Abstract
Extraosseous involvement of multiple myelomas can be seen clinically or radiologically in approximately 10-20% of patients at the time of initial diagnosis and may develop in an additional 15% of patients over the course of the disease. The condition can arise in any tissue of the body and its presence has been associated with more aggressive disease, a guarded prognosis, or high-dose chemotherapy. Imaging findings of extraosseous multiple myelomas are diverse. They usually show high enhancement on contrast-medium enhanced CT scans, exhibit iso-signal intensity on both T1- and T2-weighted images, and variable 18F-fluorine deoxyglucose (FDG) uptake at PET. The disease may simulate an infectious condition since it may be concurrent with underlying multiple myelomas per se or it may occur during myeloma treatment including stem cell transplantation.
Extraosseous multiple myeloma is defined as a localized plasma cell neoplasm in soft tissue with the presence of systemic multiple myeloma. By definition, extraosseous myeloma cannot arise within bones (1). Extraosseous involvement of multiple myeloma, which can arise in any tissues, can be seen clinically or radiologically in approximately 10-20% of patients at the time of initial diagnosis and may develop in an additional 15% of patients during the course of the disease (23). Extraosseous myeloma is more common in younger myeloma patients, and is more frequent than nonsecretory myeloma and IgD myeloma (the more aggressive subtypes of myeloma) (1).
In addition to a skeletal survey, magnetic resonance (MR) imaging or 18F-fluorine deoxyglucose (FDG) PET/CT may be performed to identify occult skeletal involvement of multiple myelomas (4). Because a sizable number of patients with multiple myelomas have extraosseous involvement of the disease at initial presentation or during the follow-up imaging evaluation (with treatment including stem cell transplantation), we may encounter cases of extraosseous involvement of multiple myeloma more frequently. Thus, it is important to be familiar with the imaging findings of extraosseous myeloma involvement. The purpose of this pictorial review was to illustrate the imaging findings of the extraosseous manifestation of multiple myelomas.
A review of the medical records performed to document multiple myeloma cases with extraosseous involvement from a single tertiary hospital for 16 years from 1995 to 2010 found 11 cases from 11 consecutive patients. Of the 11 patients, six were six men and five were women (age range, 45-76 years; mean age ± standard deviation, 60 ± 8). The summary of the involved extraosseous tissues from all 11 patients included 15 organs: oropharynx, orbit, brain, lung, pleura, mediastinum (in two patients), liver (in two patients), spleen, kidney, retroperitoneum, lymph node, muscle, and breast. Extraosseous plasma-cell myelomatous involvement was confirmed histopathologically in eight of the 15 lesion sites. The involvement of the brain and lungs was confirmed by observing the presence of plasma cells in the CSF and pleural effusion, respectively. Under these conditions, abnormal lesions could be observed in the brain and lungs. The lesions in the orbit, kidney, lymph node, spleen, and muscle from three patients were not confirmed histopathologically. However, the lesions sufficiently qualified as being diagnosed as myeloma with extraosseous involvement, because the lesions manifested as newly-appearing lesions in patients with aggressive extra- and intra-osseous myeloma during the disease progress, without clinical evidence of infection, or showed a decrease in disease extent on follow-up images after chemotherapy.
The oropharynx is the most common site (80%) of extramedullary plasmacytoma. The organ can be involved even in patients who had no systemic involvement in the disease. Involvement is associated with the best long-term prognosis (5), and can be seen as a soft-tissue mass (Fig. 1) on CT scans. However, the oral cavity is occasionally involved with myeloma; plasma cell infiltration is seen in 5% of patients with multiple myeloma.
Orbital involvement by multiple myeloma is relatively rare, and approximately 60 cases of orbital involvement have been reported to date. Almost any structures in the orbit can be involved with multiple myeloma. Patients with this disease complain of proptosis, chemosis, visual acuity changes, epiphora, and diplopia. The lesion may manifest as having iso-signal intensity on both T1- and T2-weighted images and showing noticeable enhancement on contrast enhanced CT scans (Fig. 2).
The incidence of intracranial myeloma is rare, and the prognosis of meningeal and cerebral myeloma is poor (6). The leptomeninges is the most common site of intracranial mylomatous involvement. In this condition, imaging studies show diffuse enhancement or a focal enhancing nodule or mass (Fig. 3). Therefore, imaging findings may mimic meningitis or a meningioma.
Cerebral plasmacytomas manifest as an intensely and homogeneously enhancing lesion with perilesional edema.
Myeloma cases with lung involvement are rare and have a poor prognosis. The involvement is reported to demonstrate a mass or an infiltrative lesion which is indistinguishable from a lung metastatic lesion from an extra-thoracic malignancy (2) . They may appear as multiple lung nodules scattered in both lungs (Fig. 4).
There have been few cases of myeloma that involved the mediastinum (7). These lesions show relatively homogeneous enhancement following intravenous contrast-medium administration. The differential diagnoses include non-Hodgkin lymphoma, malignant thymic epithelial tumor, and small cell lung cancer. In our cases, the lesions showed mild homogenous enhancement on CT scans and little FDG uptake on PET scans (Figs. 6, 7).
Liver is most commonly involved with extraosseous myeloma in the abdomen. The involvement demonstrates two different features; hepatomegaly without focal lesion is one of its manifestations when the plasma cell infiltrates into the sinusoids. The other manifestation is a nodular form which is indistinguishable from a hepatic metastatic lesion (2). The attenuation of the nodule has been known to be lower than that of normal liver parenchyma in all phases on dynamic CT scans (8), but it is not always the case. The lesion may be hypervascular and may manifest an enhancing lesion in the arterial phase, and delayed washout on dynamic CT and MRI (Fig. 8). The hepatic lesion may show little FDG uptake at PET (Fig. 9).
The involvement of the spleen is rare in patients with multiple myeloma. Less than 1% of patients with multiple myeloma show splenomegaly (2).
The mesentery or the peritoneum is a rare site of extramedullary involvement by plasmacytoma. With this involvement, CT may exhibit discrete mass lesions (Fig. 11) or permeative and infiltrative tumor growth. The extraosseous myeloma present as mesenteric panniculitis (9). Under these conditions, abdominal CT scans showed mesenteric thickening and inhomogeneous areas of fat interspersed with soft-tissue attenuation.
Extraosseous multiple myeloma in the retroperitoneum manifests as a retroperitoneal soft-tissue mass. Also, obstructive uropathy due to encasement of the ureter may be associated (Fig. 12).
Lymph nodes are one of the most frequently involved extraosseous tissues in multiple myeloma. In one autopsy series, lymph nodes were enlarged in 12 (23%) of 52 patients with multiple myeloma (10). Imaging findings on CT scans are similar to those of lymphoma, with multiple nodal groups involved (Fig. 13).
Plasma cell tumor in the muscle independent from bone involvement is rare. In our case series, a patient had the psoas muscle was involved with extensive multiple myeloma was. In this particular case, biopsy confirmation was not performed, but the lesion showed regression after chemotherapy (Fig. 14).
Breast plasmacytomas are solid, non-tender, and well-defined masses of variable sizes. Imaging findings of breast plasma are round and well-defined masses on mammography, and solid well-demarcated masses with a homogenous echo-texture on ultrasonography (Fig. 15).
Imaging may play an important role in the management of extraosseous myelomas, because it facilitates the early diagnosis of this condition, differentiates this condition from other diseases such as infectious diseases, and evaluates the response to a certain kind of therapy. Although imaging findings of extraosseous multiple myelomas are frequently nonspecific and diverse, they can be categorized into an infiltrative soft-tissue pattern and a nodular or mass-forming pattern. In the pleura, mesentery, and peritoneum or the liver, extraosseous multiple myelomas may manifest as infiltrative soft tissue lesions. The lesions frequently appear as enhancing soft-tissue lesions or masses with early enhancement and delayed washout on dynamic CT scans or dynamic MR images. The lesions show an isointense signal on T1-weighted MR images and a hyperintense signal on T2-weighted images. FDG PET plays a limited role in the evaluation of extraosseous involvement of myeloma because the lesions show variable FDG uptake.
Figures and Tables
Fig. 1
Biopsy-proven plasmacytoma in the oropharynx of a 76-year-old man with IgG multiple myeloma. A contrast enhanced CT scan at the level of the tongue base shows a homogenous, well-enhancing, soft-tissue mass (arrows) in the anterior wall of oropharynx.
Fig. 2
An ocular myeloma in a 60-year-old man with extensive systemic manifestation of IgM multiple myeloma.
A, B. T1-weighted (A) and T2-weighted (B) MR images show an iso-signal intensity lesion (arrows) in the right eye orbit.
C. A contrast-enhanced T1-weighted MR image demonstrates homogenous enhancement (arrow) of the lesion.

Fig. 3
Cavernous sinus κlight-chain myeloma in a 58-year-old woman. A contrast enhanced T1-weighted MR image shows a newly developed soft-tissue nodule (arrow) in the left cavernous sinus. The lesion was absent on MR images obtained one year ago. CSF analysis revealed atypical plasmacytoid cells.
Fig. 4
Pulmonary κlight-chain myelomas in a 58-year-old woman.
A, B. Conventional CT images (5.0-mm-section thickness) obtained at the levels of thoracic inlet (A) and bronchus intermedius (B), respectively, show multiple variable sized lung nodules (arrows) scattered in both lungs. Lung lesions were considered to infer lung involvement of multiple myeloma due to the absence of signs of infection and regression after chemotherapy (not shown here). Small amounts of bilateral pleural effusions were also seen. Plasma cells were identified in a pleural fluid analysis.

Fig. 5
Pleural IgM myeloma in a 60-year-old man. Enhanced CT scan (2.5-mm-section thickness) obtained at the atrial level shows bilateral pleural effusions. Also note the multifocal areas of pleural thickening and mass-like lesions (arrows).

Fig. 6
Biopsy-proven mediastinal λlight-chain myeloma in a 45-year-old man.
A. Chest radiograph shows bilateral mediastinal widening (arrows).
B. A contrast-enhanced CT scan (2.5-mm-section thickness) obtained at the level of the main bronchi demonstrates a large bilateral anterior mediastinal mass that shows mild enhancement. Small amounts of bilateral pleural effusions, small in amount are also associated. A surgical biopsy specimen revealed a myelomatous lesion. (Min JH, et al. J Korean Soc Radiol 2010;62:365-368, with permission)
Fig. 7
Biopsy-proven mediastinal IgD myeloma in a 60-year-old man.
A. A contrast-enhanced CT scan (5.0-mm-section thickness) obtained at the level of the azygos arch shows an enhancing left anterior mediastinal mass (arrow).
B. PET scan obtained at a similar level to a demonstrates little FDG uptake within the lesion. After chemotherapy, the left anterior mediastinal mass disappeared (not shown here).

Fig. 8
Biopsy-proven hepatic λlight-chain myelomas in a 49-year-old woman who is a hepatitis-B virus carrier.
A. Ultrasonography of the liver shows multiple hypoechoic nodules (arrows) in both lobes of the liver.
B, C. Enhanced liver CT scans obtained at the levels of the liver dome (B) and hepatic veins (C), respectively, and in the portal phase, show enhancing small hepatic nodules (arrows) in both lobes of the liver.
D. T2-weighted MR image shows multiple hyperintense nodular lesions (arrows) in the liver.
E. Dynamic MR images obtained after the injection of gadoxetic acid show multiple nodules in the liver. The nodules show enhancement at the arterial phase (A) and washout in both the equilibrium (E) and hepatobiliary (H) phases.

Fig. 9
Biopsy-proven hepatic IgD myelomas in 69-year-old man.
A. An enhanced whole-body MR image shows iso- to slightly high-signal intensity lesions (arrows, osseous involvement of myeloma) in the right proximal and distal tibia. Also noted is a round lesion (arrowhead) in the liver with slightly lower-signal intensity than normal liver. The hepatic lesion showed early arterial enhancement and delayed washout on dynamic MR images as in Figure 8 (not shown here).
B. A PET scan does not show any evidence of FDG uptake either in bone lesions in the right tibia or in the liver lesion.

Fig. 10
Renal involvement of λlight-chain myeloma in a 49-year-old woman. Newly developed multifocal low-attenuation lesions (arrows) are observed in both kidneys on delayed-phase CT images. Patients had such renal lesions on regular follow-up CT studies after the complete remission of multiple myeloma.
Fig. 11
Mesenteric IgG and λlight-chain myeloma in a 51-year-old woman. Contrast enhanced CT scan (5.0-mm-section thickness) shows a large mass lesion (arrows) within the mesenteries. The lesion harbors a central necrotic portion, and entraps the superior mesenteric vessels. Plasmacytoma was histopathologically confirmed.
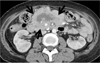
Fig. 12
Retroperitoneal IgG and κlight-chain myeloma in a 68-year-old woman. A contrast-enhanced CT scan (5.0-mm-section thickness) shows a highly enhancing infiltrative mass (arrows) in the presacral and right parapelvic areas. A double-J catheter (arrowhead) was inserted into the right ureter, owing to its invasion by the mass.
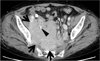
Fig. 13
Lymph node involvement of λlight-chain myeloma in a 49-year-old woman. A contrast-enhanced CT scan (5.0-mm-section thickness) obtained at the level of porta hepatis shows enlarged lymph nodes (arrows) around the caudate lobe of the liver and splenic artery, respectively. The lesions were absent on CT scans (not shown here) taken two years ago.
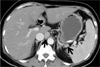
Fig. 14
Psoas muscle κlight-chain myeloma in a 48-year-old woman. A contrast enhanced CT scan (5.0-mm-section thickness obtained at the level of pelvic inlet shows a heterogeneously enhancing mass lesion (arrows) in the right psoas muscle. Also note a smaller enhancing lesion (arrowhead) in the right iliacus muscle area.

Fig. 15
Breast IgG and κlight-chain myeloma in a 65-year-old woman.
A. Mediolateral oblique view of mammography shows a well-circumscribed hyperdense mass (arrow) in the upper central portion of the right breast.
B. Ultrasonography of right breast shows a heterogeneous low-echoic mass (arrows) in the corresponding mammographic area.

References
1. Varettoni M, Corso A, Pica G, Mangiacavalli S, Pascutto C, Lazzarino M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol. 2010; 21:325–330.
2. Moulopoulos LA, Granfield CA, Dimopoulos MA, Kim EE, Alexanian R, Libshitz HI. Extraosseous multiple myeloma: imaging features. AJR Am J Roentgenol. 1993; 161:1083–1087.
3. Patlas M, Hadas-Halpern I, Libson E. Imaging findings of extraosseous multiple myeloma. Cancer Imaging. 2002; 2:120–122.
4. Hall MN, Jagannathan JP, Ramaiya NH, Shinagare AB, Van den Abbeele AD. Imaging of extraosseous myeloma: CT, PET/CT, and MRI features. AJR Am J Roentgenol. 2010; 195:1057–1065.
5. Damaj G, Mohty M, Vey N, Dincan E, Bouabdallah R, Faucher C, et al. Features of extramedullary and extraosseous multiple myeloma: a report of 19 patients from a single center. Eur J Haematol. 2004; 73:402–406.
6. Patriarca F, Zaja F, Silvestri F, Sperotto A, Scalise A, Gigli G, et al. Meningeal and cerebral involvement in multiple myeloma patients. Ann Hematol. 2001; 80:758–762.
7. Masood A, Hudhud KH, Hegazi A, Syed G. Mediastinal plasmacytoma with multiple myeloma presenting as a diagnostic dilemma. Cases J. 2008; 1:116.
8. Patlas M, Khalili K, Dill-Macky MJ, Wilson SR. Spectrum of imaging findings in abdominal extraosseous myeloma. AJR Am J Roentgenol. 2004; 183:929–932.
9. Goh J, Otridge B, Brady H, Breatnach E, Dervan P, MacMathuna P. Aggressive multiple myeloma presenting as mesenteric panniculitis. Am J Gastroenterol. 2001; 96:238–241.
10. Oshima K, Kanda Y, Nannya Y, Kaneko M, Hamaki T, Suguro M, et al. Clinical and pathologic findings in 52 consecutively autopsied cases with multiple myeloma. Am J Hematol. 2001; 67:1–5.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download