a long-lasting, promising alternative to radiation treatment or other therapies for oncology patients who suffer from pain due to bone metastases. MRgFUS can be performed in an ambulatory setting using conscious sedation for most patients. Moreover, MRgFUS has no limitations on the permitted dose and can be administered repeatedly, if required. The current findings are particularly compelling given the fact that this case study is the first to report the successful treatment of a patient with painful bone metastases with a long-term follow-up period of one year.
Additional randomized studies are currently underway to evaluate the safety and effectiveness of this therapeutic modality in a larger cohort of patients as well as its effect as a first-line therapy, (prior to EBRT). Currently, there is no clinical data on the difference between the MRgFUS treatment prior to radiation and as a first-line therapy. Another issue that requires additional investigation is the economical feasibility of using MRgFUS for pain palliation in bone metastases. Treatment cost, during the time of health care cuts and in an era where single fractionation for the same indication is gaining more and more popularity, might be a significant obstacle for the widespread adoption of this technique. Nevertheless, given the many advantages of MRgFUS, the benefits of the procedure may far outweigh the costs.
In conclusion, we believe that MRgFUS is a novel, non-invasive procedure, which may provide a unique solution for patients with painful bone metastases. MRgFUS has the potential for treating patients who have either failed to respond favorably to radiation treatment or as a first-line therapy. Although the evidence to date is promising, further clinical trials are required to establish the safety and efficacy of MRgFUS for long-term pain palliation in bone metastases.
Figures and Tables
Fig. 1
Axial CT images of the targeted bone metastatic lesion in the left scapula (circles) before treatment (left) and at 3 months after MRgFUS treatment (right). Compared with the image before MRgFUS treatment, the targeted lesion showed a more sclerotic pattern on follow-up CT images.
Note.-MRgFUS = Magnetic Resonance-guided Focused Ultrasound Surgery

Fig. 2
An example of sonication during treatment. The left image shows the T2-weighted MR image of sonication to the left scapula for treatment planning. The right MR image shows the thermal map following sonication. The central image shows the calculated temperature elevation during this sonication, which reached a maximum of 69℃.

Fig. 3
Treatment outcome - Left: Axial T1 with Fat Sat and with contrast MR image of the targeted bone metastatic lesion in the left scapula prior to MRgFUS treatment. Right: Axial T1 with Fat Sat and with contrast MR image of the targeted bone metastatic lesion in the left scapula immediately after MRgFUS treatment, showing non-perfusion in the soft tissue surrounding the scapula. Left scapula is marked with a circle.
Note.-MRgFUS = Magnetic Resonance-guided Focused Ultrasound Surgery
References
1. Hynynen K. MRI-guided focused ultrasound treatments. Ultrasonics. 2010; 50:221–229.
2. Taran FA, Tempany CM, Regan L, Inbar Y, Revel A, Stewart EA. MRgFUS Group. Magnetic resonance-guided focused ultrasound (MRgFUS) compared with abdominal hysterectomy for treatment of uterine leiomyomas. Ultrasound Obstet Gynecol. 2009; 34:572–578.
3. Gianfelice D, Gupta C, Kucharczyk W, Bret P, Havill D, Clemons M. Palliative treatment of painful bone metastases with MR imaging--guided focused ultrasound. Radiology. 2008; 249:355–363.
4. Liberman B, Gianfelice D, Inbar Y, Beck A, Rabin T, Shabshin N, et al. Pain palliation in patients with bone metastases using MR-guided focused ultrasound surgery: a multicenter study. Ann Surg Oncol. 2009; 16:140–146.
5. Falkmer U, Järhult J, Wersäll P, Cavallin-Ståhl E. A systematic overview of radiation therapy effects in skeletal metastases. Acta Oncol. 2003; 42:620–633.
6. Chow E, Hoskin P, van der Linden Y, Bottomley A, Velikova G. Quality of life and symptom end points in palliative bone metastases trials. Clin Oncol (R Coll Radiol). 2006; 18:67–66.
7. Han SH, de Klerk JM, Tan S, van het Schip AD, Derksen BH, van Dijk A, et al. The PLACORHEN study: a double-blind, placebo-controlled, randomized radionuclide study with (186)Re-etidronate in hormone-resistant prostate cancer patients with painful bone metastases. Placebo Controlled Rhenium Study. J Nucl Med. 2002; 43:1150–1156.
8. Foro Arnalot P, Fontanals AV, Galcerán JC, Lynd F, Latiesas XS, de Dios NR, et al. Randomized clinical trial with two palliative radiotherapy regimens in painful bone metastases: 30 Gy in 10 fractions compared with 8 Gy in single fraction. Radiother Oncol. 2008; 89:150–155.
9. Thanos L, Mylona S, Galani P, Tzavoulis D, Kalioras V, Tanteles S, et al. Radiofrequency ablation of osseous metastases for the palliation of pain. Skeletal Radiol. 2008; 37:189–194.
10. DeVita VT Jr, Hellman S, Rosenberg SA. Cancer; Principles & Practice of Oncology. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2001. p. 2713–2729. Section 4, Chapter 52.4.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download